Abstract
Background: Traumatic brain injury is a major cause of disability and death in the pediatric population. The metabolic and neurochemical abnormalities that underlie traumatic brain injury remain poorly understood, but hypoxia-ischemic injury might play an important role. Objective: This study evaluated children with inflicted traumatic brain injury using magnetic resonance spectroscopy (MRS). We postulated that children with hypoxic-ischemic injury indicated by elevated lactate in the acute phase of injury will have worse early neurological status and short-term clinical outcomes than those without lactate upon MRS. Materials and methods: This prospective study employed proton MRS to sample bilaterally the frontal lobes and the parasagittal cortex within the parietal and occipital lobes of 11 patients with inflicted traumatic brain injury who were undergoing a clinical MRI examination. Patients’ measured clinical course while hospitalized included initial neurological evaluation, presence of seizure activity, need for admission to the pediatric intensive care unit (PICU), number of days hospitalized, presence of retinal hemorrhages and presence of bone fractures. Measurement of outcome was determined using the Pediatric Overall Performance Category Scale (POPCS; 1 = good performance; 6 = death). Results: Four children demonstrated elevated lactate and diminished N-acetyl aspartate (a neuronal marker) within several regions, indicating global ischemic injury (lactate-positive global group). These four children all had seizure activity and abnormal initial neurological examinations and required admission to the PICU. The mean POPCS for this group was 3.25. In four other children, lactate was detected within at least one region, indicating a focal ischemic injury (lactate-positive focal group); two of these children had seizure activity, and two had an abnormal initial neurological examination. The mean POPCS score was 1.5 for this group. The remaining three children had no evidence of lactate upon MRS (lactate-negative group). These children did not have seizure activity, did not require admission to the PICU, nor did they have initial abnormal neurological examinations. The mean POPCS score was 1.3 for this group. Summary: Patients with inflicted traumatic brain injury and evidence of hypoxic-ischemic injury as indicated by elevated lactate on MRS tend to have worse early neurological status and early outcome scores. Lactate levels as sampled by MRS might predict early clinical outcome in inflicted traumatic brain injury.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Traumatic brain injury (TBI) is a major cause of disability and death in the pediatric population [1]. Many young children with TBI are victims of inflicted traumatic brain injury, or shaken baby syndrome. Shaken baby syndrome is classically described in infants or young children who have subdural or subarachnoid hemorrhages, retinal hemorrhages and long bone fractures, but who have minimal or no evidence of external trauma [2]; however, many patients do not have this complete constellation of injuries.
Infants and children who are victims of inflicted traumatic brain injury have poor outcomes and have worse outcomes than infants and children with non-inflicted traumatic brain injuries [3]. Even when an infant or child who sustains an inflicted traumatic brain injury appears neurologically intact after the injury, that infant or child can be left with serious and permanent disabilities [4].
The reasons for the poor outcomes in infants and children who sustain inflicted traumatic brain injury are not known. Some authors have found that infants and children who suffer inflicted traumatic brain injury have shown evidence of ischemia and hypoxia, as measured by blood pressure, metabolic acidosis [5] and cerebral perfusion pressure [6]. These authors postulate that early brain hypoxia-ischemia is an important cause of the poor outcomes in this group [5, 6]. Lactate results from impaired aerobic glycolysis and is associated with ischemic and hypoxic injuries. Being able to measure lactate levels in the brain early in an injury could help to predict which patients are suffering brain hypoxic-ischemic injuries and which ones, therefore, are likely to have poor outcomes.
Proton magnetic resonance spectroscopy (MRS) can be used in conjunction with MRI to help reveal and understand destructive processes in the brain. MRS demonstrates select metabolites within the brain. The concentration levels of metabolites reflect the degree of cellular integrity and/or injury [7]. Elevated lactate levels are recognized with proton MRS and can be used to evaluate for evidence of early hypoxic-ischemic injury [8]. Evidence of hypoxia-ischemia in the subacute setting can be implicated with a reduction of the neuronal/axonal marker N-acetyl-aspartate (NAA) [7].
We postulated that spectroscopic evidence of ischemic injury would correlate with the acute clinical course and short-term outcome of patients with inflicted traumatic brain injury.
