Abstract
We present a case of herpes simplex encephalitis in an 8-year-old girl, in whom hyperintensity was detected on diffusion-weighted imaging (DWI) while conventional MRI sequences were normal 1 week after the onset of neurological symptoms. This case is rare in that a child beyond the neonatal period with focal herpes simplex encephalitis had an abnormal DWI sequence as the only MRI finding.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Herpes simplex encephalitis (HSE) is the most common cause of sporadic fatal encephalitis in the United States, accounting for 10–20% of encephalitic viral infections [1]. The timely suspicion and diagnosis of this entity is very important, as treatment with acyclovir reduces mortality at 18 months from 70% to 30% [2]. The diagnosis of HSE relies on clinical suspicion, neuroradiology and electroencephalography, and is confirmed by the detection of viral particles in the cerebrospinal fluid (CSF) by viral culture or by polymerase chain reaction (PCR) testing [2].
MRI is considered the most sensitive imaging technique [2] and reveals increased signal on T2-weighted (T2-W) sequences in HSE because of the edema associated with the necrotizing meningoencephalitis. Diffusion-weighted (DW) imaging is a relatively new MRI modality that relies on the direction-restricted diffusion of water. Freely diffusing fluids (e.g., CSF) have a high diffusion coefficient and reduced image intensity on DWI. Regions where water diffusion is restricted will have a low diffusion coefficient and will appear hyperintense compared to normal tissue. Recently, there has been an emergent interest in the diagnostic role of DWI in various infectious and ischemic brain diseases [3, 4]. We report a case of HSE in an 8-year-old girl in whom the disease process was detected radiographically only by DWI techniques, with no detectable changes on conventional T1-weighted (T1-W), T2-W, or fluid attenuated inversion recovery (FLAIR) imaging sequences.
Case report
An 8-year-old girl was transferred to our facility with a 3-day history of right-side weakness. She was hospitalized 3 days prior to transfer with a 4-day history of fever, vomiting, and personality changes consisting of decreased interactivity and decreased speaking. At the outlying facility, she was noted to have decreased movement of her right upper and lower extremities. A 2-minute tonic-clonic seizure was also reported. Her previous medical history was pertinent for developmental delay and recurrent drop attacks refractory to many treatment modalities.
Vital signs at admission revealed a temperature of 100.1°F, heart rate of 71 beats per min, respiratory rate of 18 breaths per min, and blood pressure of 111/59 mmHg. She was lethargic. She was not moving her right upper and lower extremities and had slightly decreased tone on the right side, with symmetrically preserved deep tendon reflexes.
Initial laboratory studies revealed a white blood cell count of 8.4 × 103/µl (59% neutrophils, 28.9% lymphocytes, 10.2% monocytes, and 0.5% basophils), a hemoglobin of 12.8 g/dl, and a platelet count of 243 × 103/µl. CSF studies revealed 1 lymphocyte, 1 red blood cell, glucose of 81 mg/dl, and protein of 21 mg/dl. CT scan revealed no abnormalities.
The MRI protocol (Signa Excite HD 1.5; GE Medical Systems, Milwaukee, Wis.) consisted of standard sequences (T1-W fast spin echo with TR 600 ms, full TE, 320 × 224 matrix; T2-W FRFSE TRF with TR 5,000 ms, TE 129.5 ms, 320 × 224 matrix; T2 FLAIR with TR 8,000 ms, TE 136.5 ms, TI 2,000 ms, 288 × 288 matrix; all with identical FOVs of 22 × 22 cm, and 22 slices, 5-mm thick each; echo planar imaging for DWI, 128 × 128 matrix, 20 slices, 5-mm thick, TE 77 ms; T1-W images after administration of gadolinium). The isotropic trace of ADC (apparent diffusion coefficient) was calculated from the mean of the logarithm plot of the signal as a function of the b-factor.
