Abstract
Bone marrow lesions (BMLs) around the knee are a common magnetic resonance imaging (MRI) finding. However, despite the growing interest on BMLs in multiple pathological conditions, they remain controversial not only for the still unknown role in the etiopathological processes, but also in terms of clinical impact and treatment. The differential diagnosis includes a wide range of conditions: traumatic contusion and fractures, cyst formation and erosions, hematopoietic and infiltrated marrow, developmental chondroses, disuse and overuse, transient bone marrow oedema syndrome and, lastly, subchondral insufficiency fractures and true osteonecrosis. Regardless the heterogeneous spectrum of these pathologies, a key factor for patient management is the distinction between reversible and irreversible conditions. To this regard, MRI plays a major role, leading to the correct diagnosis based on recognizable typical patterns that have to be considered together with coexistent abnormalities, age, and clinical history. Several treatment options have been proposed, from conservative to surgical approaches. In this manuscript the main lesion patterns and their management have been analysed to provide the most updated evidence for the differential diagnosis and the most effective treatment.
Level of evidence IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bone marrow lesions (BMLs) around the knee are a common magnetic resonance imaging (MRI) finding. BML describes an alteration of bone marrow signal intensity, with high signal on fluid-sensitive sequences [T2/proton density with fat suppression and short tau inversion recovery (STIR)] with or without low T1WI signal. These MRI alterations may correspond histologically to true oedema, but also to trabecular necrosis, cysts, fibrosis, and cartilage fragments. Therefore, instead of the commonly used term “bone marrow oedema”, the expressions “bone marrow oedema-like signal” or “BMLs” are more appropriate [89].
Despite the growing interest on BML in multiple pathological conditions, this remains a controversial condition not only for its still unknown role in the etiopathological processes, but also in terms of clinical impact and treatment.
BML can originate from subchondral or non-subchondral bone. This article will focus specifically on subchondral lesions, or lesions that are not subchondral in origin but which can extend to the articular surface, describing the most updated available evidence on the different pathological conditions and providing a comprehensive classification, with indications on their management to preserve joint function.
Classification of subchondral bone marrow oedema-like lesions in the knee
Subchondral bone marrow oedema-like lesions around the knee can be classified into traumatic or non-traumatic, and into reversible or irreversible.
The differential diagnosis includes a wide range of conditions: traumatic contusion and fractures, cyst formation and erosions, hematopoietic and infiltrated marrow, developmental chondroses, disuse and overuse, transient bone marrow oedema syndrome and, lastly, subchondral insufficiency fractures and true osteonecrosis. The role of MRI is to lead to the correct diagnosis based on recognizable typical patterns even at early stages. These patterns rely on location, coexistent abnormalities, age and clinical history (Table 1).
Traumatic subchondral lesions
Bone contusions typically present as reversible oedema-like lesions, with indistinct margins that resolve within 2–4 months. Contusions can be of compressive or tensile type.
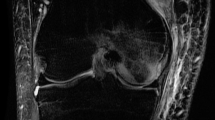
The most common subchondral contusions are those seen after pivot shift injuries and can represent secondary signs of anterior cruciate ligament (ACL) tear. They are commonly observed in the lateral femoral condyle (LFC) around the sulcus, in the posterior aspect of the lateral tibial plateau and also in the posterior aspect of the medial femoral condyle (MFC) (Figs. 1, 2) [8]. Hyperextension injuries, which lead to posterior cruciate ligament (PCL) tear, cause anterior subchondral contusions in the anterior tibia and femur [74].
A sagittal T2 fat suppressed image shows the classical contusion of a pivot shift injury. The femoral contusion is located in the lateral femoral condyle around the sulcus (arrow), and the tibial contusion is located in the posterior aspect of the lateral femoral condyle (dotted arrow). There is also hemarthrosis with a fluid–fluid level (black arrowheads)
Another patient with an anterior cruciate ligament tear. a Sagittal proton density fat suppressed image shows a deep sulcus sign in the lateral femoral condyle surrounded by an impaction contusion (arrow). There are contusions in the anterior and posterior lateral tibial plateau (dotted arrow) and in the fibular head (arrowhead). b An anterior cruciate ligament mid-substance tear is seen on proton density sagittal image (arrow)
In children with open physes, the ACL is typically avulsed from the tibia, with or without an egg-shell cortical fragment, and a resultant traction contusion is usually seen in the tibia [64]. Another age-location specific pattern, seen in teenagers around the physeal closure, is related to spontaneously reduced lateral patellar dislocation, which presents one or a combination of the following findings: impaction contusion in the anterior LFC, a kissing impaction in the medial patellar facet or the median ridge, a medial patella traction contusion of the medial retinaculum (Fig. 3) [69], and an osteochondral grade 4–5 defect in the LFC associated with a sequestered intraarticular fragment (Fig. 4).
A 15-year-old boy with a spontaneously reduced lateral patellar dislocation. Typical contusions are seen on axial proton density fat suppression. There is an impaction contusion in the anterior aspect of the lateral femoral condyle and a contusion in the medial patella (arrows). There is also an increased amount of joint effusion (asterisk)
Degenerative cartilage lesions and OA-associated BML
Oedema-like-signal is commonly visualized in early and advanced OA. It can be associated with thinning of the cartilage with or without the presence of meniscus tear and extrusion, and with or without an observed focal cartilage defect (Fig. 5). The signal alteration can precede the cartilage defect formation. High signal at the periphery of the medial tibial plateau (MTP) and MFC, sometimes subtle, seen in association with peripheral cartilage thinning and meniscus tears, can progress in the future into a cyst [13]. If a well-defined low T1W signal is also present, it represents a process of subchondral cyst formation [6, 13]. Conversely, when a less-defined low T1 signal is present, it may be difficult and even impossible to differentiate from an insufficiency fracture or osteonecrosis, which will be described later in the article.
Osteoarthritis related bone marrow oedema-like signal. Sagittal (a) and coronal (b) proton-density with fat suppression show high signal in the subchondral bone (white arrows) and an underlying cartilage defect (dotted arrow). On sagittal PD without fat suppression (c) the signal is dark, likely representing an early stage of subchondral cyst formation. Another area of subchondral marrow oedema is noted on the coronal image (arrowhead) with an underlying cartilage defect not seen on this image
Transient bone marrow oedema syndrome, subchondral insufficiency fractures (SIFK), spontaneous osteonecrosis of the knee (SONK), and avascular necrosis (AVN)
The spectrum of these pathologies includes reversible and irreversible conditions. There are three transient conditions: transient osteoporosis (TOP), regional migratory osteoporosis (RMO) and complex regional pain syndrome (CRPS), also known as reflex sympathetic dystrophy (RSD) and algodystrophy. On the other side of the spectrum are the irreversible conditions: spontaneous osteonecrosis of the knee (SONK) or avascular necrosis (AVN). Among these, insufficiency fractures (SIFK) can be found. An overlap between these conditions is also likely.
