Abstract
Multidetector row computed tomography (MDCT) coronary angiography was performed using a 16-slice MDCT scanner in three children with coronary aneurysms due to Kawasaki disease. Patients were given a β-blocker. Following contrast injection, all data were acquired during a 20-second breathhold. Results were compared with those of conventional coronary angiography performed previously. MDCT provided clear visualization of coronary artery aneurysms, with coronary calcifications but which had not yet progressed to stenotic lesions. Because MDCT allows noninvasive detection and exclusion of coronary obstructions, it may be able to replace repeat conventional angiography as a follow-up study for children with coronary artery disease.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Coronary artery aneurysms are the most serious complication of Kawasaki disease (KD), and periodic follow-up examinations are of vital importance because these aneurysms may cause sudden death or ischemic heart disease as a result of thrombotic or stenotic occlusion of the coronary arteries. The diagnostic gold standard for identifying coronary artery lesions is selective coronary angiography. However, it is sometimes difficult to monitor progressive change from aneurysm to stenotic lesion because this technique cannot be repeated frequently due to its invasive nature and a small but significant procedure-related risk. Two-dimensional echocardiography represents the standard noninvasive modality [5]; however, visualization of the distal coronary arteries is often limited. During the past few years, considerable progress has been made in the field of noninvasive coronary imaging, including magnetic resonance imaging and electron beam computed tomography. Despite encouraging initial results, neither technique is considered suitable for routine clinical use [4]. Recently, multidetector row computed tomography (MDCT) has been developed as a modality for noninvasive visualization of coronary arteries [2] and detection of coronary artery stenoses [1, 3, 7, 9, 10, 14]. With improvements in technology, MDCT scanners with higher spatial and temporal resolution, especially through thinner slices and faster gantry rotation, have recently been introduced, leading to more improved image quality and higher diagnostic accuracy [8, 12].
We performed coronary angiography using a 16-slice MDCT scanner in three children with coronary aneurysms due to KD, and results were compared with those of conventional coronary angiography performed previously so that we could evaluate the potential value of MDCT as an alternative diagnostic modality in the follow-up of patients with coronary artery disease.
Materials and Methods
Study Population
In three children with coronary aneurysms due to KD, MDCT coronary angiography, instead of the conventional approach, was performed to follow up the morphologic change in coronary artery lesions. The study was approved by the institutional ethical committee, and informed consent was obtained from the children’s parents.
Patient 1
A 9-year-old girl underwent MDCT angiography. At the age of 4.7 years, she was transferred to our institution after 9 days of disease and diagnosed with KD, with giant aneurysms of the right coronary artery (RCA) and dilatation of the mid-left anterior descending coronary artery (LAD). Thereafter, selective coronary angiography was serially carried out to monitor coronary wall changes. On the last study performed at 7.6 years, multiple aneurysms in the proximal and middle RCA were seen (Fig. 1A), with regression of dilatation of the LAD.
(A) Coronary angiogram of a 7.6-year-old girl 2.9 years after KD showing multiple aneurysms in the RCA. (B, C) Corresponding MDCT coronary angiogram with maximum intensity projection (B) and 3D volume rendering image (C) at 9 years of age showing mural calcified plaques (arrow) in addition to clear visualization of the coronary aneurysms.
Patient 2
An 11.8-year-old boy underwent MDCT angiography. At 7.3 years of age, he presented with periungual desquamation in an afebrile state 2 weeks after the onset of KD. He had already developed giant aneurysms of both LAD and RCA. The last coronary angiography was performed at 9.3 years of age, which revealed giant aneurysms of both proximal LAD and RCA (Fig. 2A and 2B).
(A, B) Coronary angiogram of a 9.3-year-old boy 2 years after KD showing a saccular aneurysm in the proximal LAD (A) and two aneurysms in the RCA (B). (C, D) Maximum intensity projection images in coronal orientation obtained by MDCT at 11.8 years of age demonstrating an undulating change in the inferior wall of the LAD aneurysm (arrow) with a calcified nodule (C) and visualization of coronary aneurysms in the RCA (D). (E, F) 3D volume rendering images showing clear visualization of both coronary arteries and their aneurysms. Note that there are no stenotic lesions in both coronary arteries.
Patient 3
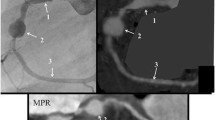
MDCT angiography was performed in a 6.4-year-old boy. At the age of 3.6 years, he was treated with a total of three courses of intravenous immunoglobulin due to prolonged fever in the acute stage of KD. Initial echocardiogram revealed a giant aneurysm of the proximal LAD, a huge fusiform aneurysm of the proximal RCA, and a small amount of pericardial effusion. He has been given salicylate, dipyridamole, and warfarin during follow-up. Giant aneurysms in both coronary arteries were shown on the latest coronary angiography performed 2.2 years ago (Fig. 3A and 3B).
