Abstract
This essay illustrates various patterns of progression of osteonecrosis of the knee and the relationship between early MR imaging findings and radiologic outcome in children with acute lymphocytic leukemia. It also includes a review of nonosteonecrosis signal abnormalities, which are common in the knee region and are often transient. Such abnormalities must be distinguished from osteonecrosis, which can lead to joint collapse and predispose to secondary arthritis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteonecrosis is a frequent complication of treatment of leukemia and lymphoma in children [1–5]. Osteonecrosis is most frequently attributed to intensive glucocorticosteroid (GCS) therapy, which is an essential component of contemporary antineoplastic regimens [2]. Osteonecrosis can cause acute bone pain, but the absence of initial pain does not exclude long-term complications associated with articular surface collapse. Such complications cause chronic pain and potentially require arthroplasty [6, 7]. Although there is no universally accepted treatment to prevent progression of osteonecrosis, several therapies, including bisphosphonates and autologous stem cell therapy, show promise [2, 8–10].
Several factors are predictive of the risk of osteonecrosis in children with hematologic cancers: age 11 years or more at the time of therapy, high doses of corticosteroids, and pharmacogenetic parameters (e.g., the vitamin D receptor FokI start-site CC genotype and the thymidylate synthase low-activity 2/2 enhancer repeat genotype) [1, 11]. However, the diagnosis of osteonecrosis is based on imaging findings. Therefore, radiologists must be able to distinguish osteonecrosis from other signal abnormalities associated with the knee in children with leukemia. This pictorial essay illustrates the progression of osteonecrosis lesions involving the knees, the relationship of early MR imaging findings to radiologic outcome, and signal abnormalities that can occur in patients at risk of osteonecrosis.
Diagnosis
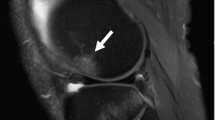
Osteonecrosis is usually diagnosed on the basis of characteristic MR imaging findings, which might be present before any symptoms occur [12]. MR imaging allows the earliest and most accurate diagnosis of osteonecrosis. These lesions are well circumscribed and have a geographical appearance (Figs. 1, 2, 3, 4 and 5). The most typical feature of the early osteonecrosis lesion is the characteristic interface between living and dead bone at the lesion’s periphery that is readily visible without the use of a contrast agent (Fig. 1); contrast material is therefore not routinely used for diagnosis of osteonecrosis [13]. This interface appears as a thin, winding line that circumscribes and clearly demarcates the zone of necrosis. This line has low signal intensity on T1-weighted (T1-W) images and high signal intensity on short T1 inversion recovery (STIR) images. On T2-weighted images, both low-intensity (outer) and high-intensity (inner) lines are visible, forming a “double line sign.” As Mitchell et al. [14] described for osteonecrosis of the femoral head, in early osteonecrosis the inner zone of necrosis has the signal intensity of normal fatty marrow. Later, especially after subchondral collapse, which is a complication of progressive osteonecrosis near a joint surface, the inner zone of necrosis might show low signal intensity or might be inhomogeneous [13, 14]. Radiography or CT is the preferred method for diagnosis of subchondral fracture [15], an early sign of which is a subchondral crescent-like lucency. MR imaging is less sensitive (although very specific) for the diagnosis of early subchondral fracture, which can appear as a high-signal-intensity line that appears to represent accumulated fluid on T2-weighted or STIR images (Fig. 2).