All transient conditions have a similar MRI presentation of diffuse subchondral-bone marrow high signal with indistinct margins, involving but preserving the articular surface. Age, gender, and clinical history are important to distinguish between the three diagnoses: TOP is typically seen in the femoral head during pregnancy and in peripartum women [34]. RMO migrates in different joints including hips, knees, and metatarsal head of middle-aged men over the course of weeks–years. However, TOP can progress to RMO and in some cases to insufficiency fracture. CRPS occurs after an initiator, which can be a major or a minor traumatic injury or pain including meniscal tears and arthroscopy.
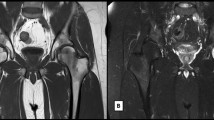
SONK has been used to describe a clinical entity affecting predominantly females in the 7th decade and patients with meniscal pathology, predominantly posterior root tears [67]. Currently, it is believed to have been often misnamed, since this condition may represent a SIFK (a condition of subchondral insufficiency fractures), that in some cases can become irreversible if the subchondral fragment undergoes true necrosis [65, 86]. In the acute stage, there is a marked non-defined oedema-like signal that is more extensive compared to the pattern secondary to cartilage loss [76]. The lack of additional subchondral changes is predictive of reversibility, while the presence of a subchondral area of low T1WI signal >4 mm thick strongly predicts irreversibility (Fig. 6) [38]. The differential diagnosis may be challenging. Bone infarcts in other locations and underlying systemic conditions can help to distinguish AVN (Fig. 7) from SIFK related osteonecrosis (SONK). Prior imaging can also help in distinguishing whether the underlying cause of an oedema-like signal, associated with an overlying cartilage abnormality, is determined by OA or prior SIFK.
Spontaneous insufficiency fractures of the medial and lateral femoral condyles at different stages. Sagittal (a) and coronal (b) fluid-sensitive sequences. There is a subchondral fracture in the medial femoral condyle (arrows) surrounded by oedema. There is more extensive bone marrow oedema in the lateral femoral condyle without a subchondral fracture. The insufficiency fracture of the medial condyle is resolving. The one in the lateral condyle is acute. Also note the extensive soft tissue oedema
Avascular necrosis of the lateral femoral condyle in a patient under steroid treatment. On the sagittal and coronal PD with and without fat suppression (b, d, and a, c respectively), there is a serpiginous lesion surrounded by the characteristic double-line sign of both low and high signal. There is no surrounding BML, indicating that this is a non-acute lesion
Post cartilage surgery BML
Perifocal BML may be observed after focal cartilage treatment (e.g. microfractures, autologous chondrocyte implantation (ACI), osteochondral autograft transplantation, osteochondral scaffold implantation, etc.). BMLs are detectable around and above the treated site, usually together with the signs of the surgical procedure itself, without other distinctive aspects (Fig. 8) [68].
The prevalence of these lesions, their evolution, and their prognosis are related to the specific cartilage procedure, but their clinical significance is still unclear [44].
Other types of BML
Subchondral bone erosions
Erosions can occur in the setting of systemic or localized synovitis. Inflammatory arthritis (rheumatoid, psoriasis, ankylosing spondylitis, reactive etc.) may have the same MRI appearance; thus, the clinical history and laboratory tests play an important role for specify correct diagnosis. Pigmented villonodular synovitis (PVNS) can appear as a focal soft tissue lesion in the joint space, with adjacent focal pressure erosions, or as more diffuse synovitis. Other causes for pressure erosions include synovial chondromatosis and even meniscal cysts [7, 73]. Characteristic in PVNS, but also seen in haemophilia, is the low T2 signal and the blooming artefact seen mostly on gradient echo sequences from the hemosiderin deposition in the synovium (Fig. 9). In general, erosions show low T1 signal with sharp margins at the periphery and demonstrate enhancement after intravenous injection of gadolinium. They may be surrounded by oedema-like signal on fluid-sensitive sequences. In inflammatory disease, erosions usually occur at tight recesses [32, 57]. More subtle differential diagnosis among types of arthritis has been reported in the literature [23]. BML also plays a prognostic role in rheumatoid arthritis, since it has been shown to be the strongest of many conventional and imaging biomarkers for prediction of erosive progression as well as an aggressive rheumatoid arthritis phenotype associated with functional decline [49].
Hematopoietic (red) and infiltrated marrow
Red marrow and bone marrow infiltration do not usually involve the subchondral bone, but they can be seen close to or extend to it. Although the first is considered normal and the second is concerning for severe illness such as lymphoma, giant cell tumour and even osteosarcoma, they can both have a similar appearance on fluid-sensitive sequences. However, T1 WI and gradient-echo in-phase and out-of-phase provide the specificity, while red marrow demonstrates low-T1-signal that is higher than the adjacent muscle, infiltrated marrow is iso- or hypo-intense to muscle (Fig. 10) [81]. While the signal of hematopoietic marrow drops on gradient echo out-of-phase, there is no significant change in marrow infiltration [15].
Bone marrow lesion related to disuse
Subchondral oedema-like signal related to disuse is most prominent 10–25 weeks following immobilization. Dot-like or linear patterns and involvement of multiple bones in the knee can direct to this diagnosis (Fig. 11) [56]. The high signal is usually less intense than in the other conditions.
Histopathological findings
As already mentioned, BML shown by MRI imaging results from various aetiologies affecting the subchondral bone and reflects a multitude of histopathological findings.
Histopathological findings following trauma
Subchondral bone injuries following a single direct impact or resulting from repetitive microtrauma show peculiar histopathological features. The underlying bone is locally impacted, showing (micro) fractures of the subarticular spongiosa with osteocyte necrosis and empty lacunae, haemorrhage and oedema [66]. These findings correspond to the MRI pattern of impaction contusion.
In some cases, in the course of bone remodelling, subchondral bone becomes stiffer and signs of early OA may appear. The cartilage overlying such areas is also directly affected. Chondrocyte apoptosis and necrosis, chondrocyte proliferation, and loss of superficial proteoglycans—all signs of early OA—may be present [55].
If the traumatic impact is more severe, a subchondral fracture may cause a local depression and collapse of the cartilage surface. Fractures affecting the osteochondral unit (either with a chondral or osteochondral fragment or purely subchondral) may show accompanying BMLs. While chondral defects do not heal spontaneously, osteochondral defects undergo a well-defined sequence of spontaneous osteochondral repair, based on a blood clot with pluripotent undifferentiated mesenchymal cells that differentiate into chondrocytes and osteoblasts, forming an osteochondral repair tissue [41].
