Abstract
Background
Transthoracic ECHO is the locally accepted method for coronary surveillance of patients with Kawasaki disease but it may have limited visualization in the older child.
Objective
To assess the feasibility of multidetector CT (MDCT) angiography in the follow-up of coronary artery aneurysms in children with previous Kawasaki disease.
Materials and methods
Six children (5 boys, 1 girl; mean age 11.5 years) with known Kawasaki disease and coronary artery involvement underwent CT coronary angiography using 16-detector MDCT. The visualized lengths and diameter of all coronary segments were measured. The number, size and location of coronary artery aneurysms were recorded and compared with recent ECHO.
Results
Twelve coronary artery aneurysms (seven saccular, five fusiform) were identified by MDCT angiography. One saccular aneurysm at the junction of the distal right coronary artery and posterior descending artery was not detected by ECHO while the remaining six in proximal segments were detected by both modalities. Two of five fusiform aneurysms were not detected by ECHO due to their small sizes. Excellent agreement was found between CT and ECHO for maximal diameter and length of the visualized aneurysms.
Conclusions
MDCT angiography accurately defines coronary artery aneurysms. It is more sensitive for detecting aneurysms at distal coronary segments and fusiform aneurysms of small size.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Kawasaki disease is an acute self-limiting vasculitis of unknown aetiology that predominantly occurs in infants and young children. Over 85% of patients worldwide have disease onset before the age of 5 years [1–5].
Cardiovascular manifestations, more specifically coronary artery involvement, are the major sequelae of Kawasaki disease. Coronary artery aneurysm or ectasia develops in about 15–25% of patients [2, 3, 6] and may lead to ischaemic heart disease [7], which is the major cause of mortality [8]. Long-term follow-up of children with coronary artery disease is necessary for risk stratification and therapeutic management [9]. Transthoracic two-dimensional (2D) ECHO is often sufficient for this purpose initially. Visualization of the coronary arteries becomes progressively more difficult as children get older. Conventional angiography carries risks associated with its invasive nature and exposure to ionizing radiation; hence it is not generally accepted as a routine follow-up tool in children.
Multidetector CT (MDCT) angiography has recently been shown to be a promising non-invasive imaging method for demonstration of anatomy and evaluation of the coronary artery lumen with good image quality and high diagnostic accuracy.
The primary objective of this study was to assess the feasibility of MDCT angiography in children. We hypothesized that MDCT angiography can provide adequate quantitative (reasonable visualized length) and qualitative assessment of coronary vasculature in children and hence can serve as a non-invasive alternative for coronary surveillance of paediatric patients with Kawasaki disease. The lengths of coronary arteries visualized were assessed. Detection of coronary artery aneurysm and other significant findings such as coronary artery stenosis were recorded and compared with the findings on 2D ECHO.
Materials and methods
Patients
Six Chinese children (five boys and one girl; aged 7–15 years, mean 11 years) with Kawasaki disease diagnosed 1–13 years previously (mean 9 years) were included in the study. All patients had coronary artery aneurysm or ectasia detected by an initial baseline transthoracic 2D ECHO performed during the acute phase of the disease (at the age of 2–8 years). They had follow-up observation in a tertiary paediatric unit with regular follow-up ECHO. All patients were asymptomatic. None had undergone selective coronary angiography due to parental refusal in view of the invasive nature of the investigation. The most recent ECHO evaluation, performed by experienced paediatric cardiologists within 3 months of the CT examination, was compared with the findings of contrast-enhanced MDCT angiography. In our centre, patients with Kawasaki disease who have developed coronary artery aneurysms or ectasia are followed up more closely in the first year after diagnosis. After the acute phase of illness, they are followed up every 3–6 months for the first year, depending on the severity of the coronary artery aneurysms, with serial ECHO performed accordingly to monitor their progress. Beyond the first year, they are followed up with ECHO every 6 months and thereafter annually until they reach adulthood (18 years old in our centre) when they are referred to an adult cardiologist. Written informed consent for MDCT angiography was obtained from the parents of all patients. The protocol was approved by the Committee on Clinical Investigation in our centre.
MDCT angiography
Contrast-enhanced CT was performed using a 16-detector CT scanner (LightSpeed 16, GE Medical Systems, Milwaukee, Wis.). One hour prior to scanning, oral beta-blocker (60–100 mg propanolol) was given to each patient in order to achieve a heart rate of 70 beats per min or less. The heart rate and blood pressure of each patient were continuously monitored in the CT waiting room.
