Abstract
Successful management of hydronephrosis in the newborn requires early accurate diagnosis to identify or exclude ureteropelvic junction obstruction. However, the presence of hydronephrosis does not define obstruction and displays unique behavior in the newborn. The hydronephrotic kidney usually has nearly normal differential renal function at birth, has not been subjected to progressive dilation and except for pelvocaliectasis does not often show signs of high-grade obstruction. Furthermore, severe hydronephrosis resolves spontaneously in more than 65% of newborns with differential renal function stable or improving. The diagnosis of obstruction in newborn hydronephrosis is challenging because the currently available diagnostic tests, ultrasonography and diuretic renography have demonstrated inaccuracy in diagnosing obstruction and predicting which hydronephrotic kidney will undergo deterioration if untreated. Accurate diagnosis of obstruction is possible but it requires an understanding of the uniqueness of both the pathophysiology of obstruction and the biology of the kidney and renal collecting system in this age group. We examine here the requirements for making an accurate diagnosis of obstruction in the young child with hydronephrosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hydronephrosis in the fetus occurs commonly and its persistence in the newborn presents the dual diagnostic challenges of trying to determine whether obstruction exists and whether the kidney is at risk of renal injury and in need of surgical intervention. Nearly 20 years ago when ultrasonography (US) was introduced and applied to a near epidemic of fetal and newborn hydronephrosis, these determinations were invariably answered with a “yes,” and almost all infants with prominent hydronephrosis were thought to be obstructed and in need of early surgical repair [1].
Since then additional investigative modalities such as diuretic renography (DR), with measurement of washout pattern and differential function, have been applied to this diagnostic conundrum in an attempt to refine the diagnosis and management of obstruction and hydronephrosis in this age group. Unfortunately, after 10–15 years of study of the natural history of postnatal hydronephrosis followed nonoperatively no gold standard for obstruction has emerged, and it has become apparent that in the majority of children (>65–75%), marked unilateral hydronephrosis of the ureteropelvic junction (UPJ) type resolves over time without renal injury. These kidneys were not obstructed at birth and do not benefit from surgery despite their initial appearances and test results (DR and US) and the fact that urologists invariably find kinks, narrowings and other assorted abnormalities at the UPJ at the time of surgery that appear obstructive and appear to justify the operative intervention. Had initial surgery been performed instead of nonoperative observation, the “surgical results” would have been outstandingly successful, and the postoperative improvement would have reinforced the misdiagnosis of obstruction and the need for unnecessary surgery [2–7].
It is in this setting that magnetic resonance urography (MRU) has been offered as a potentially better diagnostic tool for assessing obstruction in hydronephrosis. Because one of the purposes of this Workshop on MRU in Children is to determine the role of MRU in the diagnosis of obstruction, it is appropriate to discuss the requirements for making a diagnosis of obstruction in young children with hydronephrosis with a focus on problem areas that can and cannot be solved with MRU.
The pathophysiology of chronic partial upper urinary tract obstruction
Chronic partial upper urinary tract obstruction (CPUUTO) is the common form of problematic obstruction in young children and is of great clinical concern because it is often difficult to diagnose and untreated can progressively damage the kidney. It must be distinguished from total obstruction, which causes little diagnostic confusion because it is rapidly injurious and often destroys the kidney prior to or soon after birth. Although hydronephrosis is an easy-to-recognize consequence of partial obstruction, it lacks diagnostic specificity because it can be the result of nonobstructive conditions such as reflux or developmental malformation. Uniquely, CPUUTO is an extremely difficult form of obstruction to characterize physiologically, because the parameters that usually define obstruction in other organ systems, i.e. pressure and flow, are not component features in its diagnosis [8].
Renal pelvic pressure is usually normal in CPUUTO. If it were not normal then the diagnosis of chronic partial obstruction would be very easy indeed. One would simply place a needle in the renal pelvis and note the elevated pressure. Whitaker test would never have needed to be invented.
Renal pelvic volume (size) increases in CPUUTO but, puzzlingly, it often stabilizes and does not enlarge further.
The outflow rate across the UPJ is normal in CPUUTO and at almost all times is the same as the inflow rate. Were it less for any length of time, even if it were reduced by only a small amount, the renal pelvis would expand rapidly by this differential rate because of the enormous amount of renal blood flow, and would over-distend rapidly.
In the face of all these normal measurements, the pathophysiology of hydronephrosis appears to be genuinely puzzling, and one must ponder the seemingly simplistic question:
If pelvic pressure is normal in CPUUTO, why does the renal pelvis not just shrink to a smaller volume?