Histopathological findings in BML associated with OA
Changes of subchondral bone are a classic feature of OA. These usually occur in the affected articular region, indicating bone remodelling. Increased thickness and mineral density of the subarticular trabeculae induces early OA [60]. Other characteristic processes include microcracks, micro-oedema, microbleeding within the subchondral region, as well as subchondral bone cysts [41].
Histopathological findings in the course of SIFK/SONK/AVN
Ischaemic events and/or trabecular microcracks contribute to the evolution of subchondral alterations and may result in focal osteonecrosis of subchondral bone. If the injury leads to an irreversible damage, marrow cells and vessels may show evidence of necrosis just after few days. Osteocytes become necrotic within few weeks. The necrotic tissue is being removed and replaced by newly formed trabecular bone in the subarticular spongiosa by creeping substitution. There may be a sclerotic rim at the interface between the necrotic zone and the surrounding viable subchondral bone. In later stages, this bone sequestrum is often associated with subchondral insufficiency fracture presenting as thin, disconnected subarticular trabeculae [41]. These fractures may not be associated with any fracture callus, as bone is necrotic. This entire subchondral region may collapse, and cause depression and fragmentation of the previously intact and viable articular surface.
Histopathological findings post cartilage surgery
The upward migration of the subchondral bone plate, formation of intralesional osteophytes, and subchondral bone cysts are specific subchondral bone alterations following reconstructive cartilage repair procedures [59]. Deteriorations of the subchondral microarchitecture such as changes in bone mineral density, bone volume, and trabecular thickness were also reported, suggesting that the entire osteochondral unit can be altered after cartilage surgery [61].
Aetiology and evolution
Trauma-associated BML
Trauma-induced BML can be differentiated into lesions associated with acute trauma, i.e. bone contusion, and subacute lesions as a result of overload, i.e. repetitive microtrauma with physical activity [68]. These types of BML are strictly related to trauma mechanism and force, and they are often associated with knee ligament tears. In ACL tears, the characteristic BML localization can be a result of a valgus stress on the knee with the femur in external rotation relative to a fixed tibia and this explains why the lateral compartment is more involved than the medial one [9]. However, Major and Helms also demonstrated the presence of BML in preseason in 41 % of asymptomatic collegiate basketball players subject to repetitive microtrauma [42].
While the aetiology of traumatic BML has been widely analysed, only few authors investigated the long-term evolution of post-traumatic bone contusions. An MRI study in acute knee trauma showed bone contusion in 53 % of the patients. These lesions persist at 4 and 12 months of follow-up in 69 and 12 % of the patients, respectively [9]. However, BML natural history can be influenced by several factors. It has been reported that BML in a complex knee injury with an ACL tear has a slower resolution compared to BML related to an isolated MCL tear, where it spontaneously heals in 2–4 months [51]. This is probably due to the different trauma forces causing the lesion of the ligament. BML in ACL lesion was predominantly present at 3-year follow-up when associated with a disruption or a depression of the normal contour of the femoral cortical surface, while lesions without cortical involvement tended to spontaneous resolution in 95 % of the cases [12]. Site may also play a role, since LFC BML in ACL-injured knees had a quicker resolution compared to lateral tibial BMLs (median 3 vs. 6 months) [25]. Finally, the geographical appearance of the oedema-like signal associated with ACL injury may be predictive of an evolution in osteochondral damage [85].
According to the few studies reported in the literature, there is no agreement on a correlation at short-term follow-up between BML, pain and functional status. It has been suggested that BML may negatively influence pain, functional recovery, and return to previous sport level, especially if the alteration is still detectable 3 months after the injury [22, 31]. Similarly, it still remains unclear if the initial joint injury with BML has a direct relationship to long-term function and OA development. Long-term studies on BML in symptomatic and asymptomatic patients are needed to clarify these potential correlations.
OA-associated BML
The evidence of a higher prevalence of BML in case of overloading, such as in the medial compartment for varus knees or the lateral compartment for valgus knees, strongly supports the hypothesis of a possible role of repeated microtrauma in the genesis of these lesions. An MRI study performed on a healthy population, with a temporary artificial malalignment of the mechanical axis (overpronation of one foot), showed a diffuse increase in BML [71]. It has also been hypothesized that venous stasis can cause an intraosseous hypertension and, consequently, bone hypoperfusion and hypoxia, leading to BML [43].
The evolution of BML in OA is extremely variable, since different studies showed that this kind of lesion can develop, fluctuate in size, and regress, while in the Multicenter Osteoarthritis Knee Study the majority of subchondral lesions regressed or resolved completely at 30-month follow-up [68], in the Dutch Genetics Arthrosis and Progression study only 20 % of the marrow lesions decreased or resolved after 2 years [35]. The healing rate was even lower in the Boston Osteoarthritis Knee Study, where it is reported that <1 % of the patients showed a decrease in BML size after 30 months [29]. Roemer et al. [68] observed that the enlargement of BML is a negative prognostic factor for cartilage loss, pain, and predictive for arthroplasty. Tanamas et al. [77] confirmed these data and noted that the severity of BML was positively associated with the risk of knee joint replacement over 4 years. Scher et al. [70] reported that subjects with BME were 8.95 times more likely to progress rapidly to arthroplasty when compared to subjects with no BME.
Prognostic factors for BML increase are male sex, elevated BMI, and pain [70]. However, the correlation between BML and pain is still under debate: a systematic review assessing the sources of pain in knee OA found a moderate evidence for an association between BML and pain, with four high-quality studies versus one demonstrating a positive association [88]. Felson et al. [20] reported that knee pain is correlated with the development of BML or enlargement of pre-existing lesions.
SIFK/SONK/AVN
Osteonecrosis of the knee was first described by Ahlback et al. [2]. The knee is the second most common affected location, following the hip [52]. Three distinct categories of osteonecrosis have been identified: SONK, AVN, and post-arthroscopic osteonecrosis.
SIFK related osteonecrosis (SONK) is considered to be the most common form, albeit few epidemiologic data exist. Only one study indicates a 3.4 % incidence in patients aged over 50 years and an incidence ≤9.4 % in patients older than 65 years [62]. AVN (osteonecrosis mainly ascribable to ischaemic events) usually affects male patients younger than 45 years. It can be related to a history of trauma or can be secondary to systemic diseases, chemotherapy, radiation, alcohol abuse, corticosteroids use and smoking. Post-arthroscopic osteonecrosis is the rarest form, with no age or sex preference, and it is more common after meniscectomy, radiofrequency-assisted surgery, and cartilage debridement [53].
