Abstract
As the need for accurate diagnostic imaging often continues throughout a cancer survivor’s life, imaging methods with the least toxicity must be used so as to provide needed information without contributing to long-term sequelae that might compound toxicities inherent with the primary disease and its treatment. In this regard, the costs, benefits and potential risks of post-therapy monitoring for disease recurrence warrant periodic review. Unfortunately, few analyses are available regarding the impact of surveillance imaging on the detection of disease recurrence, salvage rates of relapse disease and long-term survival outcomes for pediatric cancer survivors. This review will examine the role and limitations of surveillance imaging in pediatric oncology.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Diagnostic imaging provides information critical to patient care, detection of disease and treatment-related toxicity, monitoring of disease response to therapy, and designing of clinical protocols. The dramatic advances in imaging technology coupled with the development of new drug therapies, tumor-specific treatment regimens, and improved surgical and refined radiation oncological techniques have led to a rapidly growing cohort of survivors of childhood cancer. In the United States alone, the number of survivors is estimated to approach 330,000 [1]. Thus, the potential impact of imaging monitoring and imaging-induced patient exposures to ionizing radiation is growing. This issue is of particular concern in this increasing population of young people who undergo prolonged and repeated imaging.
This paper will discuss surveillance imaging in pediatric oncology, its roles and limitations, and briefly review the available literature as it relates to pediatric oncology.
Roles of surveillance imaging
Imaging plays a key role in the diagnosis, staging and monitoring of treatment response. Not always appreciated, however, is the ongoing use of diagnostic imaging for several years after treatment completion to detect disease recurrence, disease progression and development of second malignancies [2–6]. The strategies of such regimens—frequency, modality, duration—vary widely among institutions, diagnoses and cooperative groups [7, 8].
In addition to disease detection and monitoring, diagnostic imaging is critical to the identification of late effects of therapy. Thus, as the need for accurate diagnostic imaging often continues throughout the patient’s life. Imaging methods with the least toxicity are of growing importance and must be used so as to provide needed information without contributing to long-term sequelae that might compound toxicity inherent with the primary disease and its treatment. In this regard, the costs, benefits and potential risks of post-therapy monitoring for disease recurrence warrant periodic review. Unfortunately, few analyses of the impact of surveillance imaging on the detection of disease recurrence, salvage rates of relapse disease and long-term survival outcomes are available, particularly for pediatric cancer survivors [9, 10].
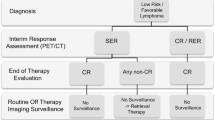
Monitoring varies widely with primary diagnosis and patient demographics at diagnosis (such as age, gender, race, genetic risk), treatment exposures, etc. Surveillance imaging for detection of disease recurrence might identify relapse before clinical symptoms develop [11]. The rate of salvage is partially dependent upon tumor type and grade and partly upon tumor burden at the time of relapse [12, 13]. Intuitively, for some tumors, the earlier detection would be expected to contribute to improved salvage rates. However, for some diseases such as sarcoma, Hodgkin disease [14–16] and others [12], detection of recurrence prior to development of symptoms has not improved salvage.
The usefulness of ongoing surveillance imaging remains controversial [9, 12, 13, 17] Chong et al. [18] recently reported on the radiation exposure burden placed on survivors of various cancers. Five-year cumulative estimates of individual radiation exposures were calculated to range from 10 mSv to 642 mSv (median, 61 mSv) resulting from 690 imaging procedures. Of these, only 34% of studies were protocol-driven; the remaining studies were optional procedures nearly evenly divided between those for clinical care and surveillance studies. These investigators found that children treated for neuroblastoma had the highest median cumulative exposure to ionizing radiation (214 mSv) but also found that patients treated for lymphoma bore a considerably greater burden (median cumulative exposure of 61 mSv) than patients treated for other malignancies [18].
In addition to detection of disease relapse, surveillance imaging might be directed toward identification of second malignant neoplasms [19] and late toxicities [20, 21] resulting from the primary disease and its treatment. However, the reported prevalence and severity of detected involvement varies widely because of inconsistent methods of detection [22]. One example is monitoring for osteonecrosis (ON). ON is reported to be one of the most common treatment-associated toxicities in patients treated for acute lymphoblastic leukemia (ALL) [23–26]. The Children’s Oncology Group (COG) has developed extensive risk- and disease-specific evidence-based long-term follow-up guidelines for ALL that incorporate clinical, laboratory and imaging assessments [27].