The answer to this seemingly simple query requires an understanding of the pathophysiology of CPUUTO and the concepts of equilibrium as well as the beneficial and protective effects of hydronephrosis that are best seen in the behavior of a partially obstructed kidney in an animal model. When an incompletely occluding ligature is placed just below the UPJ in dogs [9, 10], pelvic volume is observed to increase initially as expected (Fig. 1) but thereafter some pelves reach equilibrium and enlarge no further while the volume of others decreases (Fig. 2). The elevated pressures in the renal pelvis seen immediately after creation of obstruction likewise decrease progressively over time to normalize after several weeks (Fig. 3). The protective effect of hydronephrosis can be seen in a one-kidney canine model in which nephrectomy and creation of contralateral partial obstruction occurs simultaneously, after which changes in renal function, measured by serum creatinine (a reasonably accurate reflection of solitary kidney function in a one-kidney model) and pelvic volume, are observed over time (Fig. 4). Creatinine remains fairly stable despite a partial UPJ obstruction that is significant enough to cause progressive hydronephrosis exceeding 80 ml (normal ≤ 3 ml). After release of obstruction, pelvic volume returns toward normal but renal function remains unaffected. It appears as if the hydronephrosis has protected the renal parenchyma from functional deterioration even in the presence of a significant partial UPJ obstruction. However, not all kidneys subjected to the same degree of partial UPJ obstruction will be protected. In some cases even a large pelvic volume will not confer protection from progressive renal functional deterioration (Fig. 5).
These observations suggest that hydronephrosis induced by partial UPJ obstruction permits the same degree of obstruction to cause progressive dilation of the pelvis and renal impairment of renal function at low pelvic volumes but not at high pelvic volumes. How the partially obstructed hydronephrotic kidney exerts beneficial and protective effects requires further analysis.
Determinants of progression and equilibrium in hydronephrosis
Once a partial obstruction is created the factors that determine whether the dilation will progress or equilibrate are multiple and interrelated. They include the volume and health of the renal parenchyma, amount of urine produced, physical properties of the renal pelvis and, of course, the tightness of the obstruction. Of these, the behavior and physical properties of the renal pelvis, its compliance, contractility and capacity have received scant attention, yet might well be the most important factors in determining the fate of the partially obstructed kidney.
The physical properties of the renal pelvis have been assessed experimentally by pelvimetric examination, which defines pelvic pressure–volume relationships during filling [8, 11, 12]. This study is similar to a cystometric examination and involves filling the renal pelvis with fluid at a constant rate while monitoring changes in pelvic pressure during temporary atraumatic occlusion of the UPJ. A typical pelvimetric curve has a characteristic shape that is similar to a cystometric tracing (Fig. 6). It is composed of a slowly rising low-pressure filling or accommodation phase during which the pelvic smooth muscle relaxes to accommodate increasing volume. This is followed by a more rapidly rising overdistension phase, during which the smooth muscle exceeds its relaxation potential and the tracing reflects overstretching of elastic and connective (viscoelastic) tissues within the pelvic wall. The transition point between these phases defines the physiological capacity volume (VC) of the renal pelvis, an inflection point that is usually easily identified. Below VC, pressures are generally within the normal range and do not exceed 20 cm water. Above VC, pressures rise rapidly to quickly reach levels that are potentially damaging to the kidney. The slope of the overdistension phase can be measured as dP/dV (Fig. 6).
The pressure–volume relationships that occur during progressive hydronephrosis in partially obstructed kidneys have been studied and characterized experimentally and clinically by initially creating a partially obstructing ligature around the upper ureter, and then serially performing pelvimetric studies during progressive dilation and then after release of obstruction [8, 11, 12]. Study of many normal and obstructed hydronephrotic kidneys as well as hydronephrotic kidneys no longer obstructed after release of obstruction have revealed a very similarly shaped pelvimetric curve with the inflection point defining VC easily recognizable (Fig. 6).
As hydronephrosis progresses and the renal pelvis enlarges the curves serially evolve to reflect two distinct events that are simultaneously occurring: the slope of the overdistension curve decreases, and VC increases. Together, these two factors influence to a great extent the behavior and prognosis of the partially obstructed hydronephrotic kidney. As hydronephrosis progresses, the larger VC reflects a greater reservoir capacity, which increasingly functions as a volume buffer to protect the pelvis from reaching the overdistension phase. Likewise, a decreasing slope of the overdistension curve implies that pressures in the pelvis will rise at a slower rate and not reach as high as the pelvis fills even if overstretching of the pelvis occurs as a result of exceeding VC. Depending on the rate and extent of volume expansion, these factors can delay, mitigate or even prevent altogether the pressure within the pelvis from reaching levels that can induce renal parenchymal damage (Fig. 7).