Early MR imaging appearance of osteonecrosis lesions in the knees of a 14-year-old boy undergoing therapy for ALL. a, b Coronal T1-W (a) and STIR (b) images show the barely noticeable outline of evolving osteonecrosis lesions (arrows), correctly defining the boundaries of signal abnormalities. c, d Four months later, the boundaries are more typical in appearance on coronal T1-W (c) and STIR (d) images (arrows). This pattern of development shows that areas of necrosis might be large at the outset rather than growing from smaller necrotic lesions
Osteonecrosis of the distal femoral and proximal tibial epiphyses in the right knee of a 15-year-old boy with ALL. a Coronal T1-W image. b On a STIR MR image, a subchondral fracture (arrow) appears as a high-signal-intensity line consistent with fluid. c A radiographic image demonstrates deformation and collapse of the articular surface (arrow)
Extensive subchondral osteonecrosis of the epiphyses, leading to collapse and deformation of the articular surface in the knees of a 13-year-old girl undergoing therapy for ALL. a, b Coronal T1-W (a) and STIR (b) MR images show extensive lesions of osteonecrosis bilaterally (arrows) in the diaphyses, metaphyses, and epiphyses of the distal femurs and proximal tibias. In the femoral epiphyses, the osteonecrosis lesions extend subchondrally. This girl’s GCS therapy was stopped after the diagnosis of osteonecrosis. c, d Six years later, coronal T1-W (c) and STIR (d) MR images show that the lesions have visibly decreased in size. Deformation of the articular surface with loss of sphericity of the distal femoral epiphyses, however, is evident bilaterally (arrows). e, f On these anterior-posterior radiographs of the right (e) and left (f) knees, deformation of the articular surface is seen (arrows). These deformations can predispose the patient to arthritic complications
Small non-subchondral osteonecrosis lesion of the epiphysis in the knees of a 6-year-old girl undergoing therapy for ALL. a, b Coronal T1-W (a) and STIR (b) MR images show lesions of osteonecrosis bilaterally in the diaphyses, metaphyses, and epiphyses of the distal femurs and proximal tibias. None of the epiphyseal lesions extends subchondrally. The girl’s GCS treatment was stopped after the lesions were diagnosed. c, d Coronal T1-W (c) and STIR (d) MR images obtained 2 years later demonstrate considerable reduction in the size of the lesions, without residual deformity. The articular surface of the knees appears intact
Imaging appearance of osteonecrosis versus localized bone relapse of leukemia in an 11-year-old girl. a, b Areas of localized relapse (open arrows) are seen as regions of homogeneous, very low signal intensity on T1-W images (a) and high signal intensity on STIR (b) MR images of the knees, in contrast to coexisting lesions of osteonecrosis (solid arrows). Bone relapse of pre-B-cell ALL was confirmed by needle biopsy of the distal left femoral lesion. Cerebrospinal fluid and bone marrow aspirates disclosed no evidence of leukemia
The evolution of radiographic findings in osteonecrosis is as follows: in early MR-evident osteonecrosis, radiographs are often normal. Later, areas of sclerosis and lucency might appear, followed by the development of subchondral collapse and fragmentation of the articular surface.
Relationship between MR imaging presentation and long-term outcome
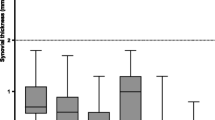
Because it allows direct visualization of the osteonecrotic lesion, including its size, location, and relationship to the articular surface, MR imaging allows early, accurate diagnosis of osteonecrosis and provides information that can help to predict the long-term outcome [16–18]. The long-term outcome of atraumatic osteonecrosis of the knee is dependent on the location of the lesion. Subchondral collapse is associated with lesions involving epiphyses, especially when they abut a cartilaginous articular surface (Fig. 3) [17, 18]. Lesions that do not extend to the articular surface might heal without causing deformity to the surface and thereby increasing the risk of long-term complications (Fig. 4). Several investigators have reported that extensive epiphyseal involvement is the most important MR imaging predictor of subchondral collapse in atraumatic osteonecrosis of the knee. Korholz et al. [17] reported that osteonecrosis lesions 900 mm2 or more in area are associated with joint destruction and the need for joint replacement in children with ALL. Sakai et al. [16] reported that in steroid- or alcohol-related osteonecrosis of the femoral condyle, lesions involving more than one-third of the condyle on a mid-coronal slice or more than one of three zones (anterior, middle, or posterior) on a mid-sagittal slice predict collapse. Mont et al. [18] studied 148 knees with osteonecrosis. Epiphyseal lesions with a combined necrotic angle of 250° or more were associated with decreased knee functionality and the need for arthroplasty.
When precise localization of an osteonecrotic lesion is desired (e.g., for estimating prognosis or surgical planning), coronal, sagittal, and possibly axial planes can be used with T1-W and STIR sequences [13, 18]. For screening purposes T1-W and STIR sequences in the coronal plane alone might be adequate. GCS-related osteonecrosis is characterized by involvement of multiple sites. Therefore, it might be useful to extend the MR imaging examination to include the opposite knee or other weight-bearing joints to detect involvement that could further compromise ambulation.
Differential diagnoses
MR signal abnormalities are common in the knee region of children treated for ALL and can present a challenge for a radiologist who is expected to provide a prognosis for these abnormalities. Osteonecrosis should be differentiated from bone marrow edema and other non-specific self-resolving signal abnormalities that are unrelated to ALL. Localized ALL recurrence in bone has a distinct appearance and if the results of bone marrow aspirates are normal biopsy of the lesion is warranted [19].
Localized relapse of ALL in bones of the extremities after allogeneic stem cell transplantation can carry a poor prognosis for survival and should not be confused with osteonecrosis. Areas of leukemia relapse to bone are seen as regions of homogeneous, very low signal intensity on T1-W images and as regions of high signal intensity on STIR MR images and they have well-defined margins (Fig. 5).
