Abstract
Purpose
To determine the diagnostic accuracy of anteroposterior renal pelvic diameter (APD) measurement and the society for fetal urology (SFU) grading in neonatal ultrasonography (USG) for detecting uropathy in newborns having antenatal isolated hydronephrosis (IH), characterized by hydronephrosis without ureter and bladder abnormalities, and to study time to resolution and factors predicting resolution of insignificant hydronephrosis.
Methods
Ninety-six healthy newborns (129 kidneys) with IH, who underwent USG at age 7–30 days and voiding cystourethrography (VCUG) in conjunction with diuretic renography (DR) if APD > 10 mm or SFU grade 3–4 in neonatal USG, and at least a 12-month follow-up were divided into significant and insignificant hydronephrosis using the combined data of sequential USG, VCUG, and DR as the reference standard.
Results
Areas under the receiver operating characteristic plots (95 % CI) were 0.86 (0.79–0.94) versus 0.81 (0.73–0.89); p = 0.08, and 87.6 versus 79.8 % of cases were correctly classified, for APD ≥ 16 mm versus SFU grade 4, respectively. Ureteropelvic junction obstruction (UPJO) was the most common uropathy diagnosed. Of 85 kidneys with insignificant hydronephrosis, 57 underwent spontaneous resolution. The resolution rates were 24, 40, and 68 % at age 6, 12, and 24 months, respectively. APD was the only independent factor predicting resolution with the hazard ratio of 0.83 (95 % CI 0.74–0.92; p = 0.001).
Conclusions
In IH, neonatal USG was a useful diagnostic tool to detect uropathy, mainly UPJO. Further investigation should be recommended when APD ≥ 16 mm or SFU grade 4.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Postnatal investigation for antenatal hydronephrosis (AH) including voiding cystourethrography (VCUG) and diuretic renography (DR) is indicated if abnormal ureter or bladder is detected in fetal or neonatal ultrasonography (USG) [1–3]. The imaging required in infants with isolated hydronephrosis (IH), characterized by renal pelvis dilatation without ureter and bladder abnormalities, is a subject of debate due to the high incidence but limited prognostic information [4–7]. It is crucial to differentiate significant hydronephrosis, such as ureteropelvic junction obstruction (UPJO), which could cause renal damage if left untreated, from insignificant hydronephrosis, a self-limited condition.
Several studies showed that the outcomes of AH and severity, classified by fetal or neonatal USG findings, were correlated [8–11]. However, the validity of neonatal USG in IH is unknown. We conducted this study to determine the diagnostic accuracy of two classification systems introduced to standardize the neonatal USG results, anteroposterior renal pelvic diameter (APD) measurement and the society for fetal urology (SFU) grading [12–14], for detecting pathology in healthy newborns with IH. Time to resolution and factors predicting resolution of insignificant hydronephrosis were evaluated.
Patients and methods
A retrospective review of healthy, full-term infants with AH, referred to a university-based, pediatric outpatient center from January 1, 2007 to December 31, 2012, and at least a 12-month follow-up, was conducted. Newborns who underwent neonatal USG at age 7–30 days and VCUG in conjunction with DR if APD > 10 mm or SFU grade 3–4 in neonatal USG were eligible. Exclusion criteria were single, cystic, dysplastic, or hyperechogenic kidney, hydroureter or dilated, thick-walled bladder in neonatal USG. Only newborns with IH were analyzed.
All kidney, ureter, and bladder USG was performed in the supine position after adequate oral hydration by two radiologists who were aware of AH but blind to VCUG and DR results. Severity of hydronephrosis was determined after voiding based on APD measurement in the mid-renal transverse plane at cortical-pelvic margins within the confines of the renal cortex, and SFU grading.
VCUG was performed at age 0.5–3 months. Vesicoureteral reflux (VUR) was graded during filling and voiding using the International Reflux Study Committee classification [15]. DR was performed after adequate hydration using 99mtechnetium-mercaptoacetyltriglycine (99mTc-MAG3) at the minimum age of 6–8 weeks. Differential renal function was assessed during the first few minutes. Intravenous furosemide was given, and renogram curves along with the half-time drainage were assessed at 20 min. Post-micturition films were taken at 120 min. In patients with residual contrast, bladder catheterization was performed.