The clinical implications of these physiological phenomena are significant. They explain how pressures rise faster and reach higher levels in kidneys with small renal pelves than large pelves. This is the reason that kidneys with small or intrarenal pelves are more vulnerable to obstruction than kidneys with large or extrarenal pelves. Also explained is why the presence of infection in the obstructed hydronephrotic kidney magnifies renal injury by causing the pelvis to thicken, lose its compliance and elasticity and develop higher pressures more rapidly. Finally, these mechanisms also explain how the renal pelvis is able to maintain a state of hydronephrotic dilation despite normal pressures and provide an answer to the following question:
Why does the partially obstructed hydronephrotic kidney not shrink to a more normal pelvic size when pelvic pressure is normal?
The answer to this seemingly simple question provides a key to understanding the pathophysiology of progressive hydronephrosis in partial UPJ obstruction. Intermittent diuresis is a driving force for progression of hydronephrosis, and two physical properties of the renal pelvis determine its fate. They are: (1) hysteresis, a mechanical property by which the force needed to create a deformation is always greater than the force needed to maintain that deformation, and (2) stress relaxation, an attribute of the pelvic wall that enables it to slowly enlarge or creep under stress, rather than to tear or disrupt.
It is important to recognize that in chronic partial obstruction the hydronephrotic renal pelvis is rarely overdistended. Pelvic volumes vary and depend on the state of hydration and urine production. The instigating event in progressive hydronephrosis appears to be a temporary imbalance between urine production into the pelvis and urine outflow from the pelvis. With extrinsic obstructions, the imbalance occurs during pelvis volume expansion as a result of an aberrant vessel or band that compresses or kinks the UPJ to increase its resistance. In contrast, for intrinsic UPJ obstructions that fix or decrease the luminal caliber of the UPJ and prevent it from dilating during peristalsis, the imbalance occurs during diuresis. In either case, the result of imbalance between inflow and outflow is pelvic volume expansion. As the pelvis enlarges, its pressure is determined by the particular pelvimetric relationship that exists at that point in time. During volume expansion, pathological pressures generally do not develop and are not sustained as long as the pelvic smooth muscle relaxes sufficiently to accommodate the increased volume. However, once the pelvis expands beyond this point, overstretching will lead to progression of hydronephrosis [13–15].
Physiologically, the overstretched pelvis will produce pathologically high pressures that can adversely affect renal function. The most obvious functional change will be a decrease in urine production, which can cease altogether if pressures get too high. Once urine production decreases or stops, the pelvis will stop enlarging and will eventually begin to decrease in size as urine flows out across the UPJ and through alternative lymphatic and tubular backflow channels. However, if the overdistension has altered the integrity of the pelvic wall, then progression of hydronephrosis will occur because once the pelvis enlarges beyond its accommodative limits and the viscoelastic tissues stretch under stress they will be deformed to a new maximum volume. This will reset the pressure–volume relationships within the pelvis and will shift the pelvimetric curve to the right (Fig. 8). The consequence of this will be that at each and every increment of pelvic volume the pressure within the pelvis will be slightly less than before. This reflects hysteresis: it took excessive pressure (force) to overstretch and enlarge the pelvis, but it now takes less pressure (force) to maintain the enlarged pelvis in its new slightly overstretched state. The new pelvimetric curve relationships determine the pressure that exists at each and every increment of pelvic volume (Fig. 8). The answer to the above query becomes apparent: the pelvis does not shrink to a normal size when pressures are normal because pressure does not determine volume within the renal pelvis. Rather, pressure is determined by volume in the pelvis according to the pressure–volume pelvimetric relationship in the pelvis; pressure at each increment of volume reflects the smooth muscle and viscoelastic properties of the pelvis wall.
Figure 8 reveals the pressure–volume relationships in an expanding partially obstructed hydronephrotic kidney and it displays a series of pelvimetric curves. Each curve reflects a pressure–volume relationship that remains constant until the next episode of pelvic overdistension. In essence, the process of hydronephrotic expansion in CPUUTO involves a series of small episodes of renal pelvic overdistension that can be viewed as intermittent acute obstructions. Not all diuretic or obstructive episodes will be of sufficient duration or degree to produce overdistension, but when overstretching does occur it will shift the pelvimetric curve to the right and cause progression of hydronephrosis.