Need for outcomes analysis of surveillance imaging studies
Technology advances more rapidly than our ability to fully assess its clinical utility. Not uncommonly, new imaging modalities are incorporated into clinical trials prior to full investigation of their impact on clinical management of diseases. Few modality-specific outcomes publications are available. It falls within our responsibility as imagers and collaborators in study designs to engage the oncological community and direct assessment of the sensitivity and specificity of a given modality, its frequency of use and impact on tumor response assessments. Only through such analyses can we minimize radiation exposures, optimize disease detection and monitoring, and impact resource utilization.
In order to determine the timing of surveillance that will maximize detection while minimizing excessive imaging-associated exposures, analysis of historical data related to risk factors associated with relapse, the time to relapse and method(s) by which relapse was or was not detected must be analyzed [8].
Limited investigations reveal an overall lack of consensus regarding the timing and utility of post-therapy surveillance imaging. Lee et al. [9], focusing their retrospective analysis on nearly 200 adult patients in first remission after being treated for classic Hodgkin disease, found surveillance imaging detected 12 cases of recurrent Hodgkin disease and four cases of second malignant neoplasms. The positive predictive value of CT and PET-CT were not significantly different (P = 0.73; 28.6% and 22.9%, respectively). Further, they estimated the cost to detect a single event to be $100,000 with radiation exposures of 146.6 mSv per patient [5]. Other studies investigating the use of surveillance CTs in detecting relapse adult lymphomas have reported similar results [14–16, 28, 29].
In an additional retrospective study of more than 700 children in first complete remission from a variety of malignancies, Biasotti et al. [12] found the median age to relapse being 12 months (range, 3–87 months). Of the 739 patients who completed therapy, six developed a second malignant tumor and 173 developed relapse of their primary disease. Seventy-five percent of relapses were suspected clinically, 16% were identified by imaging and 9% by laboratory results. They further pointed out that routine scheduled surveillance appointments failed to detect half of the relapse cases they report [12]. Similarly, Howell et al. [17] reported 37 recurrences of solid tumors in a cohort of 186 pediatric patients followed for a median of almost 6 years. More than half of the recurrences were symptomatic. They further estimated that for every recurrence, 42 routine MR examinations, 129 CT examinations and 257 chest radiographs were performed [17].
In contrast to the above examples, a review of nearly 300 cases of relapse of malignant glioma, medulloblastoma and ependymoma in pediatric patients treated on one of 10 Pediatric Oncology Group (POG) protocols found that nearly one-third (99/291) of relapses were detected by surveillance imaging; 192/291 were detected clinically [8]. However, other investigators found that a multidisciplinary clinical evaluation was a sensitive means for detecting recurrence of brain tumors and thus raised the question of the utility of routine imaging surveillance [30].
Not only must the potential impact of repeated exposures to ionizing radiation be considered [31–37] but also the potential impact of repeated contrast administration, anesthesia risks [8, 38], costs of time, resources and funds [8, 9, 11, 17] and the impact of false-positive and false-negative findings.
Future considerations
Refinement of US and MR techniques to maximize information obtained and expand their use in surveillance would obviate patient exposure to ionizing radiation. Current investigations into the technical aspects and value of whole-body MR indicate that such imaging can play a valuable role in the care of children [39–41]. As drug therapies are developed, additional potentially unseen challenges will require further reassessment and modification of surveillance imaging as well as development of specialized imaging techniques. Targeted surveillance imaging for patients treated with targeted therapy might prompt refinement of imaging needs. New imaging modalities—functional imaging, biological imaging, etc.—will be incorporated into developing treatment regimens but their roles and efficacy at specific treatment time points must be assessed with an ongoing trials-based approach.
Conclusion
Of the few outcomes studies evaluating routine surveillance imaging in detecting disease relapse after completion of therapy for pediatric cancers, most indicate little if any significant improvement in salvage rates between relapse detected by imaging and that by clinical suspicions. The role of surveillance imaging, laboratory investigation and clinical examination for detecting toxicities as reported in the COG long-term follow-up guidelines is based upon hypothesis-driven publications and undergoes continuous review [27].