Normal DR was characterized by an early peak at 2–5 min followed by complete emptying either spontaneously, after furosemide, or after micturition. An obstructive pattern included: (1) the renogram rose continuously over 20 min or appeared as a plateau; or (2) the half-time drainage was >30 min, or the half-time drainage was >15 min with relative renal function <40 %. Repeated DR was indicated for indeterminate results in the initial DR or worsening dilatation in the subsequent USG.
Outcomes at the last visit were divided into significant and insignificant hydronephrosis, using the combined data of sequential USG, VCUG, and DR as the reference standard. Insignificant hydronephrosis was defined as normal VCUG and stable or decreasing APD in sequential USG if the APD was ≤10 mm in the neonatal USG, or normal VCUG and DR if the APD was >10 mm in the neonatal USG. In patients with insignificant hydronephrosis, sequential USG was performed at age 3, 6, 12, 18, and 24 months, and every year thereafter until resolution, defined as APD ≤ 5 mm and SFU grade ≤1 in two consecutive USG. Patients with significant abnormalities in USG, VCUG, or DR were classified as having significant hydronephrosis.
Statistical analysis
Data analysis was conducted using Stata 12 (StataCorp, College Station, TX). p values of <0.05 were considered significant. Descriptive data are reported as mean ± standard deviation (SD) or median (interquartile range, IQR) as appropriate. Data were compared using the Chi-square test and Student’s t test for categorical and continuous variables, respectively. Receiver operating characteristic (ROC) plots were used to determine the optimal cutoffs for the APD and SFU grading. A formal comparison of the number of correctly classified cases, reflecting differences in sensitivity and specificity, was made by comparing area under the ROC curves (AUC). The Kaplan–Meier method was used to estimate time to resolution of physiologic hydronephrosis. Four potential predicting factors for resolution chosen a priori, namely gender, laterality, SFU grade, and APD were evaluated using Cox proportional hazard analysis. Assumptions about the linearity of SFU grading were checked, and the hazard ratios (HR) with 95 % confidence interval (CI) were examined. Adjacent categories were collapsed together into categorical groupings if appropriate when these assumptions were not met. Chi-square test for model fit and test of interaction were performed.
Completed checklists of standards for reporting of diagnostic accuracy (the STARD initiative) are shown in Online Resource 1.
Results
Patient characteristics
Of 128 eligible healthy newborns with AH, 26 were excluded due to abnormal neonatal USG including dysplastic kidney (12), hydroureter (10), double collecting system with ureterocele (3), and abnormal urinary bladder (1). Six patients were incompletely investigated or lost to follow-up. Hence, 96 patients with IH (82.3 % male and 17.7 % female; 129 kidneys) were analyzed. The mean gestational age was 37.9 ± 1.1 weeks, and the mean birth weight was 3.18 ± 0.50 kg. The median follow-up time was 29.5 (17.7–49.3) months.
Postnatal radiological results
Neonatal USG was performed at the median age of 8 (7–16) days. Hydronephrosis was resolved in four patients (five kidneys). Sixty patients (62.5 %) had unilateral hydronephrosis (43 left kidneys; 17 right kidneys), and 32 patients (34.7 %) had bilateral hydronephrosis. The mean APD was 12.16 ± 10.44 mm. SFU grades 0, 1, 2, 3, and 4 were observed in 5 (3.9 %), 22 (17.1 %), 35 (27.1 %), 27 (20.9 %), and 40 (31.0 %) patients, respectively.
VCUG was performed at the median age of 38 (18–67) days. Abnormal VCUG were observed in five patients (5.2 %) or seven kidneys (5.4 %), consistent with VUR grade 1, 2, 3, and 5 in 2, 1, 1, and 1 patients, respectively. Every patient received continuous antibiotic prophylaxis. None were operated. The patient with VUR grade 5 was exclusively breastfed and did not regain the birth weight when initial USG was performed at the age of 7 days. Partially distended bladder secondary to neonatal oliguria could contribute to the absence of hydroureter in the initial neonatal USG as the refluxing ureter was observed in subsequent USG.
DR was performed in 69 of 96 patients (71.9 %) at the median age of 59 (42–88) days. UPJO were identified in 31 patients (32.3 %) or 37 kidneys (28.7 %). Pyeloplasty was performed in 20 patients (24 kidneys) at the mean age of 11.7 ± 5.9 months.
Outcomes of IH
Of the 129 kidneys, 85 (65.9 %) and 44 (34.1 %) had insignificant and significant hydronephrosis, respectively. Four patients with resolved hydronephrosis in neonatal USG had insignificant hydronephrosis. Gender, gestational age, birth weight, and laterality did not differ between both groups (Table 1). The APD was larger and SFU grade 4 was more common in significant than in insignificant hydronephrosis (p < 0.001).