SONK is classically described as a focal, superficial subchondral lesion, mainly affecting the MFC. It is rarely a bilateral condition (<5 %), and female patients are more commonly affected although some MRI studies showed equal prevalence among males and females [38]. Patients usually complain of a medial-sided acute knee pain, which worsens at night. Typically the patients do not report a history of trauma or risk factors. Aetiology is still not completely understood. Two aetiologic hypotheses have been reported. A vascular origin was initially suggested, with compromised microcirculation to the subchondral bone resulting in oedema, increased intraosseous pressure, finally leading to ischaemia and necrosis [33]. However, the evidence is at best limited to histological findings from a very small number of studies suggesting abnormal vascularity, oedema and increased focal bone turnover [63]. Subsequently, SONK has been associated with SIFK once the subchondral fragment undergoes true necrosis. SIFK are non-traumatic fractures, and they are usually occurring in elderly, female, overweight and osteoporotic patients. Once subchondral fractures occur and fail to heal, repetitive micromotion of the unstable osteochondral portion can lead to infiltration of synovial fluid into the fracture site, detachment and fragmentation of the osteochondral fragment, followed by osteonecrotic changes in the disconnected lesion [86].
The reported clinical course can be unpredictable. SIFK does not necessarily progress in every patient. Sometimes, reparative mechanisms with new bone formation can occur and avoid bone death. The duration of symptoms is variable and depends on the initial severity and extent of bone involvement. Typically, the initial phase consists in severe pain with functional impairment for at least 3–6 months, followed by spontaneous resolution with functional and radiographic improvement [80]. Alternatively, clinical progression of severe symptoms and radiological evidence of subchondral bone collapse can occur.
Post cartilage surgery
The increasing awareness on the role played by BMLs in the homoeostasis of the osteochondral unit recently led to investigate the meaning of such MRI findings also in patients who underwent cartilage treatments [44].
Bone marrow oedema-like signals are frequent findings after both chondral and osteochondral surgical procedures, with a reported rate ranging from about 40 to 80 %. Takahashi et al. [75] evaluating 41 patients treated with ACI for femoral condyle lesions, demonstrated that BMLs can be present even before treatment, but that they can also be caused by the treatment itself, with a 47 % rate at 1 year after surgery. Niethammer et al. [58] prospectively documented BMLs presence after third-generation ACI with serial MRIs of 38 knees up to 36 months of follow-up. BMLs were seen in 78.9 % of the defects over the postoperative course and were more common in femoral than patellar defects. Other authors evaluated MRI findings after ACI surgery detecting BMLs in about half of the cases at short-term follow-up [14, 27, 79]. The same percentage was confirmed at longer follow-up. Tetta et al. [78] evaluated 40 chondral lesions of the femoral condyles or trochlea treated with hyaluronic acid-based MACT. At 5- to 7-year follow-up, the prevalence of MRIs presenting BMLs was 50 %. Finally, Vasiliadis et al. [84] documented the persistence of subchondral bone changes also at the long-term evaluation at 13 years in 36 knees treated with ACI: 59 % still showed oedema-like signals.
The etiopathology and clinical significance of these findings remain nebulous, and also the significance of post-surgical BMLs evolution is not clear, since there is evidence of both reduction and increase over time. In the attempt to clarify the evolution of BMLs found after cartilage surgery, Filardo et al. [21] evaluated 248 MRIs performed from 6 to 108 months after hyaluronic acid-based ACI. BMLs were present in the first postoperative phases, markedly reduced at 2 and 3 years, and then again increased and steadily present at mid/long-term follow-up. This peculiar evolution trend could be the expression of tissue modifications over time: the initial reduction could be due to the maturation phase, which for such cartilage treatments is commonly acknowledged to stabilize at around 2 years, resulting in a reduction of the MRI signal. On the other hand, the hyaline-like cartilage found as a result of ACI procedures may be not sufficient to protect subchondral bone from mechanical forces and thus lead to progressive subchondral bone stimulation. The importance of the abnormal load applied seems to be supported by the distribution of BML, more common in femoral condyles than in trochlea and patellae, or in joint compartments with combined meniscus damage and therefore further increased abnormal mechanical stress.
Despite the aforementioned studies shedding some light on frequency and evolution, no correlation has been found between BMLs and clinical outcome, thus making the clinical significance of this imaging finding questionable [21, 58, 75]. The high MRI sensitivity may allow early changes to be detected, which may be a tissue reaction that is abnormal but still not severe enough to affect the clinical outcome, even at mid/long-term follow-up.
Nonetheless, BMLs are common finding after cartilage surgery, and a better understanding of the evolution of post-surgical BML over time is needed, as well as its importance as a prognostic factor over time, to better evaluate the potential of cartilage procedures and improve the management of patients undergoing surgery for the treatment of the articular surface.
Conservative treatment
Physical treatment
Patients suffering from SIFK related osteonecrosis (SONK) or other BML-related conditions may be managed non-operatively or operatively, based on symptoms and disease staging. The decision is largely based on the aetiology and on the size and grading of the osteonecrotic area. This can be calculated by measuring the greatest width both in anterior-posterior and lateral radiographs [33], or as a percentage of the affected femoral condyle [39]. Osteonecrosis areas involving more than 40–50 % of the condyle or lesions bigger than 5 cm2 usually lead to collapse and require prosthetic arthroplasty [1, 53].
Conversely, medium lesions (3.5–5.0 cm2) may or may not regress, and small lesions (typically <3.5 cm2) usually regress with non-surgical management. Thus, non-operative management is usually reserved for small BML (<3.5 cm2) without clear signs of osteonecrosis [33]. The conservative approach includes treatment with non-steroidal anti-inflammatory drugs (NSAIDs), analgesics as needed, and protected weight bearing for 3–8 months, based on patients symptoms and radiological control [33, 87].
Another area of non-operative management currently being studied is pulsed electromagnetic fields therapy. In a case series of patients affected by early SONK stage, pulsed electromagnetic fields significantly reduced pain and size of the necrotic lesion after 6 months [46].
Pharmacological
Two drugs have been proposed and studied for the treatment of BML: prostacyclin and bisphosphonate. They act on different bone targets, and therefore they may interact with different steps of the etiopathological pattern of BML.
The most studied prostacyclin analogue is iloprost (Schering AG, Berlin, Germany), whose pharmacokinetic effects lead to better perfusion in tissues with a critical blood supply. It induces vasodilation and has an impact on the rheological properties of the terminal vascular bed [26]. Moreover, it reduces capillary permeability, inhibits platelet aggregation and diminishes the concentration of free oxygen radicals and leukotrienes [3, 10, 16, 17]. However, the pharmacological effects that are responsible for pain relief and the decrease in BML are not yet known. It is unclear if the pain relief and reduction of BML during and after iloprost application are primarily based on a normalization of intraosseous pressure or on interactions with local leukotrienes and cytokines [30]. Nonetheless, the effects of iloprost in treating BML were proved by several clinical studies at short-term follow-up, with lesions regression and symptoms improvement [47, 48], but with poorer results in advanced stages [30].