Materials and methods
This prospective study was approved by the Institutional Review Board at our institution. Infants and children who were diagnosed by the child-abuse team (CAT) with inflicted traumatic brain injury were studied. Determination of inflicted traumatic brain injury was based on findings from the clinical history, physical examination findings, and radiographic findings. Neuroradiological evaluations consisted of initial head CT and MRI. Patients with a history of an underlying neurological or metabolic disorder, known history of developmental delay, or prior central nervous system injury were excluded from the study.
Patients received MRI and MRS as soon as they were clinically stable, and the time interval from admission to MRS was recorded. Recorded clinical information included age at the time of injury, findings from the initial neurological examination, presence of seizures initially or at any time during the hospitalization (based on history and/or EEG findings), presence of retinal hemorrhages, presence of fractures, the number of days hospitalized, and need for admission to the pediatric intensive care unit (PICU).
The neurological outcomes at discharge were classified by one of the authors using the Pediatric Overall Performance Category Scale (POPCS), a six-point outcome scoring system modified from the Glasgow Outcome Scale. The POPCS has been found to be reliable and valid for the measurement of short-term outcomes in children who have suffered a critical illness or injury [9]. The score includes the following outcomes: (1) good overall performance: capable of normal activities of daily life; (2) mild overall disability: minor physical or neurological problem that is still compatible with normal life; (3) moderate overall disability: conscious and performs independent activities of daily life but is disabled for competitive performance in school; (4) severe overall disability: conscious but dependent on others for activities of daily living support; (5) coma or vegetative state; (6) brain death [9].
Structural MRI and proton MRS procedure
All MRI and MRS investigations were acquired on a 1.5-T Signa General Electric MR scanner (Milwaukee, Wis., USA). For each subject, a sagittal spin echo series was acquired (echo time (TE) 14 ms, repetition time (TR) 500 ms, field of view (FOV) 22 cm, 5-mm thick slices with 1-mm spacing). An axial proton density and T2-weighted sequence (TE 30 and 110 ms, TR 2,500 ms, FOV 20 cm, 4.0 mm thick with 1.5-mm interslice spacing) was acquired. An axial inversion recovery sequence (TE 20 ms, TR 2,000 ms, inversion time (TI) 800 ms, FOV 20 cm, 4.0 mm thick with 1.5-mm interslice spacing) was acquired. An axial gradient echo sequence (TE 30 ms, TR 600 ms, flip angle 20°, FOV 20 cm, 5.0 mm thick with 2-mm interslice spacing) was acquired. A coronal fast-spin echo (FSE) sequence (TE 120 ms, TR 5,000 ms, echo train length (ETL) 12, FOV 20 cm, 4.0 mm thick with 1.5-mm interslice spacing) was acquired. Single voxel spectra were prescribed from the axial T2-weighted imaging series based on anatomical landmarks. Three single voxels, approximately 8 cc in volume, were positioned in the left frontal, right frontal, and occipital cortex. The voxels were positioned by a single spectroscopist to ensure consistent placement. All spectra were acquired using point-resolved spectroscopy (PRESS) (TE 35 ms, TR 2,000 ms with 64 averages). If time permitted, long-echo (TE 288 ms, TR 2,000 ms with 128 averages) images were obtained (6 of 11 patients) to reveal lactate signal further.
A board-certified pediatric neuroradiologist reviewed the CT and conventional MR imaging for features consistent with inflicted TBI. These features included acute subarachnoid hemorrhage (SAH) and subdural hemorrhage (SDH), subdural collections, and focal and diffuse evidence of hypoxia-ischemia.
MRS data were processed using the proton brain examination single voxel (PROBE/SV) quantification tool (General Electric Healthcare, Milwaukee, Wis., USA) [10]. Five spectral areas associated with NAA, creatine and phosphocreatine (Cr), choline (Cho), myo-inositol (mI), and brain water were quantitated by the Marquardt–Levenberg curve-fitting algorithm [11]. Prior to curve fitting, line widths were normalized, and a Lorentzian-to-Gaussian transformation was performed. Metabolite ratios were calculated from these areas. Lactate signal was denoted as present or absent by visual inspection of the spectra by the spectroscopist. Control data (total n = 25) for assessment of NAA/Cr levels was obtained in age-matched and region-matched spectra sampled from clinically indicated MRS examinations, which were without neuroimaging findings. Mean control NAA/Cr values with respect to age are 1.4 at 4–6 weeks, 1.5 at 11–16 weeks and 1.6 at 26 weeks. Unfortunately, we do not have truly normative control data, as uninjured infants are not imaged. However, data extrapolated from older children and those of infants imaged for minor clinical findings offer us usable control data in the form of metabolite ratios.