ROC curves were used to evaluate optimal cutoffs for determining sensitivity and specificity in detecting significant hydronephrosis (Fig. 1). The APD and SFU grading yielded AUC (95 % CI) of 0.86 (0.79–0.94) and 0.81 (0.73–0.89), respectively (p = 0.08). For the APD of ≥16 mm, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) with 95 % CI were 70.5 (60.0–83.9), 96.5 (92.5–100), 91.2 (81.6–100), and 86.3 (79.4–93.2) %, respectively, and 87.6 % of cases were correctly classified. For SFU grade 4, sensitivity, specificity, PPV, and NPV (95 % CI) were 65.9 (51.9–79.9), 87.1 (79.9–94.2), 72.5 (58.6–86.3), and 83.1 (75.4–90.9) %, respectively, and 79.8 of cases were correctly classified. False positive rates for APD ≥ 16 mm and SFU grade 4 were 3.5 and 12.9 %, respectively. False negative rates for APD ≥ 16 mm and SFU grade 4 were 29.5 and 34.1 %, respectively (Table 1).
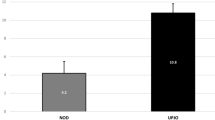
Resolution of insignificant hydronephrosis
Over the time of 1,360 months that 85 kidneys with insignificant hydronephrosis contributed to the study, 57 kidneys underwent spontaneous resolution, whereas 28 kidneys had persistent hydronephrosis. A Kaplan–Meier graph illustrating the probability of having hydronephrosis at select time points is shown in Fig. 2. Overall rates (95 % CI) of having hydronephrosis were 76.2 (65.6–83.9), 60.0 (48.5–69.6), and 31.6 (20.7–43.1) %, and resolution occurred in 23.8, 40.0, and 68.4 % at age 6, 12, and 24 months, respectively.
Multivariate analysis revealed that gender (female vs. male), laterality (bilateral vs. unilateral), and SFU grading (0–2 vs. 3–4) were not associated with resolution with HR (95 % CI) of 1.30 (0.68–2.50), 0.93 (0.53–1.62), and 1.09 (0.53–2.23), respectively. By contrast, the APD was significantly associated with resolution (HR 0.83; 95 % CI 0.74–0.92, p = 0.001). Likelihood ratio test showed acceptable fit of the model (p < 0.001). We did not find any evidence of effect modification of one on the other covariates.
Discussion
Neonatal USG, an initial diagnostic modality of choice for AH, provides better anatomic resolution due to fewer interposed tissues when compared to fetal USG. In this study, neonatal USG correctly identified dysplastic or duplex kidney in 12 % of patients diagnosed with AH by fetal USG. We focused on healthy, full-term infants having AH without abnormal ureter and bladder. UPJO was the most common pathologic finding. The optimal cutoffs of neonatal USG parameters were evaluated. The APD and SFU grading were good indicators for detecting significant hydronephrosis with similar overall diagnostic value based on the AUC.
Diagnostic performance of USG is influenced by study population and cutoff value [8, 16–19]. A large series of AH with a long-term follow-up from the Great Ormond Street experience reported by Dhillon [19] demonstrated that APD < 12 mm with no calyceal involvement posed no risk of surgery, whereas APD > 50 mm inevitably warranted surgery. Our study showed that APD ≥ 16 mm and SFU grade 4 yielded an excellent specificity and PPV; thus, neonatal USG could be used as a diagnostic tool to detect pathology in IH, mainly UPJO. Additional postnatal imaging should be recommended for APD ≥ 16 mm or SFU grade 4. The modest sensitivity and NPV decreased the accuracy of neonatal USG as a screening tool, and postnatal investigation should be considered on a case-by-case basis for APD < 16 mm and SFU grade <4. This recommendation could prevent a misdiagnosis of significant pathology and reduce the use of unneeded postnatal imaging with potential harmful effects from radiation exposure and urinary catheterization.