Intravascular contrast medium was administered via a 20-gauge needle into the antecubital vein. The delay time was determined by the administration of a test bolus of 10 ml iopromide (Ultravist 300; Schering, Berlin, Germany) at a flow rate of 3 ml/s (total volume 60–120 ml depending on weight of child) and the dynamic scanning of the ascending aorta at the level of the main pulmonary artery. Retrospective ECG-gated CT was performed (16×0.625-mm collimation, pitch 3.0–3.2 depending on heart rate, 0.5-s rotation time, 120 kV, and 370 mA). The mean scanning time was 20 s (range 15–25 s). Contrast-enhanced CT angiograms were reconstructed from data from 10% of every R–R interval.
Image analysis
ECHO and CT images were analyzed independently. CT data were transferred to a workstation (Advantage Workstation 4.0; GE Medical Systems, Milwaukee, Wis.). Volume rendering and multiplanar reconstruction of the coronary arteries were applied for qualitative analysis. Vessel analysis was performed for quantitative measurement. The analysis included 13 arterial segments. Segments 1–4 corresponded to the proximal, middle and distal right coronary (RCA), and posterior descending arteries; segment 5 corresponded to the left main artery (LMCA); segments 6–9 to the proximal, middle and distal left anterior descending (LAD), and first diagonal artery; and segments 11–13 and 15, to the proximal, middle and distal left circumflex (LCX), and first obtuse marginal arteries, as defined by the American Heart Association [10].
Two radiologists independently assessed the images. The radiologists were informed of the diagnosis of Kawasaki disease, but were blinded to both the baseline and follow-up ECHO findings. The two radiologists measured the maximum visualized lengths of the RCA, LMC, LAD and LCX, their major branches (posterior descending artery, first diagonal artery and left first obtuse marginal branch) and the diameter of each segment. Each arterial segment was recorded as normal, abnormal or not assessable. Coronary artery aneurysm was the main abnormality to look for in this cohort. Aneurysms were classified as saccular if axial or longitudinal diameters were nearly equal. They were classified as fusiform if there was concentric dilatation with gradual proximal and distal tapering. Aneurysms were also categorized as small (<5 mm internal diameter), medium (5–8 mm internal diameter), or giant (>8 mm internal diameter). When the whole segment of the coronary artery was larger than normal (internal segment measured ≥1.5 times that of an adjacent segment according to the Japanese Ministry of Health criteria [11], the segment was considered as ectatic. The number of aneurysms in each coronary arterial segment, the maximal diameter and length of the aneurysm, and the distance from the origin of the arterial segment involved were recorded. The presence or absence of intraluminal thrombi was also noted. Other important findings such as stenosis (defined as diameter narrowing ≥50%) and presence of wall calcifications were also recorded.
Each of the above measurements was taken twice by the radiologists on different occasions. The inter- and intraobserver variations were then calculated.
Positive findings on MDCT were then compared with ECHO for the number of lesions detected, location and size assessment. Reliability test (intraclass correlation) was applied to assess agreement between measurements between CT angiography and ECHO.
Results
Baseline ECHO showed a total of ten aneurysms with a short axis diameter from 3.5 mm to 12 mm and one coronary artery ectasia. During follow-up ECHO, one patient (patient F) was noted to have regression of her solitary coronary artery aneurysm in the right coronary artery. Other patients had persistent coronary artery aneurysms or ectasia, the sizes of which did not change markedly over the follow-up period.
MDCT findings
MDCT was performed without complications in all patients. MDCT coronary angiography permitted visualization of the coronary arteries and aneurysms with diagnostic image quality. Details of the visualized length of the major coronary arteries and the diameter of each segment in each patient are given in Table 1. The mean visualized lengths of coronary artery were 144±43.8 mm for RCA, 10±5.1 mm for LMCA, 124±26.0 mm for LAD, and 53±33.8 mm for LCX respectively. The CT measurements showed good interobserver and intraobserver reliability. The intraclass and interclass coefficients were 0.91 and 0.89, respectively.
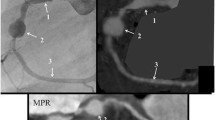
A total of 12 coronary artery aneurysms (seven saccular, five fusiform) and one arterial ectasia were found. Six of seven saccular aneurysms were present in the proximal coronary arteries and were detected by 2D ECHO. One saccular aneurysm (lesion 3 in Table 2) present at the junction of the distal RCA and posterior descending artery (PDA) was missed by ECHO. This aneurysm measured 5.8 mm in diameter and was 143 mm away from the coronary ostium (Fig. 1).