The second drug proposed for the treatment of BML, bisphosphonate, inhibits osteoclast activity and consequently bone resorption. The rationale for the use of bisphosphonates in the treatment of BML and early, precollapse stage osteonecrosis, is based on the assumption that the structural bone failure is the result of resorption of necrotic bone during revascularization before new bone has been formed. It can be hypothesized that if accelerated bone resorption could be reduced during the revascularization process, until sufficient new bone has been formed, structural failure could be avoided [50]. Clinical results of bisphosphonate treatment for BML and subchondral pathology are controversial. In the only randomized, double-blind, placebo-controlled trial on knee osteonecrosis, Meier et al. [50] failed to find any differences between ibandronate and placebo. On the other hand, other studies showed clinical and radiological benefit from bisphosphonate treatment in osteonecrosis [36], in transient bone marrow lesion syndrome and in CRPS [5, 82]. Bisphosphonates were also recently applied with a different indication: early OA, with evidence of reduced knee pain and BML size, which suggests that OA treatment may benefit from this specific therapeutic approach [37, 83].
In the only trial comparing the effect of prostacyclin and bisphosphonate IV in treatment of BML of the knee and foot, with 10 patients per arms, Baier et al. [4] found that both treatments have a therapeutic benefit, allowing symptoms relief and BML reduction on MRI, with a quicker and greater effect of prostacyclin.
Regarding the posology, prostacyclin has been administered both intravenously (0.5–1.0 ng/kg/min 6 h daily for 5 days) [30] and per os (50–100 μg twice or thrice daily for 4 weeks) [48], whereas bisphosphonates have been used intravenously with different dosage for the different drugs (neridronate 100 mg IV four times over 10 days [83], zoledronic acid 5 mg single IV infusion [37], ibandronate 6 mg infusion three times at a monthly interval [5]).
These promising results suggest an attempt of pharmacological treatment with prostacyclin or bisphosphonates for early stage osteonecrosis, as well as in early OA, but further studies are needed in order to clarify posology, indications, and long-term results of these drugs.
Surgical treatment
Classifications may create artificial separations, yet are useful for choosing treatment options, especially when considering surgical intervention. Only lesions candidate for surgery will be discussed in this section.
Microscopic trabecular fractures may be associated with macro (e.g. impaction injuries associate with the tibiofemoral subluxation of an ACL tear or patellar dislocation) or microtrauma (e.g. stress fracture) [89], but it is also important to consider that microtrabecular fractures can be associated with altered loads of bone, ranging from loss of meniscal function to loss of the protective function of articular cartilage, whether from OA or inadequate function of a cartilage restoration procedure. Finally, ischaemic events should be considered. With these various pathogenetic patterns in mind, if nonoperative treatment fails, operative treatments may be divided into two nonexclusive broad categories: those stabilizing the microtrabecular fractures and those encouraging a healing response.
Stabilization of microtrabecular fractures
Sharkey et al. [72] proposed flowable calcium phosphate that could endothermically crystalize without displacing the trabeculae to stabilize microtrabecular fractures in OA patients, first applying polymethylmethacrylate and then calcium phosphate (Figs. 12, 13, 14). Pain improvement and a delayed arthroplasty in the treated patients were reported. A recent publication by Colon et al. [11] pointed out that not all commercially available bone substitute materials are able to flow in a closed fracture environment without damaging the bone structure, thus suggesting the importance of the material choice. Recently, extended indications have been proposed for the treatment of knee BML areas, but the utility of these procedures remain under evaluation, also considering some reported complications in the preliminary experiences [19] .
a Intraoperative fluoroscopy view of cannula insertion prior to calcium phosphate injection. Precise location achieved through triangulation from coronal and sagittal planes on preoperative MRI and transferred to AP and true lateral views fluoroscopically. b Postoperative fluoroscopy view showing calcium phosphate blush in the region of bone marrow lesion
A high incidence of BML after cartilage treatment has been reported [21]. This appears to occur after all types of cartilage procedures and may represent a benign bone cartilage construct interaction or the beginning of a process of pathologic bone overload. Calcium phosphate injections have been recently proposed also to improve patient comfort and potentially avert progression to delamination by treating these lesions [18].
When insufficiency fractures progress to a bone structure collapse, subchondral support techniques are inadequate and thus the treatment of choice should be bone grafting of the injured and deficient bone, followed by osteochondral restoration [45, 54].
Stimulation of a healing response
As an alternative for a ceramic support (calcium phosphate crystallizes to hydroxyapatite) another approach is to stimulate healing before a collapse occurs. Treatment of osteonecrosis has typically involved core decompression [24]. Future trends may involve the use of bone marrow concentrate as augmentation of core decompression, borrowing a treatment already used and studied in the hip. In the subchondral bone pathology of the femoral head, this combined treatment has shown promising results in the past few years. Treating 534 hips with early stages of osteonecrosis, Hernigou et al. [28] demonstrated that only 94 hips progressed to collapse and needed a total hip replacement after a mean 13 years after core decompression with bone marrow grafting. Moreover, randomized trials were also performed, showing how core decompression augmented with bone marrow concentrate improved bone healing rates when compared to core decompression alone [40].
Conclusions
BML can be found in a wide range of conditions. The key factor for patient management is the distinction between reversible and irreversible conditions. MRI plays a major role for a correct diagnosis based on recognizable typical patterns that have to be considered together with coexistent abnormalities, age, and clinical history. Several conservative and surgical treatment options have been proposed, but with an overall weak literature support. Future studies should focus on BML to better define specific pathologic patterns, allowing a more accurate differential diagnosis and precise indications for the available and new therapies. Finally, high-level studies should prove the potential of each treatment according to the specific pathology and disease phase, in order to optimize the management of BML.