The majority of patients with IH had insignificant hydronephrosis. Until spontaneous resolution occurs, potential morbidity associated with hydronephrosis causes substantial parental concerns. Comprehensive prognostic information could reduce ongoing parental distress and prevent repeated unnecessary imaging. Resolution was inversely correlated with the severity of hydronephrosis, and details of resolution in mild cases were previously described [5, 6]. Data shown in the study by Longpre et al. [20] that the resolution rate of AH was determined by the APD and SFU grading provide an excellent prognostic overview. Nevertheless, the information is partially relevant to patients with insignificant hydronephrosis as prognosis of AH is variable by the underlying pathology. Our study is the first to report the prognostic data on insignificant hydronephrosis. However, the long-term prognosis of insignificant hydronephrosis requires further elucidation as we found that spontaneous resolution occurred within 2 years in the majority of these patients and only one-third of the patients with insignificant hydronephrosis had a follow-up of more than 18 months. The APD was the only independent factor predicting resolution. An increased chance of resolution by 17 % was observed with every 1-mm decrease of APD.
Selection bias toward the diagnosis of insignificant hydronephrosis as opposed to VUR was avoided as VCUG was performed in every patient. As patients with abnormalities of the ureter and bladder in neonatal USG were excluded and the incidence of VUR in IH was low, routine VCUG may yield limited benefit in IH. Moreover, a high spontaneous resolution and a low likelihood of urinary tract infection were noted in VUR associated with AH [21, 22]. Nevertheless, prompt recognition and management of urinary tract infection should be emphasized during parental counseling for IH.
There were a few limitations to this study. First, the diagnosis of insignificant hydronephrosis depended on the results of DR which are open to interpretation and subjective. However, the serial imaging protocol and length of observation allowed for the diagnosis of UPJO in subsequent imaging and could minimize misclassification. Second, USG interpretation is operator dependent, and inter-rater variability was not evaluated in this study. Nevertheless, APD measurement is objective and could improve the comparison of USG results between different studies [23]. Third, there was a trend toward the superior performance of APD measurement when compared to SFU grading although the difference did not reach statistical significance. A larger sample size may be required to detect the difference of the diagnostic accuracy between the APD and SFU grading.
In conclusion, APD measurement and SFU grading in the USG performed at the age of 7–30 days were a useful diagnostic tool for detecting pathology in IH. Prospective large-scale studies are required to validate our findings before the threshold for treatment decisions is recommended in clinical practice. Nevertheless, postnatal management and parental counseling for patients with IH could be individualized based upon neonatal USG parameters. Selective postnatal diagnostic procedures could reduce unnecessary investigation and utilization of limited healthcare resources. Our findings are applicable to healthy infants without ureter and bladder abnormalities as neonates with prematurity, oligohydramnios, renal failure, or extrarenal structural anomalies were excluded.
References
Riccabona M (2004) Assessment and management of newborn hydronephrosis. World J Urol 22(2):73–78. doi:10.1007/s00345-004-0405-0
Yiee JH, Tasian GE, Copp HL (2011) Management trends in prenatally detected hydronephrosis: national survey of pediatrician practice patterns and antibiotic use. Urology 78(4):895–901. doi:10.1016/j.urology.2011.04.027
Braga LH, Ruzhynsky V, Pemberton J, Farrokhyar F, Demaria J, Lorenzo AJ (2014) Evaluating practice patterns in postnatal management of antenatal hydronephrosis: a national survey of Canadian pediatric urologists and nephrologists. Urology 83(4):909–914. doi:10.1016/j.urology.2013.10.054
Sidhu G, Beyene J, Rosenblum ND (2006) Outcome of isolated antenatal hydronephrosis: a systematic review and meta-analysis. Pediatr Nephrol 21(2):218–224. doi:10.1007/s00467-005-2100-9
Tombesi MM, Alconcher LF (2012) Short-term outcome of mild isolated antenatal hydronephrosis conservatively managed. J Pediatr Urol 8(2):129–133. doi:10.1016/j.jpurol.2011.06.009