Despite the pathophysiology and consequences of the obstructive events required to create progressive hydronephrosis, hydronephrosis per se should not be viewed as pathological or harmful. It is actually protective, and its salutary effects are seen when the pelvimetric curve is examined more carefully. Figure 3 illustrates that partial obstruction initially causes high and potentially damaging pelvic pressures. But, with increasing hydronephrosis, the maximum pressures within the partially obstructed (canine) kidney decrease toward normal and after about 6–10 weeks remain within the normal range. This is because the enlarged renal pelvis now has a larger maximum capacity and can take in significantly more urine volume before pelvic overdistension occurs. In addition, the rate at which pressures rise within the pelvis is less than before because the slope of the overdistension curve has decreased. This implies that a longer period of imbalance between inflow and outflow will be tolerated before the pelvis exceeds its accommodative limit and before pressures reach pathological levels; theoretically, if the pelvis enlarges sufficiently, pressures will never become pathologically high.
Taken together, the biological changes occurring in the hydronephrotic renal pelvis are compensating mechanisms that enable it to become large enough to reduce the likelihood of further pelvic overdistension, and when overdistension occurs they blunt the pelvic pressure rise to reduce or prevent damaging elevations. As a result, when the pelvis is extremely compliant and stretchy as exists in the newborn, hydronephrosis actually might prevent any renal damage from occurring by keeping pressures low. These beneficial effects might be reflected in relatively normal levels of differential renal function seen in hydronephrotic newborn kidneys and in the surprisingly benign behavior of these kidneys observed in natural history studies of untreated hydronephrosis.
Natural history of newborn hydronephrosis
Studies in which children with severe newborn hydronephrosis were observed without any form of surgical or radiological therapeutic intervention are uncommon but do exist. They reveal that about 65–75% of hydronephrotic kidneys are not obstructed and will demonstrate resolution or marked improvement in hydronephrosis without deterioration of renal function provided they are followed at close intervals and that renal function will be preserved in those showing signs of obstruction—decreasing differential function (>10%) or increasing hydronephrosis—provided intervention is initiated promptly once these signs appear [2–7].
Mechanisms of UPJ obstruction in children
The reasons for this high spontaneous improvement rate for hydronephrosis can be found in the mechanisms of UPJ obstruction and in particular the unique behavior of the UPJ in young children [11]. In animal models of partial UPJ obstruction the obstruction is created in a manner similar to Chevalier’s model discussed elsewhere in this issue: the UPJ is constricted with a ligature or compressive device. This results in what is called a pressure-dependent or fixed-resistance UPJ obstruction in which the rate of flow across the UPJ is determined by the amount of pressure within the renal pelvis. Unfortunately, UPJ obstruction in children is generally caused by a dual obstruction composed of a narrowed or abnormal segment of ureter that produces an intrinsic obstruction combined with a second extrinsic obstruction. This extrinsic obstruction is caused by fibrous tissues that overlay the ureter just below the UPJ and cause a variable degree of compression, depending on the volume of fluid within the pelvis. The larger the pelvis is, the tighter the obstruction. This is a volume-dependent or variable-resistance obstruction that at low pelvic volumes does not produce any obstruction at all but that can be totally obstructive and prevent any egress across the UPJ when the pelvis is overfilled. This dual mechanism for human UPJ obstruction creates havoc with diagnostic testing because if the obstruction does not become activated during the test then absence of obstruction might be diagnosed erroneously. It also means that there is no extant animal model for partial UPJ obstruction, and therefore the observations that partial obstruction in children behaves as a chronic continuous obstruction are likely invalid. CPUUTO in children is in reality an intermittent series of acute obstructions that might have profoundly different effects on renal function than would a continuous chronic obstruction, and this is clearly reflected in the behavior of children with fetal and newborn obstruction whose hydronephrosis is rarely progressive or rarely damaging in utero or postnatally, where differential function in the affected kidney is usually >40% and in more than two-thirds of newborns spontaneously improves or resolves postnatally. Newborn hydronephrosis is clearly unique and even when associated with some degree of obstruction, both components of the obstruction appear to improve over time: the intrinsic or fixed narrowing gets larger with age and the extrinsic resistance becomes less significant as pelvis distensibility and degree of hydronephrosis decrease.