References
Aglietti P, Insall JN, Buzzi R, Deschamps G (1983) Idiopathic osteonecrosis of the knee. Aetiology, prognosis and treatment. J Bone Joint Surg Br 65(5):588–597
Ahlback S, Bauer GC, Bohne WH (1968) Spontaneous osteonecrosis of the knee. Arthritis Rheum 11(6):705–733
Aktan AO, Buyukgebiz O, Yegen C, Yalcin SH, Haklar G, Yalin R, Ercan S (1994) Does PGE2 act as a mediator for endothelin release? Prostaglandins Leukot Essent Fatty Acids 50(1):37–41
Baier C, Schaumburger J, Gotz J, Heers G, Schmidt T, Grifka J, Beckmann J (2013) Bisphosphonates or prostacyclin in the treatment of bone-marrow oedema syndrome of the knee and foot. Rheumatol Int 33(6):1397–1402
Bartl C, Imhoff A, Bartl R (2012) Treatment of bone marrow edema syndrome with intravenous ibandronate. Arch Orthop Trauma Surg 132(12):1781–1788
Bergman A, Brandt I, Darnerud PO, Wachtmeister CA (1982) Metabolism of 2,2′,5,5′-tetrachlorobiphenyl: formation of mono- and bis-methyl sulphone metabolites with a selective affinity for the lung and kidney tissues in mice. Xenobiotica 12(1):1–7
Blair TR, Schweitzer M, Resnick D (1999) Meniscal cysts causing bone erosion: retrospective analysis of seven cases. Clin Imaging 23(2):134–138
Brandser EA, Riley MA, Berbaum KS, El-Khoury GY, Bennett DL (1996) MR imaging of anterior cruciate ligament injury: independent value of primary and secondary signs. Am J Roentgenol (AJR) 167(1):121–126
Bretlau T, Tuxoe J, Larsen L, Jorgensen U, Thomsen HS, Lausten GS (2002) Bone bruise in the acutely injured knee. Knee Surg Sports Traumatol Arthrosc 10(2):96–101
Buyukgebiz O, Aktan AO, Yegen C, Yalcin AS, Haklar G, Yalin R, Ercan ZS (1994) Captopril increases endothelin serum concentrations and preserves intestinal mucosa after mesenteric ischemia-reperfusion injury. Res Exp Med 194(6):339–348
Colon DA, Yoon BJ, Russell TA, Cammisa FP, Abjornson C (2015) Assessment of the injection behavior of commercially available bone BSMs for Subchondroplasty® procedures. Knee 22(6):597–603
Costa-Paz M, Muscolo DL, Ayerza M, Makino A, Aponte-Tinao L (2001) Magnetic resonance imaging follow-up study of bone bruises associated with anterior cruciate ligament ruptures. Arthroscopy 17(5):445–449
Crema MD, Roemer FW, Zhu Y, Marra MD, Niu J, Zhang Y, Lynch JA, Javaid MK, Lewis CE, El-Khoury GY, Felson DT, Guermazi A (2010) Subchondral cystlike lesions develop longitudinally in areas of bone marrow edema-like lesions in patients with or at risk for knee osteoarthritis: detection with MR imaging—the MOST study. Radiology 256(3):855–862
Dhollander AA, Huysse WC, Verdonk PC, Verstraete KL, Verdonk R, Verbruggen G, Almqvist KF (2010) MRI evaluation of a new scaffold-based allogenic chondrocyte implantation for cartilage repair. Eur J Radiol 75(1):72–81
Disler DG, McCauley TR, Ratner LM, Kesack CD, Cooper JA (1997) In-phase and out-of-phase MR imaging of bone marrow: prediction of neoplasia based on the detection of coexistent fat and water. Am J Roentgenol (AJR) 169(5):1439–1447
Erlansson M, Bergqvist D, Persson NH, Svensjo E (1991) Modification of postischemic increase of leukocyte adhesion and vascular permeability in the hamster by iloprost. Prostaglandins 41(2):157–168
Erlansson M, Svensjo E, Bergqvist D (1989) Leukotriene B4-induced permeability increase in postcapillary venules and its inhibition by three different antiinflammatory drugs. Inflammation 13(6):693–705
Farr J (2013) Treatment of subchondral bone pathology. In: Paper presented at the ICRS World Congress, Izmir, Turkey
Farr J, Cohen SB (2013) Expanding applications of the subchondroplasty procedure for the treatment of bone marrow lesions observed on magnetic resonance imaging. Oper Tech Sports Med 21(2):138–143
Felson DT, Niu J, Guermazi A, Roemer F, Aliabadi P, Clancy M, Torner J, Lewis CE, Nevitt MC (2007) Correlation of the development of knee pain with enlarging bone marrow lesions on magnetic resonance imaging. Arthritis Rheum 56(9):2986–2992
Filardo G, Kon E, Di Martino A, Perdisa F, Busacca M, Tentoni F, Balboni F, Marcacci M (2014) Is the clinical outcome after cartilage treatment affected by subchondral bone edema? Knee Surg Sports Traumatol Arthrosc 22(6):1337–1344
Filardo G, Kon E, Tentoni F, Andriolo L, Di Martino A, Busacca M, Di Matteo B, Marcacci M (2016) Anterior cruciate ligament injury: post-traumatic bone marrow oedema correlates with long-term prognosis. Int Orthop 40(1):183–190
Flemming DJ, Hash TW 2nd, Bernard SA, Brian PS (2014) MR imaging assessment of arthritis of the knee. Magn Reson Imaging Clin N Am 22(4):703–724
Forst J, Forst R, Heller KD, Adam G (1998) Spontaneous osteonecrosis of the femoral condyle: causal treatment by early core decompression. Arch Orthop Trauma Surg 117(1–2):18–22
Frobell RB (2011) Change in cartilage thickness, posttraumatic bone marrow lesions, and joint fluid volumes after acute ACL disruption: a two-year prospective MRI study of sixty-one subjects. J Bone Joint Surg Am 93(12):1096–1103
Grant SM, Goa KL (1992) Iloprost. A review of its pharmacodynamic and pharmacokinetic properties, and therapeutic potential in peripheral vascular disease, myocardial ischaemia and extracorporeal circulation procedures. Drugs 43(6):889–924
Henderson I, Francisco R, Oakes B, Cameron J (2005) Autologous chondrocyte implantation for treatment of focal chondral defects of the knee—a clinical, arthroscopic, MRI and histologic evaluation at 2 years. Knee 12(3):209–216
Hernigou P, Poignard A, Zilber S, Rouard H (2009) Cell therapy of hip osteonecrosis with autologous bone marrow grafting. Indian J Orthop 43(1):40–45
Hunter DJ, Zhang Y, Niu J, Goggins J, Amin S, LaValley MP, Guermazi A, Genant H, Gale D, Felson DT (2006) Increase in bone marrow lesions associated with cartilage loss: a longitudinal magnetic resonance imaging study of knee osteoarthritis. Arthritis Rheum 54(5):1529–1535
Jager M, Tillmann FP, Thornhill TS, Mahmoudi M, Blondin D, Hetzel GR, Zilkens C, Krauspe R (2008) Rationale for prostaglandin I2 in bone marrow oedema—from theory to application. Arthritis Res Ther 10(5):R120