Several authors have described patchy bone marrow signal abnormalities in the knee region in children with leukemia [4, 20–22]. Three frequently encountered types of signal abnormality are “punctate foci” (Fig. 6), a bone marrow edema pattern (Fig. 7), and a diffuse inhomogeneity pattern (Fig. 8). These nonspecific signal changes are often transient.
Punctate foci in the knees of a 15-year-old boy with ALL. a, b Multiple dot-like signal abnormalities of low intensity on coronal T1-W (a) and high signal intensity on STIR (b) MR images (arrows) are visible. c, d These signal abnormalities were no longer visible 3 years later on coronal T1-W (c) and STIR (d) MR images of the patient’s knees
Bone marrow edema in the metaphyses of bilateral proximal femurs and distal tibias of a 17-year-old boy with ALL. a, b Coronal T1-W (a) and STIR (b) MR images show bone marrow edema (arrows). c, d On coronal T1-W (c) and STIR (d) MR images obtained 16 months later, the isolated signal abnormalities consistent with bone marrow edema are no longer visible
Diffuse inhomogeneity pattern coexisting with osteonecrosis in a 15-year-old girl undergoing therapy for ALL, after 15 months of continuous complete remission. a, b Diffuse inhomogeneity of the bone marrow signal is visible in bilateral metaphyses of the distal femurs and proximal tibias (open arrows), showing low signal intensity on coronal T1-W (a) and high signal intensity on STIR (b) MR images. Typical lesions of osteonecrosis are seen in the bilateral epiphyses of the distal femurs, proximal tibias, and left tibial diaphysis (solid arrows). c, d After an additional 6 years of complete remission, the bone marrow signal intensity had returned to fat-like signal on coronal T1-W (c) and STIR (d) MR images. In contrast, lesions of osteonecrosis persist (solid arrows)
Punctate foci of abnormal signal (diameter 1–3 mm; Fig. 6) are nonspecific marrow abnormalities commonly encountered in children with leukemia as multiple signal abnormalities of similar size and appearance on MR imaging of the knees. Punctate foci are smaller than osteonecrosis lesions and lack a discernible interior area of fat-like intensity [20, 22, 23].
Bone marrow edema (Fig. 7) is a painful condition described as a predecessor and/or companion of early osteonecrosis lesions [24] or a sequela of subchondral fracture caused by more advanced osteonecrosis [25, 26]. It can also accompany epiphyseal stress fracture or infection or occur independently as transient bone marrow edema syndrome [27]. MR imaging characteristics include low signal intensity on T1-W images and very high signal intensity on STIR coronal MR images (Fig. 7). Unlike osteonecrosis lesions with their sharply defined borders, bone marrow edema appears as a gradual transition between normal and abnormal areas. Isolated bone marrow edema is usually transient; when the condition is secondary, prognosis depends on the underlying disorder.
The diffuse inhomogeneity pattern lacks the sharply circumscribed outline and the inner zone of fat-like signal intensity seen in osteonecrosis lesions (Fig. 8). This pattern is nonspecific and has been observed in the knees of ALL patients in complete remission as well as in patients with bone marrow relapse [20].
Conclusion
Osteonecrosis of the knee is a frequent complication of treatment of acute leukemia in children and can lead to joint collapse and predispose to secondary arthritis. MR imaging provides early, accurate diagnosis of osteonecrosis of the knee and helps to predict outcome by precisely characterizing lesion size and location. Non-osteonecrosis signal abnormalities are common in the knee region in children with ALL and must be distinguished from osteonecrosis because of their different prognostic significance.