Problems in diagnosing UPJ obstruction in children
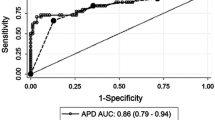
The diagnosis of obstruction is further compromised by the misbehavior of DR in newborns with severe hydronephrosis who were observed to have resolution of hydronephrosis over time [4]. In this group of patients, initial and follow-up DR studies revealed T½ times of >20 min in 38% and >30 min in 20%. Nearly 60% of nonobstructed hydronephroses showed obstructed tracer washout times. This clearly limits the ability of washout to be used as a predictive test for diagnosing obstruction. The question is why is DR washout so inaccurate in this population. A study that used US in three dimensions to measure the volume of the renal pelvis during DR in children with normal and hydronephrotic kidneys helped clarify this issue and explained how changes in pelvic volume could affect the accuracy of DR in diagnosing obstruction [16].
During DR all normal or hydronephrotic kidneys, whether obstructed or nonobstructed, in children age 1 month to 10 years responded similarly to diuresis, and between 15 and 60 min after injection of diuretic the renal pelvis enlarged to a maximum volume then gradually decreased in size. The mean average increase in volume for hydronephrotic kidneys ranged from 46% to 88% and exceeded 100% in children younger than 2 years. This volume expansion caused significant dilution of isotope within the dilated renal pelvis, which resulted in prolongation of the T½ time >20 min in 42% of nonobstructed hydronephrotic kidneys, which would have wrongly led to a diagnosis of obstruction.
The error potentials inherent in DR that affect T½ time reliability as a marker of obstruction have been well addressed in the literature. These include technical, physiological, and anatomical factors [17–19]. To these we must add the above-noted observations on diuretic-induced renal pelvis volume expansion, which adversely affects T½ time accuracy as a marker of obstruction. Consequently, isotope washout or T½ time should no longer be relied upon to determine whether obstruction exists in youngsters with hydronephrotic kidneys and it should no longer be used in operative decision-making.
Conclusion
Successful management of hydronephrosis requires early accurate diagnosis. However, both hydronephrosis in the newborn and CPUUTO are somewhat unique biological phenomena that can create a diagnostic dilemma. The hydronephrotic newborn kidney typically has nearly normal differential renal function, has not been subjected to progressive dilation and generally does not show signs of ever having been subjected to an obstruction. Furthermore, hydronephrosis resolves spontaneously in more than 65% of newborns and renal function remains stable or improves. CPUUTO, when it does exist, typically presents as repeated bouts of intermittent acute obstruction (Fig. 8), and, because it is different from and not represented by any extant animal model of partial obstruction, the previously described animal studies might not validly reflect the renal response to and behavior in CPUUTO.
Unfortunately, the diagnostic armamentarium that currently exists to assess obstruction in young children with hydronephrosis, US and DR, has not been able to accurately diagnose CPUUTO. This is because in the absence of any physiological markers of obstruction, the diagnosis in this age group is basically an exercise in prediction, trying to identify in advance which hydronephrotic kidney will deteriorate and require preemptive surgery before deterioration occurs. Unfortunately, neither the presence or severity of hydronephrosis nor the differential function or the washout rate of isotope through and from the renal pelvis predicts accurately the ultimate outcome: more than two-thirds of severely hydronephrotic kidneys spontaneously improve. Consequently, the only currently available way to accurately make the diagnosis of CPUUTO in hydronephrosis is to retrospectively use and compare serial studies to follow the kidney closely and to exclude or identify as early as possible the first signs of renal deterioration reflected as either decreasing (or failure to increase) differential function or progression of hydronephrosis. Prompt surgical intervention for these signs of deterioration is necessary regardless of patient age and has proved to be successful in restoring function and in preventing progressive deterioration in most cases while avoiding unnecessary surgery in the majority, whose hydronephrosis resolves.
In this setting of difficulties in diagnosing CPUUTO, MRU offers promise because of its ability to combine excellent anatomic imaging with quantitative measurements of renal function and qualitative assessment of renal nephropathy. But to provide competitive advantage, MRU must provide more than just pretty images and be more than just another test, and an invasive and costly one at that, for making serial retrospective observations. Exceptional value in diagnosing CPUUTO will be recognized when the unique features of MRU are proved to predict which kidney is obstructed and which requires surgical intervention before deterioration occurs. To date the preliminary clinical observations on the efficacy of MRU in diagnosing obstruction in children with hydronephrosis have been anecdotal, uncontrolled and in need of scientific validation [20–22]. Much work is needed to determine and refine the precise role of MRU in the evaluation of hydronephrosis, and one hopes this Workshop on MRU in Children will provide that impetus.