An 8-year-old boy (patient A in Table 1) with previous Kawasaki disease underwent MDCT angiography at 1-year follow-up. Curved reconstruction image shows a 5.8-mm saccular aneurysm (long arrow; aneurysm 3 in Table 2) at the junction of the distal RCA and PDA, which was not detected by ECHO. The more proximal aneurysms (arrowheads; aneurysms 1, 2, 10) were identified by both ECHO and MDCT angiography
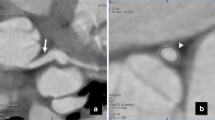
Two of five fusiform aneurysms were not detected by 2D ECHO (lesions 4 and 8 in Table 2; Fig. 2). These two aneurysms were 5 mm and 4.4 mm in diameter respectively while their longitudinal lengths were 11.5 mm and 15.1 mm. Calcifications were identified in two aneurysms without significant stenosis (Fig. 3).
An 8-year old boy (patient A in Table 1).with previous Kawasaki disease underwent MDCT angiography at 1-year follow-up. Best view of curved reconstruction image of the LAD shows an elongated fusiform aneurysm (arrow; aneurysm 4 in Table 2), which was not recognized by ECHO. A second saccular aneurysm (arrowhead, aneurysm 11 in Table 2), distal to the former lesion, was identified by both ECHO and MDCT angiography
A 13-year-old boy (patient B in Table 1) underwent MDCT angiography 9 years after the diagnosis of Kawasaki disease. Curved reconstruction image along the RCA shows calcification in the wall of the largest saccular aneurysm (arrow; aneurysm 7 in Table 2) in the proximal part of the artery. A smaller aneurysm (arrowhead; aneurysm 6 in Table 2) is present more proximally. Both aneurysms were identified by both ECHO and MDCT angiography
For all the nine aneurysms detected by both ECHO and CT angiography, their described location and size by both studies agreed closely. The intraclass correlation coefficients (with 95% confidence interval) for the maximum diameter and maximum length of the aneurysms were 0.94 (0.97–0.98) and 0.98 (0.92–0.99), respectively.
Details of the aneurysms are given in Table 2.
The LCX was ectactic in one patient; it measured 4.5 mm in diameter and had the same diameter as the LMCA. This was detected by both CT angiography and ECHO (patient D, Table 1). No definite stenotic segment was identified in any subject.
Discussion
There is evidence of persisting abnormal vascular wall morphology and vascular dysfunction in the coronary arteries despite regression of aneurysms in patients with previous Kawasaki disease [12]. New dilated or expanding lesions have been found in 3% of patients with Kawasaki disease in the late period up to 20 years after the initial diagnosis [13]. About 4% of children with Kawasaki disease eventually develop ischaemic heart disease, which is often associated with calcified stenosis [14]. Long-term follow-up into adult life is therefore needed for children with Kawasaki disease and known coronary artery involvement.
Conventional contrast angiography is the gold standard for assessing coronary arteries. There is, however, an extremely low level of acceptance by parents in our locality due to the invasiveness of the procedure and, therefore, it is not routinely performed in children in our centre. Transthoracic 2D ECHO therefore represents the standard screening method. It is non-invasive and has a high sensitivity and specificity for the detection of abnormalities of the proximal LMCA and RCA [15]. It is employed to establish a baseline for longitudinal follow-up of coronary artery morphology in young children. However, visualization of the distal coronary arteries by 2D ECHO is often limited and the visualization of coronary arteries becomes progressively more difficult as the child grows and body size increases. MDCT angiography has recently been shown to be a promising non-invasive imaging method for evaluation of coronary arteries in adults. There have been a few sporadic reports on detection of coronary aneurysms in Kawasaki disease using MDCT [16, 17]. A previous case series including three children with Kawasaki disease [18] has shown good correlation of MDCT findings with conventional angiography. One recent MDCT study with promising results has been reported in a group of adolescents and young adults with a mean age of 18.6 years [19]. MR angiography is another non-invasive alternative that has also been shown to have excellent agreement with conventional angiography findings [20]. Similar to ECHO, MR angiography has a limitation of spatial resolution in the more distal coronary arteries (diameter of which are usually less than 2 mm, as shown in our patients in Table 1). The mean visualized length of the coronary arteries by MR angiography is also much shorter than that demonstrated by MDCT. Aneurysms in the more distal coronary arteries might, therefore, not be detected by MR angiography. One would also argue that not all arterial segments were evaluated by MDCT in our study as the spatial resolution of 0.625 mm is probably not sufficient for evaluation of all distal arterial segments in children. Fortunately, previous data indicate that these segments are not usually involved [10].