Johnson DL, Bealle DP, Brand JC Jr, Nyland J, Caborn DN (2000) The effect of a geographic lateral bone bruise on knee inflammation after acute anterior cruciate ligament rupture. Am J Sports Med 28(2):152–155
Karchevsky M, Schweitzer ME, Morrison WB, Parellada JA (2004) MRI findings of septic arthritis and associated osteomyelitis in adults. Am J Roentgenol (AJR) 182(1):119–122
Karim AR, Cherian JJ, Jauregui JJ, Pierce T, Mont MA (2015) Osteonecrosis of the knee: review. Ann Transl Med 3(1):6
Klontzas ME, Vassalou EE, Zibis AH, Bintoudi AS, Karantanas AH (2015) MR imaging of transient osteoporosis of the hip: an update on 155 hip joints. Eur J Radiol 84(3):431–436
Kornaat PR, Kloppenburg M, Sharma R, Botha-Scheepers SA, Le Graverand MP, Coene LN, Bloem JL, Watt I (2007) Bone marrow edema-like lesions change in volume in the majority of patients with osteoarthritis; associations with clinical features. Eur Radiol 17(12):3073–3078
Kraenzlin ME, Graf C, Meier C, Kraenzlin C, Friedrich NF (2010) Possible beneficial effect of bisphosphonates in osteonecrosis of the knee. Knee Surg Sports Traumatol Arthrosc 18(12):1638–1644
Laslett LL, Dore DA, Quinn SJ, Boon P, Ryan E, Winzenberg TM, Jones G (2012) Zoledronic acid reduces knee pain and bone marrow lesions over 1 year: a randomised controlled trial. Ann Rheum Dis 71(8):1322–1328
Lecouvet FE, van de Berg BC, Maldague BE, Lebon CJ, Jamart J, Saleh M, Noel H, Malghem J (1998) Early irreversible osteonecrosis versus transient lesions of the femoral condyles: prognostic value of subchondral bone and marrow changes on MR imaging. Am J Roentgenol (AJR) 170(1):71–77
Lotke PA, Abend JA, Ecker ML (1982) The treatment of osteonecrosis of the medial femoral condyle. Clin Orthop Relat Res 171:109–116
Ma Y, Wang T, Liao J, Gu H, Lin X, Jiang Q, Bulsara MK, Zheng M, Zheng Q (2014) Efficacy of autologous bone marrow buffy coat grafting combined with core decompression in patients with avascular necrosis of femoral head: a prospective, double-blinded, randomized, controlled study. Stem Cell Res Ther 5(5):115
Madry H, van Dijk CN, Mueller-Gerbl M (2010) The basic science of the subchondral bone. Knee Surg Sports Traumatol Arthrosc 18(4):419–433
Major NM, Helms CA (2002) MR imaging of the knee: findings in asymptomatic collegiate basketball players. Am J Roentgenol (AJR) 179(3):641–644
Manara M, Varenna M (2014) A clinical overview of bone marrow edema. Reumatismo 66(2):184–196
Marcacci M, Andriolo L, Kon E, Filardo G (2015) Bone marrow edema and results after cartilage repair. Ann Transl Med 3(10):132
Marcacci M, Filardo G, Kon E (2013) Treatment of cartilage lesions: what works and why? Injury 44(Suppl. 1):S11–S15
Marcheggiani Muccioli GM, Grassi A, Setti S, Filardo G, Zambelli L, Bonanzinga T, Rimondi E, Busacca M, Zaffagnini S (2013) Conservative treatment of spontaneous osteonecrosis of the knee in the early stage: pulsed electromagnetic fields therapy. Eur J Radiol 82(3):530–537
Mayerhoefer ME, Kramer J, Breitenseher MJ, Norden C, Vakil-Adli A, Hofmann S, Meizer R, Siedentop H, Landsiedl F, Aigner N (2007) Short-term outcome of painful bone marrow oedema of the knee following oral treatment with iloprost or tramadol: results of an exploratory phase II study of 41 patients. Rheumatology 46(9):1460–1465
Mayerhoefer ME, Kramer J, Breitenseher MJ, Norden C, Vakil-Adli A, Hofmann S, Meizer R, Siedentop H, Landsiedl F, Aigner N (2008) MRI-demonstrated outcome of subchondral stress fractures of the knee after treatment with iloprost or tramadol: observations in 14 patients. Clin J Sport Med 18(4):358–362
McQueen FM (2012) Bone marrow edema and osteitis in rheumatoid arthritis: the imaging perspective. Arthritis Res Ther 14(5):224
Meier C, Kraenzlin C, Friederich NF, Wischer T, Grize L, Meier CR, Kraenzlin ME (2014) Effect of ibandronate on spontaneous osteonecrosis of the knee: a randomized, double-blind, placebo-controlled trial. Osteoporos Int 25(1):359–366
Miller MD, Osborne JR, Gordon WT, Hinkin DT, Brinker MR (1998) The natural history of bone bruises. A prospective study of magnetic resonance imaging-detected trabecular microfractures in patients with isolated medial collateral ligament injuries. Am J Sports Med 26(1):15–19
Mont MA, Baumgarten KM, Rifai A, Bluemke DA, Jones LC, Hungerford DS (2000) Atraumatic osteonecrosis of the knee. J Bone Joint Surg Am 82(9):1279–1290
Mont MA, Marker DR, Zywiel MG, Carrino JA (2011) Osteonecrosis of the knee and related conditions. J Am Acad Orthop Surg 19(8):482–494
Murphy RT, Pennock AT, Bugbee WD (2014) Osteochondral allograft transplantation of the knee in the pediatric and adolescent population. Am J Sports Med 42(3):635–640
Nakamae A, Engebretsen L, Bahr R, Krosshaug T, Ochi M (2006) Natural history of bone bruises after acute knee injury: clinical outcome and histopathological findings. Knee Surg Sports Traumatol Arthrosc 14(12):1252–1258
Nardo L, Sandman DN, Virayavanich W, Zhang L, Souza RB, Steinbach L, Guindani M, Link TM (2013) Bone marrow changes related to disuse. Eur Radiol 23(12):3422–3431
Narvaez JA, Narvaez J, Ortega R, De Lama E, Roca Y, Vidal N (2003) Hypointense synovial lesions on T2-weighted images: differential diagnosis with pathologic correlation. Am J Roentgenol (AJR) 181(3):761–769
Niethammer TR, Valentin S, Gulecyuz MF, Rossbach BP, Ficklscherer A, Pietschmann MF, Muller PE (2015) Bone marrow edema in the knee and its influence on clinical outcome after matrix-based autologous chondrocyte implantation: results after 3-year follow-up. Am J Sports Med 43(5):1172–1179
Orth P, Cucchiarini M, Kohn D, Madry H (2013) Alterations of the subchondral bone in osteochondral repair—translational data and clinical evidence. Eur Cell Mater 25:299–316 (discussion 314–316)
Orth P, Cucchiarini M, Wagenpfeil S, Menger MD, Madry H (2014) PTH [1–34]-induced alterations of the subchondral bone provoke early osteoarthritis. Osteoarthr Cartil 22(6):813–821