(A, B) Coronary angiograms of a 4.2-year-old boy 7 months after KD showing an aneurysm in the proximal LAD (A) and a huge fusiform aneurysm in the RCA (B). (C, D) MDCT angiograms in axial orientation (C) and 3D volume rendering image (D) at 6.4 years of age demonstrating an aneurysm in the LAD (arrows) and a huge RCA aneurysm (An). Note motion artifacts of the RCA and its aneurysm.
MDCT Scan Protocol
Using a 16-slice MDCT scanner (Siemens Sensation 16), a volume data set was obtained (detector collimation, 12 × 0.75 mm; gantry rotation time, 420 msec; table feed, 2.8 mm/rotation; tube voltage, 120 kV). All patients were given 30–50 mg of oral metoprolol 1 hour before the scan. A bolus injection of 2–2.5 ml/kg of nonionic contrast medium (iohexol; Nycomed, Cork, Ireland) was given via the antecubital vein. When the signal density level in the ascending aorta reached a predefined threshold of 100 Hounsfield units, the patient was instructed to maintain an inspiratory breathhold for 20 seconds, during which the CT data and electrocardiogram (ECG) trace were obtained. Next, axial images were reconstructed with a slice thickness of 3 mm in 2-mm intervals using an ECG-gated half-scan reconstruction algorithm to obtain an image acquisition window of 210 msec. At least three data sets were created with a reconstruction window positioned within the diastolic phase starting at 300, 400, and 500 msec before the next R wave. One data set with the least motion artifacts, typically reconstructed at approximately 400 msec before the following R wave, was selected for further analysis. For three-dimensional reconstruction and visualization of the coronary arteries, the volume rendering technique and maximum intensity projection in axial and coronal orientation with the use of Syngo software (VA60B) were applied.
Results
MDCT was performed without complications in our patients. The scan time was 16–18 seconds, and the entire examination was generally completed within 10 minutes. Heart rate 1 hour before the scan was 74–90 beats per minute (bpm). The use of a ß-blocker significantly decreased heart rate during scanning (range, 56–76 bpm), with a mean reduction of 20.8% (Table 1).
Compared with conventional coronary angiography performed 1.4–2.5 years ago, MDCT coronary angiography also permitted visualization of the coronary arteries and aneurysms with good image quality (Figs. 1B, 1C, and 2C–2F). Generally, coronary aneurysms did not significantly change in size, but in one aneurysm a smooth inferior wall was altered to undulating margin (Fig. 2C). There was no progressive change of aneurysms to stenotic lesions; but coronary calcifications were clearly demonstrated by MDCT angiography (Figs. 1B and 2C). The youngest (patient 3) was unable to hold his breath sufficiently during the scan, when his heart rate was 76 bpm; the RCA and its giant aneurysm were affected by motion artifacts but without significant stenosis (Fig. 3C and 3D).
Discussion
Noninvasive coronary imaging has become available due to the development of imaging modalities such as magnetic resonance imaging, electron beam computed tomography, and recently, MDCT. Four-slice MDCT scanners allow visualization of the coronary lumen [2] and detection of stenoses [1, 3, 7, 9, 10, 14], but cardiac motion artifacts and coronary calcifications render 20–30% of the coronary segments noninterpretable [1, 3, 9, 10]. Recently, a new generation of MDCT scanners equipped with thinner slices and faster rotation have been introduced, leading to improved image quality and higher diagnostic accuracy [8, 12].
Using this latest-generation 16-slice MDCT scanner, we performed noninvasive coronary angiography to monitor the morphologic change of coronary aneurysms due to KD. Based on the findings previously obtained with conventional angiography, all coronary aneurysms were well visualized with no significant changes in size, and there was no stenotic lesion on MDCT angiography. Instead, coronary calcifications were clearly identified, which may correlate with the extent and severity of atherosclerosis in addition to the risk of future events [6]. Because we focused on noninvasively detecting the coronary wall change to stenoses from the preexisting lesions, we did not determine the sensitivity, specificity, and predictive values of MDCT for detection of coronary artery disease.
Advantages of MDCT coronary angiography are its noninvasive nature, a short duration of examination (approximately 10 min), and that there is no need for hospital admission. Unlike conventional coronary angiography, MDCT may be useful to differentiate the origin of coronary stenoses (calcification vs fatty or fibrous lesions) [14], whereas this technique is not reliable in patients with arrhythmias or rapid heart rates. Disadvantages are a considerable radiation dose and the use of contrast material. Because the patient’s heart rate critically influences image quality [3, 11, 13], it is important to lower the heart rate using a β-blocker. In addition to motion artifacts from rapid coronary artery motion, movement of the patient, such as breathing, also affects image quality. In our youngest patient, aged 6.4 years, image quality was affected by motion artifacts resulting from insufficient breathhold and/or a relatively rapid heart rate of 76 bpm during the scan compared with that of older patients (56 and 58 bpm). Thus, it is advisable to limit its clinical use in young children and to lower the heart rate to <60 bpm at the time of the MDCT scan in order to achieve better image quality.