References
Tripp BM, Homsy YL (1995) Neonatal hydronephrosis—the controversy and the management. Pediatr Nephrol 9:503–509
Ransley PG, Dhillon HK, Gordon I et al (1990) The postnatal management of hydronephrosis diagnosed by prenatal ultrasound. J Urol 144(2 Pt 2):584–587
Koff SA, Campbell KD (1994) The nonoperative management of unilateral neonatal hydronephrosis: natural history of poorly functioning kidneys. J Urol 152:593–595
Ulman I, Jayanthi VR, Koff SA (2000) The long-term follow-up of newborns with severe unilateral hydronephrosis initially treated nonoperatively. J Urol 164:1101–1105
Chung YK, Chang PY, Lin CJ et al (1992) Conservative treatment of neonatal hydronephrosis. J Formos Med Assoc 91:75–80
Nonomura K, Yamashita T, Kanagawa K et al (1994) Management and outcome of antenatally diagnosed hydronephrosis. Int J Urol 1:121–128
Dhillon HK (1998) Prenatally diagnosed hydronephrosis: the Great Ormond Street experience. Br J Urol 81 [Suppl 2]:39–44
Koff SA (1990) Pathophysiology of ureteropelvic junction obstruction. Clinical and experimental observations. Urol Clin N Am 17:263–272
Koff SA (1981) Diagnosis of obstruction in experimental hydroureteronephrosis: mechanisms for progressive urinary tract dilation. Invest Urol 19:85–88
Koff SA (1983) Determinants of progression and equilibrium in hydronephrosis. Urology 21:496–500
Koff SA (1985) Pressure volume relationships in human hydronephrosis. Urology 25:256–258
Koff SA, Hayden LJ, Cirulli C et al (1986) Pathophysiology of ureteropelvic junction obstruction: experimental and clinical observations. J Urol 136:336–338
Djurhuus JC (1977) Dynamics of upper urinary tract. III. The activity of renal pelvis during pressure variations. Invest Urol 14:475–477
Djurhuus JC, Nerström B, Gyrd-Hansen N et al (1976) Experimental hydronephrosis. An electrophysiologic investigation before and after release of obstruction. Acta Chir Scand Suppl 472:17–28
Djurhuus JC, Stage P (1976) Percutaneous and intrapelvic pressure registration in hydronephrosis during diuresis. Acta Chir Scand Suppl 472:43–48
Koff SA, Binkovitz L, Coley B et al (2005) Renal pelvis volume during diuresis in children with hydronephrosis: implications for diagnosing obstruction with diuretic renography. J Urol 174:303–307
Conway JJ (1992) “Well-tempered” diuresis renography: its historical development, physiological and technical pitfalls, and standardized technique protocol. Semin Nucl Med 22:74–84
Gungor F, Anderson P, Gordon I (2002) Effect of the size of regions of interest on the estimation of differential renal function in children with congenital hydronephrosis. Nucl Med Commun 23:147–151
Connolly LP, Zurakowski D, Peters CA et al (2000) Variability of diuresis renography interpretation due to method of post-diuretic renal pelvic clearance half-time determination. J Urol 164:467–471
McDaniel BB, Jones RA, Scherz H et al (2005) Dynamic contrast-enhanced MR urography in the evaluation of pediatric hydronephrosis: part 2, anatomic and functional assessment of ureteropelvic junction obstruction. AJR 185:1608–1614
Kirsch AJ, McMann LP, Jones RA et al (2006) Magnetic resonance urography for evaluating outcomes after pediatric pyeloplasty. J Urol 176(4 Pt 2):1755–1761
McMann LP, Kirsch AJ, Scherz HC et al (2006) Magnetic resonance urography in the evaluation of prenatally diagnosed hydronephrosis and renal dysgenesis. J Urol 76:1786–1792
Author information
Authors and Affiliations
Corresponding author
Additional information
The author has no financial interests, investigational or “off-label” uses to disclose.
Rights and permissions
About this article
Cite this article
Koff, S.A. Requirements for accurately diagnosing chronic partial upper urinary tract obstruction in children with hydronephrosis. Pediatr Radiol 38 (Suppl 1), 41–48 (2008). https://doi.org/10.1007/s00247-007-0590-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-007-0590-2