Orth P, Goebel L, Wolfram U, Ong MF, Graber S, Kohn D, Cucchiarini M, Ignatius A, Pape D, Madry H (2012) Effect of subchondral drilling on the microarchitecture of subchondral bone: analysis in a large animal model at 6 months. Am J Sports Med 40(4):828–836
Pape D, Seil R, Fritsch E, Rupp S, Kohn D (2002) Prevalence of spontaneous osteonecrosis of the medial femoral condyle in elderly patients. Knee Surg Sports Traumatol Arthrosc 10(4):233–240
Patel S (2014) Primary bone marrow oedema syndromes. Rheumatology 53(5):785–792
Prince JS, Laor T, Bean JA (2005) MRI of anterior cruciate ligament injuries and associated findings in the pediatric knee: changes with skeletal maturation. Am J Roentgenol (AJR) 185(3):756–762
Ramnath RR, Kattapuram SV (2004) MR appearance of SONK-like subchondral abnormalities in the adult knee: SONK redefined. Skelet Radiol 33(10):575–581
Rangger C, Kathrein A, Freund MC, Klestil T, Kreczy A (1998) Bone bruise of the knee: histology and cryosections in 5 cases. Acta Orthop Scand 69(3):291–294
Robertson DD, Armfield DR, Towers JD, Irrgang JJ, Maloney WJ, Harner CD (2009) Meniscal root injury and spontaneous osteonecrosis of the knee: an observation. J Bone Joint Surg Br 91(2):190–195
Roemer FW, Frobell R, Hunter DJ, Crema MD, Fischer W, Bohndorf K, Guermazi A (2009) MRI-detected subchondral bone marrow signal alterations of the knee joint: terminology, imaging appearance, relevance and radiological differential diagnosis. Osteoarthr Cartil 17(9):1115–1131
Sanders TG, Paruchuri NB, Zlatkin MB (2006) MRI of osteochondral defects of the lateral femoral condyle: incidence and pattern of injury after transient lateral dislocation of the patella. Am J Roentgenol (AJR) 187(5):1332–1337
Scher C, Craig J, Nelson F (2008) Bone marrow edema in the knee in osteoarthrosis and association with total knee arthroplasty within a three-year follow-up. Skelet Radiol 37(7):609–617
Schweitzer ME, White LM (1996) Does altered biomechanics cause marrow edema? Radiology 198(3):851–853
Sharkey PF, Cohen SB, Leinberry CF, Parvizi J (2012) Subchondral bone marrow lesions associated with knee osteoarthritis. Am J Orthop 41(9):413–417
Sheah K, Png MA (2005) Meniscal cyst causing periarticular tibial erosion. Singap Med J 46(3):137–139
Sonin AH, Fitzgerald SW, Hoff FL, Friedman H, Bresler ME (1995) MR imaging of the posterior cruciate ligament: normal, abnormal, and associated injury patterns. Radiographics 15(3):551–561
Takahashi T, Tins B, McCall IW, Richardson JB, Takagi K, Ashton K (2006) MR appearance of autologous chondrocyte implantation in the knee: correlation with the knee features and clinical outcome. Skelet Radiol 35(1):16–26
Takeda M, Higuchi H, Kimura M, Kobayashi Y, Terauchi M, Takagishi K (2008) Spontaneous osteonecrosis of the knee: histopathological differences between early and progressive cases. J Bone Joint Surg Br 90(3):324–329
Tanamas SK, Wluka AE, Pelletier JP, Pelletier JM, Abram F, Berry PA, Wang Y, Jones G, Cicuttini FM (2010) Bone marrow lesions in people with knee osteoarthritis predict progression of disease and joint replacement: a longitudinal study. Rheumatology 49(12):2413–2419
Tetta C, Busacca M, Moio A, Rinaldi R, Delcogliano M, Kon E, Filardo G, Marcacci M, Albisinni U (2010) Knee osteochondral autologous transplantation: long-term MR findings and clinical correlations. Eur J Radiol 76(1):117–123
Tins BJ, McCall IW, Takahashi T, Cassar-Pullicino V, Roberts S, Ashton B, Richardson J (2005) Autologous chondrocyte implantation in knee joint: MR imaging and histologic features at 1-year follow-up. Radiology 234(2):501–508
Trevisan C, Ortolani S, Monteleone M, Marinoni EC (2002) Regional migratory osteoporosis: a pathogenetic hypothesis based on three cases and a review of the literature. Clin Rheumatol 21(5):418–425
Vande Berg BC, Malghem J, Lecouvet FE, Maldague B (1998) Magnetic resonance imaging of the normal bone marrow. Skelet Radiol 27(9):471–483
Varenna M, Adami S, Rossini M, Gatti D, Idolazzi L, Zucchi F, Malavolta N, Sinigaglia L (2013) Treatment of complex regional pain syndrome type I with neridronate: a randomized, double-blind, placebo-controlled study. Rheumatology 52(3):534–542
Varenna M, Zucchi F, Failoni S, Becciolini A, Berruto M (2015) Intravenous neridronate in the treatment of acute painful knee osteoarthritis: a randomized controlled study. Rheumatology 54(10):1826–1832
Vasiliadis HS, Danielson B, Ljungberg M, McKeon B, Lindahl A, Peterson L (2010) Autologous chondrocyte implantation in cartilage lesions of the knee: long-term evaluation with magnetic resonance imaging and delayed gadolinium-enhanced magnetic resonance imaging technique. Am J Sports Med 38(5):943–949
Vellet AD, Marks PH, Fowler PJ, Munro TG (1991) Occult posttraumatic osteochondral lesions of the knee: prevalence, classification, and short-term sequelae evaluated with MR imaging. Radiology 178(1):271–276
Yamamoto T, Bullough PG (2000) Spontaneous osteonecrosis of the knee: the result of subchondral insufficiency fracture. J Bone Joint Surg Am 82(6):858–866
Yates PJ, Calder JD, Stranks GJ, Conn KS, Peppercorn D, Thomas NP (2007) Early MRI diagnosis and non-surgical management of spontaneous osteonecrosis of the knee. Knee 14(2):112–116
Yusuf E, Kortekaas MC, Watt I, Huizinga TW, Kloppenburg M (2011) Do knee abnormalities visualised on MRI explain knee pain in knee osteoarthritis? A systematic review. Ann Rheum Dis 70(1):60–67
Zanetti M, Bruder E, Romero J, Hodler J (2000) Bone marrow edema pattern in osteoarthritic knees: correlation between MR imaging and histologic findings. Radiology 215(3):835–840
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kon, E., Ronga, M., Filardo, G. et al. Bone marrow lesions and subchondral bone pathology of the knee. Knee Surg Sports Traumatol Arthrosc 24, 1797–1814 (2016). https://doi.org/10.1007/s00167-016-4113-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4113-2