Statistical analysis
The Fisher’s exact test was used to compare the spectral data and clinical data in patients. Differences were considered significant at a P < 0.05 level. Patients were grouped based on the presence of lactate on spectroscopy. Lactate appears as a doublet resonance located at 1.3 ppm on proton MRS. The signal must be twice as intense as the baseline noise for detection. Short-echo MRS displays lactate in combination with lipids. Long-echo MRS displays lactate without the presence of lipids.
Results
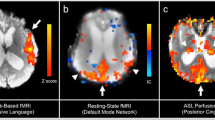
Between March 2001 and August 2002, 11 patients who were diagnosed with inflicted traumatic brain injury and who underwent MRI and spectroscopy were included in the study. The patients had a mean age at imaging of 10.4 weeks (range 4–26 weeks). Six patients were male. The patients were divided into three groups based on the presence of a lactate peak on MRS (Table 1). There were four patients in the lactate-positive global group; these patients had a lactate peak detected in at least two voxels. There were four patients in the lactate-positive focal group. These patients had a lactate peak detected in one voxel only. There were three patients in the lactate-negative group. These patients did not have lactate detected in any of the sampled voxels. Figure 1 shows MRI and MRS findings in a lactate-positive global patient. Figure 2 shows findings in a lactate-positive focal patient. Figure 3 shows findings in a lactate-negative patient.
The MR findings in a 16-week-old boy (patient 1). a Sagittal T1-weighted, b coronal T2-weighted, c, e axial MPGR, and d axial T2-weighted images. The MPGR sequence demonstrates subarachnoid and subdural hemorrhage at the convexity on the left side and along the posterior falx. On T2-weighted images, within bilateral parietal and frontal lobes, a loss of gray- and white-matter differentiation consistent with diffuse ischemic injury is demonstrated. Cerebellar signal abnormalities are noted on both T1-weighed and T2-weighed images. Short-echo (f) and long-echo (g) (TR, TE: 2,000/35, 288 ms) proton MR spectroscopy performed on a voxel positioned within left frontal lobe indicates reduced NAA and elevated lactate
The MR findings in a 12-week-old boy (patient 4). a Sagittal T1-weighted, b coronal T2-weighted, c axial IR, d axial MPGR, and e axial T2-weighted images. The images demonstrate bilateral subdural fluid collections with components of left subdural hemorrhage. f Short-echo proton MR spectroscopy performed on a voxel positioned within the left frontal lobe indicates reduced NAA and elevated lactate
The MR Findings in a 26-week-old boy (patient 8). a Sagittal T1-weighted, b coronal T2-weighted, c axial IR, d axial MPGR, and e axial T2-weighted images. The images demonstrate bilateral subdural fluid collections. f A short-echo proton MR spectroscopy performed on a voxel positioned within the occipital cortex is normal
Patients also had values of NAA quantified (expressed as ratio of NAA/Cr). These values are shown in Table 1 with individual comparisons based on age and region to values extracted from metabolite ratio level curves generated clinically. In the lactate-positive global group, a normal NAA/Cr level was found in only one voxel. For that patient, the two other voxels sampled demonstrated reduced NAA/Cr levels (Table 1). In the lactate-positive focal group of 10 sampled voxels, only four demonstrated age- and region-matched normal NAA/Cr levels. In the lactate-negative group of eight sampled voxels, five revealed normal NAA/Cr levels.
Table 2 summarizes the outcomes at discharge for patients grouped by the presence of lactate. The outcomes are stratified using the POPCS Outcome Scale. None of the patients in our series died or was left in a vegetative state, so the outcomes listed include good overall performance and mild, moderate or severe overall disability. The patients in the lactate-positive global group had either moderate or severe disabilities upon hospital discharge. Conversely, almost all of the patients (6/7) in the lactate-positive focal and lactate-negative groups had a good outcome or only mild deficits upon hospital discharge. The mean POPCS score for patients in the lactate-positive global group was 3.25. The mean POPCS score for patients in the lactate-positive focal group was 1.5; in the lactate-negative group, it was 1.3.