In this cohort of children, MDCT was performed without complications. With the use of a beta blocker, the heart rate of all the patients could be lowered to 60–70 beats per min so that satisfactory cardiac gating could be achieved. The whole scanning procedure could be completed within 5 min.
The main limitations of this study lie with the small sample size and the lack of conventional angiography for correlation. As only patients with coronary artery aneurysm or ectasia detected by ECHO were recruited, there was also a bias in population selection. The sensitivity and accuracy of MDCT in detection of coronary artery involvement in Kawasaki disease could not be assessed. It is, however, important to realize that in a clinical setting it would be difficult and unethical to perform CT or conventional angiography on asymptomatic children when the small risk of iodinated contrast medium and irradiation are considered. In this cohort, we only targeted the feasibility of MDCT angiography in children with Kawasaki disease and we investigated any additional benefit of MDCT over ECHO in evaluation of the coronary arteries in these patients. We therefore referred to the most recent 2D ECHO to correlate with the MDCT angiography findings. Both CT angiography and ECHO were able to depict all saccular aneurysms in the proximal coronary arteries with good agreement in location and size of the aneurysms. Two mild fusiform aneurysmal dilatations not detected by ECHO were identified by MDCT angiography. This could be explained by the limitation of ECHO in visualizing the whole length of the coronary artery and thus difficulty in appreciating the gradual calibre change in fusiform type of aneurysm, in particular when the aneurysm is small. On MDCT angiography, the tortuous course of coronary arteries could be displayed as a single image using interactive 3D reformation software. In addition to better visualization of small fusiform aneurysms, an isolated saccular aneurysm in a distal coronary artery initially not detected by ECHO was identified by MDCT angiography. Despite the small cohort, MDCT angiography was more sensitive than ECHO in the detection of coronary artery aneurysms in children with Kawasaki disease.
MDCT angiography has a further advantage for the evaluation of coronary artery morphology in Kawasaki disease. It can provide additional information on potential complications related to the development of aneurysms, such as stenosis, thrombosis and atherosclerotic changes. Wall calcifications were detected in two aneurysms in this cohort, though no significant stenosis was evident in any patients. Previous adult studies have shown that MDCT can demonstrate stenosed coronary artery segments with high sensitivity and specificity [21]. Coronary calcification and plaque can also be clearly visualized [22, 23]. MDCT angiography therefore is useful in the assessment of long-term coronary sequelae and the possible development of arteriosclerotic changes in Kawasaki disease. MDCT angiography, therefore, has the potential to replace conventional angiography for serial surveillance of coronary artery abnormalities in patients with Kawasaki disease.
As breath-holding is required for performing diagnostic MDCT angiography, children should have reached a certain age so that they can follow instructions and hold their breath. In this study cohort, the youngest patient was 7 years old and could achieve breath-holding of 15 s. Children with a breath-hold shorter than 15 s are less likely to have angiography of satisfactory image quality and spatial resolution with a 16-slice CT scanner. Newer generation of MDCT such as 64- or 128-slice MDCT might allow thinner slices and significantly shortened rotation time. Coronary CT angiography of diagnostic quality might then be achieved in even younger patients.
Conclusion
MDCT angiography is feasible and accurately defines coronary artery aneurysms in children with Kawasaki disease. Diagnostic images could be obtained in children as young as 7 years in our cohort. ECHO remains the mainstay of imaging in young children with Kawasaki disease due to the lack of radiation and lack of requirement for deep sedation. MDCT angiography, however, is useful and provides a non-invasive alternative when transthoracic ECHO image quality is insufficient. The implication of radiation dose should always be considered when performing MDCT angiography. A compromise should be made between qualitative diagnostic image and dose reduction. Introduction of low mAs technique and newer generation 64-slice and 128-slice MDCT might help to minimize radiation dose to children when performing MDCT angiography.