Mami C, Paolata A, Palmara A, Marrone T, Berte LF, Marseglia L, Arena F, Manganaro R (2009) Outcome and management of isolated moderate renal pelvis dilatation detected at postnatal screening. Pediatr Nephrol 24(10):2005–2008. doi:10.1007/s00467-009-1229-3
Garne E, Loane M, Wellesley D, Barisic I (2009) Congenital hydronephrosis: prenatal diagnosis and epidemiology in Europe. J Pediatr Urol 5(1):47–52. doi:10.1016/j.jpurol.2008.08.010
Coplen DE, Austin PF, Yan Y, Blanco VM, Dicke JM (2006) The magnitude of fetal renal pelvic dilatation can identify obstructive postnatal hydronephrosis, and direct postnatal evaluation and management. J Urol 176(2):724–727. doi:10.1016/j.juro.2006.03.079 discussion 727
Passerotti CC, Kalish LA, Chow J, Passerotti AM, Recabal P, Cendron M, Lee RS, Lopez AB, Retik AB, Nguyen HT (2011) The predictive value of the first postnatal ultrasound in children with antenatal hydronephrosis. J Pediatr Urol 7(2):128–136. doi:10.1016/j.jpurol.2010.09.007
Onen A (2007) Treatment and outcome of prenatally detected newborn hydronephrosis. J Pediatr Urol 3(6):469–476. doi:10.1016/j.jpurol.2007.05.002
Hothi DK, Wade AS, Gilbert R, Winyard PJ (2009) Mild fetal renal pelvis dilatation: much ado about nothing? Clin J Am Soc Nephrol 4(1):168–177. doi:10.2215/CJN.00810208
Davenport MT, Merguerian PA, Koyle M (2013) Antenatally diagnosed hydronephrosis: current postnatal management. Pediatr Surg Int 29(3):207–214. doi:10.1007/s00383-012-3258-4
Timberlake MD, Herndon CD (2013) Mild to moderate postnatal hydronephrosis–grading systems and management. Nat Rev Urol 10(11):649–656. doi:10.1038/nrurol.2013.172
Vemulakonda V, Yiee J, Wilcox DT (2014) Prenatal hydronephrosis: postnatal evaluation and management. Curr Urol Rep 15(8):430. doi:10.1007/s11934-014-0430-5
Lebowitz RL, Olbing H, Parkkulainen KV, Smellie JM, Tamminen-Mobius TE (1985) International system of radiographic grading of vesicoureteric reflux. International Reflux Study in Children. Pediatr Radiol 15(2):105–109
de Kort EH, Bambang Oetomo S, Zegers SH (2008) The long-term outcome of antenatal hydronephrosis up to 15 millimetres justifies a noninvasive postnatal follow-up. Acta Paediatr 97(6):708–713. doi:10.1111/j.1651-2227.2008.00749.x
Dias CS, Silva JM, Pereira AK, Marino VS, Silva LA, Coelho AM, Costa FP, Quirino IG, Simoes ESAC, Oliveira EA (2013) Diagnostic accuracy of renal pelvic dilatation for detecting surgically managed ureteropelvic junction obstruction. J Urol 190(2):661–666. doi:10.1016/j.juro.2013.02.014
Ismaili K, Avni FE, Wissing KM, Hall M (2004) Long-term clinical outcome of infants with mild and moderate fetal pyelectasis: validation of neonatal ultrasound as a screening tool to detect significant nephrouropathies. J Pediatr 144(6):759–765. doi:10.1016/j.jpeds.2004.02.035
Dhillon HK (1998) Prenatally diagnosed hydronephrosis: the Great Ormond Street experience. Br J Urol 81(Suppl 2):39–44
Longpre M, Nguan A, Macneily AE, Afshar K (2012) Prediction of the outcome of antenatally diagnosed hydronephrosis: a multivariable analysis. J Pediatr Urol 8(2):135–139. doi:10.1016/j.jpurol.2011.05.013
St Aubin M, Willihnganz-Lawson K, Varda BK, Fine M, Adejoro O, Prosen T, Lewis JM, Shukla AR (2013) Society for fetal urology recommendations for postnatal evaluation of prenatal hydronephrosis—will fewer voiding cystourethrograms lead to more urinary tract infections? J Urol 190(4 Suppl):1456–1461. doi:10.1016/j.juro.2013.03.038
Estrada CR Jr (2008) Prenatal hydronephrosis: early evaluation. Curr Opin Urol 18(4):401–403. doi:10.1097/MOU.0b013e328302edfe
Pereira AK, Reis ZS, Bouzada MC, de Oliveira EA, Osanan G, Cabral AC (2011) Antenatal ultrasonographic anteroposterior renal pelvis diameter measurement: is it a reliable way of defining fetal hydronephrosis? Obstet Gynecol Int 2011:861865. doi:10.1155/2011/861865
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard
The study was approved by the Institutional Review Board Committee of Faculty of Medicine, Chulalongkorn University, and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Parents gave their informed consent prior to the inclusion in the study. Patient anonymity was preserved.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rianthavorn, P., Limwattana, S. Diagnostic accuracy of neonatal kidney ultrasound in children having antenatal hydronephrosis without ureter and bladder abnormalities. World J Urol 33, 1645–1650 (2015). https://doi.org/10.1007/s00345-015-1478-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-015-1478-7