In summary, with sufficient breathhold and heart rate control, MDCT permits visualization of the coronary arteries with high image quality and allows noninvasive detection and exclusion of coronary obstructions, avoiding the risks of repeat conventional coronary angiography. Therefore, this new noninvasive modality may possibly replace conventional angiography in the follow-up of children with known coronary artery disease.
References
S Achenbach T Giesler D Ropers et al. (2001) ArticleTitleDetection of coronary artery stenoses by contrast-enhanced, retrospectively electrocardiographically-gated, multislice spiral computed tomography. Circulation 103 2535–2538 Occurrence Handle1:STN:280:DC%2BD3M3pvFaisg%3D%3D Occurrence Handle11382719
S Achenbach S Ulzheimer U Baum et al. (2000) ArticleTitleNoninvasive coronary angiography by retrospectively ECG-gated multislice spiral CT. Circulation 102 2823–2828 Occurrence Handle1:STN:280:DC%2BD3M%2FpslSltA%3D%3D Occurrence Handle11104739
T Giesler U Baum D Ropers et al. (2002) ArticleTitleNoninvasive visualization of coronary arteries using contrast-enhanced multidetector CT: influence of heart rate on image quality and stenosis detection. Am J Roentgenol 179 911–916
GF Greil M Stuber RM Botnar et al. (2002) ArticleTitleCoronary magnetic resonance angiography in adolescents and young adults with Kawasaki disease. Circulation 105 908–911
S Hiraishi H Misawa N Takeda et al. (2000) ArticleTitleTransthoracic ultrasonic visualization of coronary aneurysm, stenosis, and occlusion in Kawasaki disease. Heart 83 400–405
WR Janowitz (2001) ArticleTitleCT imaging of coronary artery calcium as an indicator of atherosclerotic disease: an overview. J Thorac Imaging 16 2–7 Occurrence Handle10.1097/00005382-200101000-00002 Occurrence Handle1:STN:280:DC%2BD3M7ns1KktA%3D%3D Occurrence Handle11149689
A Knez CR Becker A Leber et al. (2001) ArticleTitleUsefulness of multislice spiral computed tomography angiography for determination of coronary artery stenoses. Am J Cardiol 88 1191–1194 Occurrence Handle1:STN:280:DC%2BD3MnltF2ktg%3D%3D Occurrence Handle11703970
K Nieman F Cademartiri PA Lemos et al. (2002) ArticleTitleReliable noninvasive coronary angiography with fast submillimeter multislice spiral computed tomography. Circulation 106 2051–2054
K Nieman M Oudkerk BJ Rensing et al. (2001) ArticleTitleCoronary angiography with multislice computed tomography. Lancet 357 599–603 Occurrence Handle1:STN:280:DC%2BD3MrhtV2mtw%3D%3D Occurrence Handle11558487
K Nieman BJ Rensing RJ van Geuns et al. (2002) ArticleTitleUsefulness of multislice computed tomography for detecting obstructive coronary artery disease. Am J Cardiol 89 913–918 Occurrence Handle10.1016/S0002-9149(02)02238-5 Occurrence Handle11950427
K Nieman BJ Rensing RJ van Geuns et al. (2002) ArticleTitleNon-invasive coronary angiography with multislice spiral tomography: impact of heart rate. Heart 88 470–474 Occurrence Handle10.1136/heart.88.5.470 Occurrence Handle1:STN:280:DC%2BD38nisVWntg%3D%3D Occurrence Handle12381635
D Ropers U Baum K Pohle et al. (2003) ArticleTitleDetection of coronary artery stenoses with thin-slice multidetector row spiral computed tomography and multiplanar reconstruction. Circulation 107 664–666
S Schroeder AF Kopp A Kuettner et al. (2002) ArticleTitleInfluence of heart rate on vessel visibility in noninvasive coronary angiography using new multislice computed tomography. Experience in 94 patients. Clin Imaging 26 106–111 Occurrence Handle10.1016/S0899-7071(01)00371-0 Occurrence Handle11852217
H Treede C Becker H Reichenspurner et al. (2002) ArticleTitleMultidetector computed tomography (MDCT) in coronary surgery: first experiences with a new tool for diagnosis of coronary artery disease. Ann Thorac Surg 74 S1398–S1402 Occurrence Handle10.1016/S0003-4975(02)04010-9 Occurrence Handle12400825
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sohn, S., Kim, H. & Lee, S. Multidetector Row Computed Tomography for Follow-Up of Patients with Coronary Artery Aneurysms Due to Kawasaki Disease . Pediatr Cardiol 25, 35–39 (2004). https://doi.org/10.1007/s00246-003-0559-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-003-0559-3