Table 3 compares the clinical presentation of patients grouped by the presence of lactate. All of the patients in the lactate-positive global group had an initial abnormal neurological examination, retinal hemorrhages and seizures and were admitted to the PICU. Three patients in this group had fractures. These fractures included bilateral clavicle fractures and a fracture of the first rib in one patient, a sixth rib fracture in one patient and a parietal skull fracture in one patient. Four patients in the lactate-positive focal and lactate-negative groups had fractures including rib fractures (two patients) and tibia metaphyseal fractures (two patients). The presence of retinal hemorrhages or fractures was not necessary to make the diagnosis of inflicted traumatic brain injury in our patients.
Most of the patients demonstrated acute, high-attenuation subdural (10/11) and subarachnoid hemorrhages (9/11) on CT (Table 4). The lactate-positive global group demonstrated diffuse (3/4) and multifocal (1/4) regions consistent with hypoxia-ischemia evident on both CT and conventional MRI sequences. The lactate-positive focal and lactate-negative groups had no regions of hypoxia-ischemia noted by conventional imaging. The brain parenchyma in both the lactate-positive focal and lactate-negative groups had no acute signal and attenuation abnormalities.
The time interval range from admission to performing MRI and MRS for the patients in the lactate-positive global group was 1-19 days (mean 6.5 days; 2.3 days excluding the outlier of 19 days). The time interval range from admission to performing MRS for the patients in the lactate-positive focal group was 2–4 days (mean 3 days), and in the lactate-negative group it was 3–9 days (mean 5 days).
Discussion
The presence of lactate on MRS might predict early clinical outcome in patients with inflicted traumatic brain injury. Patients who have suffered inflicted traumatic brain injury and have lactate detected on initial MRS are more likely to have an abnormal initial neurological examination, need intensive care and have a poor short-term outcome score compared to patients in whom lactate is not observed.
Other investigators have examined the role of MRS for predicting the outcomes of infants and children with brain injury. Haseler et al. [12] studied three infants with shaken baby syndrome and measured the principal metabolite concentrations observable by MRS and also measured the infants’ clinical outcomes at 6–10 months after injury. The infant who appeared to have a full neurological recovery 6 months after the insult had normal metabolite levels both initially (7 days after the trauma) and later (19 days after). The two infants with greatly reduced and absent levels of NAA initially had poor clinical outcomes at 10 and 6 months after trauma, respectively [12].
Holshouser et al. [13] demonstrated that the presence of lactate on proton MR spectroscopy in neonates, infants and children with central nervous system injury correlated with poorer outcome from the injury. Ashwal et al. [14] studied a group of infants and children with traumatic brain injury using MRS and also measured their clinical outcomes. Lactate was present in the great majority of infants and children (91% and 80%, respectively) with a poor outcome. None of the patients with a good outcome had lactate evidence on MRS. Finally, Kadri et al. [15] showed that the presence of lactate on MRS had a good predictive value on outcome in neonates with hypoxic-ischemic encephalopathy.
Relying on the detection of lactate alone to evaluate for hypoxic-ischemic injury is problematic. Lactate is elevated within the early stages of brain injury; lactate levels can rise immediately after injury and then fall after approximately 4 days. The MRS evaluation at a subacute stage of hypoxic-ischemic injury might miss the optimal time for observing a lactate elevation. However, NAA declines during this period correspond with neural dysfunction. This trend was noted in patient NAA/Cr levels. Normal NAA/Cr levels were found in 12.5% of sampled regions for the lactate-positive global group, 40% of the lactate-positive focal group and 62.5% of the lactate-negative group.
In some of our patients, lactate was elevated even though spectroscopy was obtained more than 4 days post-injury. This likely reflects a greater degree of injury severity and ongoing anaerobic glycolysis. The short-echo technique employed for this study provides the maximum number of metabolites with the fastest scan time in the clinical setting. Metabolites observed only on short-echo MRS such as myoinositol, glutamate and glutamine fluctuate more rapidly than other metabolites. Unfortunately, because of our small sample size, we did not appreciate significant changes in these metabolites. From the results of our study, with changes found in lactate and NAA levels, it seems that employing spectroscopic methods with longer TE would be optimal for lactate and NAA detection in the acute and subacute phases of injury.
A review of the conventional imaging on our patients noted diffuse and multifocal regions consistent with hypoxic-ischemic injury in the lactate-positive global group. However, the lactate-positive focal group did not have imaging evidence of hypoxic-ischemic regions. The underestimation of injury that could occur with conventional neuroimaging is demonstrated with the clinical findings and outcome of the MRS-derived lactate-positive focal group. In this group, 2/4 demonstrated an abnormal initial neurological examination, 3/4 had retinal hemorrhages and fractures and 1/4 revealed seizures. One member of the lactate-positive focal group had an outcome of moderate disability. At the time of this study, diffusion-weighted imaging was not always included in the imaging protocol. Diffusion-weighted imaging might have complemented the conventional imaging in detecting ischemia as the spectroscopy did in this study.