As pediatric radiologists, we must develop the most sensitive, specific and innovative methods of anatomical and functional imaging for longitudinally determining tumor response to therapy, detecting tumor recurrence and detecting second malignant neoplasms and late affects resulting from disease and its therapy. To contribute optimally to study designs and the use of diagnostic imaging tools, we must be abreast of new disease-specific, patient-specific and risk-adapted protocols in the design of imaging surveillance. These aspects must all be considered in the context of optimizing cure and identifying and minimizing adverse toxicities related to medical imaging, recognizing the growing survivorship and directing the utilization of resources. Our contributions to the care of these young patients must adhere to the dictum of “As Low As Reasonably Achievable” (ALARA).
References
Mariotto AB, Rowland JH, Yabroff KR et al (2009) Long-term survivors of childhood cancers in the United States. Cancer Epidemiol Biomarkers Prev 18:1033–1040
Bhatia S, Yasui Y, Robison LL et al (2003) High risk of subsequent neoplasms continues with extended follow-up of childhood Hodgkin’s disease: report from the Late Effects Study Group. J Clin Oncol 21:4386–4394
Bhatti P, Veiga LH, Ronckers CX et al (2010) Risk of second primary thyroid cancer after radiotherapy for a childhood cancer in a large cohort study: an update from the childhood cancer survivor study. Radiat Res 174:741–752
Inskip PD, Curtis RE (2007) New malignancies following childhood cancer in the United States, 1973–2002. Int J Cancer 121:2233–2240
Reaman GH (2009) What, why, and when we image: considerations for diagnostic imaging and clinical research in the Children’s Oncology Group. Pediatr Radiol 39(Suppl 1):S42–S45
Meadows AT, Friedman DL, Neglia JP et al (2009) Second neoplasms in survivors of childhood cancer: findings from the childhood cancer survivor study cohort. J Clin Oncol 27:2356–2362
Bowers DC, Adhikari S, El-Khashab YM et al (2009) Survey of long-term follow-up programs in the United States for survivors of childhood brain tumors. Pediatr Blood Cancer 53:1295–1301
Minn AY, Pollock BH, Garzarella L et al (2001) Surveillance neuroimaging to detect relapse in childhood brain tumors: a pediatric oncology group study. J Clin Oncol 19:4135–4140
Lee AI, Zuckerman DS, Van den Abbeele AD et al (2010) Surveillance imaging of Hodgkin lymphoma patients in first remission: a clinical and economic analysis. Cancer 116:3835–3842
Postovsky S, Barzilai M, Meller I et al (2008) Does regular follow-up influence the survival of patients with sarcoma after recurrence? The Miri Shitrit pediatric oncology department experience. J Pediatr Hematol Oncol 30:189–195
Kovanlikaya A, Karabay N, Cakmakci H et al (2003) Surveillance imaging and cost effectivity in pediatric brain tumors. Eur J Radiol 47:188–192
Biasotti S, Garaventa A, Padovani P et al (2005) Role of active follow-up for early diagnosis of relapse after elective end of therapies. Pediatr Blood Cancer 45:781–786
Owens CM, Brisse HJ, Olsen OE et al (2008) Bilateral disease and new trends in Wilms tumour. Pediatr Radiol 38:30–39
Guadagnolo BA, Punglia RS, Kuntz KM et al (2006) Cost-effectiveness analysis of computerized tomography in the routine follow-up of patients after primary treatment for Hodgkin’s disease. J Clin Oncol 24:4116–4122
Torrey MJ, Poen JC, Hoppe RT (1997) Detection of relapse in early-stage Hodgkin’s disease: role of routine follow-up studies. J Clin Oncol 15:1123–1130
Dryver ET, Jernstrom H, Tompkins K et al (2003) Follow-up of patients with Hodgkin’s disease following curative treatment: the routine CT scan is of little value. Br J Cancer 89:482–486
Howell L, Mensah A, Brennan B et al (2005) Detection of recurrence in childhood solid tumors. Cancer 103:1274–1279
Chong AL, Grant RM, Ahmed BA et al (2010) Imaging in pediatric patients: time to think again about surveillance. Pediatr Blood Cancer 55:407–413