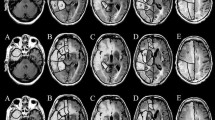
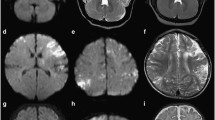
DW images revealed hyperintensity in the left parietooccipital area (Fig. 1); T1-W, T2-W (Fig. 2), and FLAIR (Fig. 3) images were normal. T1-W images after gadolinium administration were also normal (Fig. 4). On the first day of admission, she was febrile to 101.7°F and had a 10-s generalized tonic-clonic seizure. She was loaded with phosphenytoin. Electroencephalography (EEG) revealed bilateral diffuse slowing, more pronounced over the left hemisphere. PCR testing on the CSF was positive for herpes simplex virus (HSV) type I. The patient had no seizure recurrence and gradually improved. By the 4th day of hospitalization, she was talking; by the end of a 21-day course of high-dose intravenous acyclovir she was walking with assistance.
Discussion
In this case the diagnosis of an infectious encephalitis was suggested by clinical presentation (hemiparesis, fever, personality changes) and abnormalities on DW imaging and was confirmed by PCR. Interestingly, conventional MRI sequences failed to detect the disease process. A study in 1999 suggested that DW imaging is superior to conventional MRI sequences in delineating the extent of encephalitic foci, but that study did not address the potential correlation between the duration of clinical symptoms and the time at which imaging was performed [5]. More recent studies have indicated that DW imaging is more sensitive only in the acute phase (1–7 days) [4, 6]. In two recent studies in which imaging was performed in the first 5 days after symptom onset, DW imaging was found to be superior to conventional MRI in a neonate with HSE [7], and in 11 patients with viral encephalitis, two of whom were reported to have normal conventional MRI [6]. HSE was also detected by DW imaging while conventional MRI was normal in two separately reported patients, a neonate and a 66-year-old woman in whom imaging was performed within 5 days of symptom onset [4, 8]. Our patient is the fifth case of viral encephalitis with imaging abnormalities detected by DW imaging but not by conventional MRI, and the first such case to be reported in a child beyond the neonatal period.
In conclusion, this case, along with the previously reported cases of viral encephalitis with DW imaging focal findings and normal conventional MRI, suggests that DW imaging is not only superior to conventional MRI in the acute phase of lesional viral encephalitis but, more important, might be the only imaging finding and one of the earliest clues to complement clinical suspicion for, or alert the clinician to, the diagnosis of HSE. This will help in making an early diagnosis of this treatable disease with potentially devastating sequelae. DW imaging sequences should be routinely added to conventional MRI sequences when investigating central nervous system infections and potentially added to all central nervous system protocols, as it might reveal valuable unanticipated information without considerably increasing the time or cost of MRI.
References
Corey L, Spear PG (1986) Infections with herpes simplex viruses (2). N Engl J Med 20:749–757
Whitley RJ, Kimberlin DW (2005) Herpes simplex encephalitis: children and adolescents. Semin Pediatr Infect Dis 16:17–23
Gadian DG, Calamante F, Kirkham FJ et al (2000) Diffusion and perfusion magnetic resonance imaging in childhood stroke. J Child Neurol 15:279–283
Teixeira J, Zimmerman RA, Haselgrove JC et al (2001) Diffusion imaging in pediatric central nervous system infections. Neuroradiology 43:1031–1039
Tsuchiya K, Katase S, Yoshino A et al (1999) Diffusion-weighted MR imaging of encephalitis. AJR 173:1097–1099
Kiroglu Y, Calli C, Yunten N et al (2006) Diffusion-weighted MR imaging of viral encephalitis. Neuroradiology 48:875–880
Dhawan A, Kecskes Z, Jyoti R et al (2006) Early diffusion-weighted magnetic resonance imaging findings in neonatal herpes encephalitis. J Paediatr Child Health 42:824–826
Nouranifar RK, Ali M, Nath J (2003) The earliest manifestation of focal encephalitis on diffusion-weighted MRI. Clin Imaging 27:316–320
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Obeid, M., Franklin, J., Shrestha, S. et al. Diffusion-weighted imaging findings on MRI as the sole radiographic findings in a child with proven herpes simplex encephalitis. Pediatr Radiol 37, 1159–1162 (2007). https://doi.org/10.1007/s00247-007-0577-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-007-0577-z