References
Burns JC, Kushner HI, Bastian JF, et al (2000) Kawasaki disease: a brief history. Pediatrics 106:E27
Du ZD, Zhang T, Liang L, et al (2002) Epidemiologic picture of Kawasaki disease in Beijing from 1995 through 1999. Pediatr Infect Dis J 21:103–107
Park YW, Han JW, Park IS, et al (2005) Epidemiologic picture of Kawasaki disease in Korea, 2000–2002. Pediatr Int 47:382–387
Chang RK (2002) Hospitalizations for Kawasaki disease among children in the United States, 1988–1997. Pediatr Infect Dis J 21:1150–1155
Lue HC, Philip S, Chen MR, et al (2004) Surveillance of Kawasaki disease in Taiwan and review of the literature. Acta Paediatr Taiwan 45:8–14
Yanagawa H, Nakamura Y, Ysahiro M, (2001) Incidence survey of Kawasaki disease in 1997 and 1998 in Japan. Pediatrics 107:E33
Hirohisa K, Tetsu S, Teiji A, et al (1996) Heart and vascular Disease in the young: long-term consequences of Kawasaki disease: a 10- to 21-year follow-up study of 594 patients. Circulation 94:1379–1385
Nakamura Y, Yanagawa H, Harada K, et al (2000) Mortality among persons with a history of Kawasaki disease in Japan: existence of cardiac sequelae elevated the mortality. J Epidemiol 10:372–375
Nakamura Y, Aso E, Yashiro M, et al (2005) Mortality among persons with a history of Kawasaki disease in Japan: can paediatricians safely discontinue follow-up of children with a history of the disease but without cardiac sequelae? Acta Paediatr 94:429–434
Newburger JW, Takahashi M, Gerber MA, et al (2004) Diagnosis, treatment and long-term management of Kawasaki disease: a statement for health professionals form the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Pediatrics 114:1708–1733
Ministry of Health and Welfare (1984) Report of the Subcommittee on Standardization of Diagnostic Criteria and Reporting of Coronary Artery Lesions in Kawasaki Disease. Research Committee on Kawasaki disease, Ministry of Health and Welfare, Tokyo, Japan
Iemura M, Ishii M, Sugimura T, et al (2000) Long term consequences of regressed coronary aneurysms after Kawasaki disease: vascular wall morphology and function. Heart 83:307–311
Tsuda E, Kamiya T, Ono Y, et al (2005) Dilated coronary arterial lesions in the late period after Kawasaki disease. Heart 91:177–182
Sugimura T, Yokoi H, Sato N, et al (1997) Interventional treatment for children with severe coronary artery stenosis with calcification after long-term Kawasaki disease. Circulation 96:3928–3933
Hiraishi S, Misawa H, Takeda N, et al (2000) Transthoracic ultrasonic visualization of coronary aneurysm, stenosis and occlusion in Kawasaki disease. Heart 83:400–405
Wu MT, Hsieh KS, Lin CC, et al (2004) Images in cardiovascular medicine. Evaluation of coronary artery aneurysms in Kawasaki disease by multislice computed tomographic coronary angiography. Circulation 110:e339
Goo HW, Park IS, Ko JK, et al (2006) Coronary CT angiography and MR angiography in Kawasaki disease. Pediatr Radiol 36:697–705
Sohn S, Kim HS, Lee SW (2004) Multidetector row computed tomography for follow up of patients with coronary artery aneurysms due to Kawasaki disease. Pediatr Cardiol 25:35–39
Kanamaru H, Sato Y, Takayama T, et al (2005) Assessment of coronary artery abnormalities by multislice spiral computed tomography in adolescents and young adults with Kawasaki disease. Am J Cardiol 95:522–525
Greil GF, Stuber M, Botnar RM, et al (2002) Coronary magnetic resonance angiography in adolescents and young adults with Kawasaki disease. Circulation 105:908–911
Lau GT, Ridley LJ, Schieb MC, et al (2005) Coronary artery stenosis: detection with calcium scoring, CT angiography, and both methods combined. Radiology 235:415–422
Schroeder S, Kopp AF, Baumbach A, et al (2001). Noninvasive detection and evaluation of atherosclerotic coronary plaques with multislice computed tomography. J Am Coll Cardiol 37:1430–1435
Becker CR, Knez A, Ohnesorge B, et al (2000) Imaging of noncalcified coronary plaques using helical CT with retrospective ECG gating. AJR 175:423–424
Acknowledgements
We thank Mr. Tom Lee and Mr. James Cheung for their technical support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chu, W.C.W., Mok, G.C.F., Lam, W.W.M. et al. Assessment of coronary artery aneurysms in paediatric patients with Kawasaki disease by multidetector row CT angiography: feasibility and comparison with 2D echocardiography. Pediatr Radiol 36, 1148–1153 (2006). https://doi.org/10.1007/s00247-006-0281-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-006-0281-4