Nathan PC, Ness KK, Mahoney MC et al (2010) Screening and surveillance for second malignant neoplasms in adult survivors of childhood cancer: a report from the childhood cancer survivor study. Ann Intern Med 153:442–451
Meadows AT (2003) Pediatric cancer survivors: Past history and future challenges. Curr Probl Cancer 27:112–126
Hudson MM, Mulrooney DA, Bowers DC et al (2009) High-risk populations identified in childhood cancer survivor study investigations: implications for risk-based surveillance. J Clin Oncol 27:2405–2414
Kaste SC (2008) Skeletal toxicities of treatment in children with cancer. Pediatr Blood Cancer 50(2 Suppl):469–473
Karimova EJ, Rai SN, Ingle D et al (2006) MRI of knee osteonecrosis in children with leukemia and lymphoma: Part 2, clinical and imaging patterns. AJR 186:477–482
LA Mattano J, Sather HN, Trigg ME et al (2000) Osteonecrosis as a complication of treating acute lymphoblastic leukemia in children: a report from the children’s cancer group. J Clin Oncol 18:3262–3272
Sala A, Mattano LA Jr, Barr RD (2007) Osteonecrosis in children and adolescents with cancer—an adverse effect of systemic therapy. Eur J Cancer 43:683–689
Barr RD, Sala A (2008) Osteonecrosis in children and adolescents with cancer. Pediatr Blood Cancer 50(2 Suppl):483–485
Children’s Oncology Group (2008) Long-term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers. Available via www.survivorshipguidelines.org. Accessed 07 March 2011
Guppy AE, Tebbutt NC, Norman A et al (2003) The role of surveillance CT scans in patients with diffuse large B-cell non-Hodgkin’s lymphoma. Leuk Lymphoma 44:123–125
Elis A, Blickstein D, Klein O et al (2002) Detection of relapse in non-Hodgkin’s lymphoma: role of routine follow-up studies. Am J Hematol 69:41–44
de Graaf N, Hew JM, Fock JM et al (2002) Predictive value of clinical evaluation in the follow-up of children with a brain tumor. Med Pediatr Oncol 38:254–257
Ron E (2003) Cancer risks from medical radiation. Health Phys 85:47–59
Frush DP, Goske MJ, Hernanz-Schulman M (2008) Computed tomography and radiation exposure. N Engl J Med 358:851–853
Frush DP (2009) Radiation, CT, and children: the simple answer is … it’s complicated. Radiology 252:4–6
Brenner D, Elliston C, Hall E et al (2001) Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR 176:289–296
Huda W (2004) Assessment of the problem: pediatric doses in screen-film and digital radiography. Pediatr Radiol 34(Suppl 3):S173–S182
Huda W (2007) Radiation doses and risks in chest computed tomography examinations. Proc Am Thorac Soc 4:316–320
Brody AS, Frush DP, Huda W et al (2007) Radiation risk to children from computed tomography. Pediatrics 120:677–682
Girshin M, Shapiro V, Rhee A et al (2009) Increased risk of general anesthesia for high-risk patients undergoing magnetic resonance imaging. J Comput Assist Tomogr 33:312–315
Kwee TC, Takahara T, Luijten PR et al (2010) ADC measurements of lymph nodes: inter- and intra-observer reproducibility study and an overview of the literature. Eur J Radiol 75:215–220
Ley S, Ley-Zaporozhan J, Schenk JP (2009) Whole-body MRI in the pediatric patient. Eur J Radiol 70:442–451
Darge K, Jaramillo D, Siegel MJ (2008) Whole-body MRI in children: current status and future applications. Eur J Radiol 68:289–298
Acknowledgement
We thank Ms. Sandra Gaither for manuscript preparation.
Disclaimer
The supplement this article is part of is not sponsored by the industry. Dr. Kaste discloses that this work is supported in part by grants P30 CA-21765 from the National Institutes of Health, a Center of Excellence grant from the State of Tennessee, and the American Lebanese Syrian Associated Charities (ALSAC).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kaste, S.C. Oncological imaging: tumor surveillance in children. Pediatr Radiol 41 (Suppl 2), 505 (2011). https://doi.org/10.1007/s00247-011-2108-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00247-011-2108-1