We were unable to perform the spectroscopic evaluations at a uniform time from injury. The majority of our patients, 9 of the 11, were imaged fewer than 4 days after hospital admission. This time limitation is compounded by the fact that for patients with inflicted traumatic brain injury, the history offered by the caregiver is often wrong or misleading, so the stated time of injury is not always accurate. This also influences the findings if diffusion-weighted imaging is used for detecting ischemia. However, MRS can offer other markers for detecting hypoxia-ischemia throughout its evolution [7, 14]. Lactate elevation is the earliest measured marker, followed by reductions in NAA levels in the subacute phase. After lactate is cleared, persistent declines in NAA are followed by elevations of choline and reductions in creatine associated with cellular death. Although NAA reductions occur for most pathological processes in the brain, upon combining MRS with clinical history and imaging, hypoxic and ischemic injury markers can be surmised in the absence of diffusion imaging or lactate markers.
Our report details a preliminary study. The sample size of our pediatric population is small. Larger populations need to be studied with similar and expanded methods focusing on both the detection of hypoxic ischemic injury using diffusion-weighted imaging and MRS, and the role of MRS for predicting the outcomes of infants and children with traumatic brain injury. Identifying biological brain markers that predict early clinical outcomes in pediatric traumatic brain injury might help to guide clinical and rehabilitative management for these patients and identify children at high risk for a poorer outcome.
References
Lescohier I, DiScala C, Caffey J (1993) Blunt trauma in children: causes and outcomes of head versus extracranial injury. Pediatrics 91:721–725
Caffey J (1972) On the theory and practice of shaking infants: its potential residual effects of permanent brain damage and mental retardation. Am J Dis Child 124:161–169
Ewing-Cobbs L, Kramer L, Prasad M (1998) Neuroimaging, physical and developmental findings after inflicted and noninflicted traumatic brain injury in young children. Pediatrics 102:300–307
Makoroff KL, Putnam FW (2003) Outcomes in inflicted traumatic brain injury. Dev Med Child Neurol 45:497–502
Johnson DL, Boal D, Baule R (1995) Role of apnea in nonaccidental head injury. Pediatr Neurosurg 23:305–310
Barlow KM, Minns RA (1999) The relationship between intracranial pressure and outcome in non-accidental head injury. Dev Med Child Neurol 4:220–225
Cecil KM, Jones BV (2001) Magnetic resonance spectroscopy of the pediatric brain. Top Magn Reson Imag 12:435–452
Lanfermann H, Kugel H, Heindel W, et al (1995) Metabolic changes in acute and subacute cerebral infarctions: findings at proton MR spectroscopic imaging. Radiology 196:203–210
Fiser DH (1992) Assessing the outcome of pediatric intensive care. J Pediatr 121:68–74
Webb PG, Sailasuta N, Kohler SJ, et al (1994) Automated single-voxel proton MRS: technical development and multisite verification. Magn Reson Med 31:365–373
Marquardt DW (1963) An algorithm for least-squares estimation on nonlinear parameters. J Soc Ind Appl Math 11:431–441
Haseler LJ, Phil M, Arcinue E, et al (1997) Evidence from proton magnetic resonance spectroscopy for a metabolic cascade of neuronal damage in shaken baby syndrome. Pediatrics 99:4–14
Holshouser BA, Ashwal S, Luh GY, et al (1997) Proton MR spectroscopy after acute central nervous system injury: outcome prediction in neonates, infants, and children. Radiology 202:487–496
Ashwal S, Holshouser BA, Shu SK, et al (2000) Predictive value of proton magnetic resonance spectroscopy in pediatric closed-head injury. Pediatr Neurol 23:114–125
Kadri M, Shu S, Holhouser B, et al (2003) Proton magnetic resonance spectroscopy improves outcome prediction in perinatal CNS insults. J Perinatol 23:181–185
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Makoroff, K.L., Cecil, K.M., Care, M. et al. Elevated lactate as an early marker of brain injury in inflicted traumatic brain injury. Pediatr Radiol 35, 668–676 (2005). https://doi.org/10.1007/s00247-005-1441-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-005-1441-7