References
Mattano LA Jr, Sather HN, Trigg ME et al (2000) Osteonecrosis as a complication of treating acute lymphoblastic leukemia in children: a report from the Children’s Cancer Group. J Clin Oncol 18:3262–3272
Sala A, Mattano LA, Barr RD (2007) Osteonecrosis in children and adolescents with cancer: an adverse effect of systemic therapy. Eur J Cancer 43:683–689
Strauss AJ, Su JT, Dalton VM et al (2001) Bony morbidity in children treated for acute lymphoblastic leukemia. J Clin Oncol 19:3066–3072
Ojala AE, Lanning FP, Paakko E et al (1997) Osteonecrosis in children treated for acute lymphoblastic leukemia: a magnetic resonance imaging study after treatment. Med Pediatr Oncol 29:260–265
Ojala AE, Paakko E, Lanning FP et al (1999) Osteonecrosis during the treatment of childhood acute lymphoblastic leukemia: a prospective MRI study. Med Pediatr Oncol 32:11–17
Ohzono K, Saito M, Takaoka K et al (1991) Natural history of nontraumatic avascular necrosis of the femoral head. J Bone Joint Surg Br 73:68–72
Werner A, Jager M, Schmitz H et al (2003) Joint-preserving surgery for osteonecrosis and osteochondral defects after chemotherapy in childhood. Klin Padiatr 215:332–337
Gangji V, Toungouz M, Hauzeur JP (2005) Stem cell therapy for osteonecrosis of the femoral head. Expert Opin Biol Ther 5:437–442
Hernigou P, Beaujean F (2002) Treatment of osteonecrosis with autologous bone marrow grafting. Clin Orthop Relat Res 405:14–23
Nishii T, Sugano N, Miki H et al (2006) Does alendronate prevent collapse in osteonecrosis of the femoral head? Clin Orthop Relat Res 443:273–279
Relling MV, Yang W, Das S et al (2004) Pharmacogenetic risk factors for osteonecrosis of the hip among children with leukemia. J Clin Oncol 22:3930–3936
Karimova EJ, Rai SN, Ingle D et al (2006) MRI of knee osteonecrosis in children with leukemia and lymphoma: part 2, clinical and imaging patterns. AJR 186:477–482
Saini A, Saifuddin A (2004) MRI of osteonecrosis. Clin Radiol 59:1079–1093
Mitchell DG, Rao VM, Dalinka MK et al (1987) Femoral head avascular necrosis: correlation of MR imaging, radiographic staging, radionuclide imaging, and clinical findings. Radiology 162:709–715
Stevens K, Tao C, Lee SU et al (2003) Subchondral fractures in osteonecrosis of the femoral head: comparison of radiography, CT, and MR imaging. AJR 180:363–368
Sakai T, Sugano N, Ohzono K et al (1998) MRI evaluation of steroid- or alcohol-related osteonecrosis of the femoral condyle. Acta Orthop Scand 69:598–602
Korholz D, Bruder M, Engelbrecht V et al (1998) Aseptic osteonecrosis in children with acute lymphoblastic leukemia. Pediatr Hematol Oncol 15:307–315
Mont MA, Baumgarten KM, Rifai A et al (2000) Atraumatic osteonecrosis of the knee. J Bone Joint Surg Am 82:1279–1290
Porter RP, Kaste SC (2004) Imaging findings of recurrent acute lymphoblastic leukemia in children and young adults, with emphasis on MRI. Pediatr Radiol 34:400–408
Benz-Bohm G, Gross-Fengels W, Bohndorf K et al (1990) MRI of the knee region in leukemic children. Part II. Follow-up: responder, non-responder, relapse. Pediatr Radiol 20:272–276
Bernbeck B, Christaras A, Krauth K et al (2004) Bone marrow oedema and aseptic osteonecrosis in children and adolescents with acute lymphoblastic leukaemia or non-Hodgkin-lymphoma treated with hyperbaric-oxygen-therapy (HBO): an approach to cure? – BME/AON and hyperbaric oxygen therapy as a treatment modality. Klin Padiatr 216:370–378
Karimova EJ, Rai SN, Deng X et al (2006) MRI of knee osteonecrosis in children with leukemia and lymphoma: part 1, observer agreement. AJR 186:470–476
Ojala AE, Paakko E, Lanning FP et al (1998) Bone marrow changes on MRI in children with acute lymphoblastic leukaemia 5 years after treatment. Clin Radiol 53:131–136
Koo KH, Ahn IO, Kim R et al (1999) Bone marrow edema and associated pain in early stage osteonecrosis of the femoral head: prospective study with serial MR images. Radiology 213:715–722
Huang GS, Chan WP, Chang YC et al (2003) MR imaging of bone marrow edema and joint effusion in patients with osteonecrosis of the femoral head: relationship to pain. AJR 181:545–549
Kim YM, Oh HC, Kim HJ (2000) The pattern of bone marrow oedema on MRI in osteonecrosis of the femoral head. J Bone Joint Surg Br 82:837–841
Lecouvet FE, Malghem J, Maldague BE et al (2005) MR imaging of epiphyseal lesions of the knee: current concepts, challenges, and controversies. Radiol Clin North Am 43:655–672
Acknowledgements
We thank Sharon Naron for her editorial assistance. This work was supported by the American Lebanese Syrian Associated Charities (ALSAC), a Center of Excellence grant from the State of Tennessee, and by grants RO1-CA20180 and P30-CA21765 from the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Karimova, E.J., Kaste, S.C. MR imaging of osteonecrosis of the knee in children with acute lymphocytic leukemia. Pediatr Radiol 37, 1140–1146 (2007). https://doi.org/10.1007/s00247-007-0579-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-007-0579-x