Abstract
The purpose of these analyses was to determine how specific comorbidities and medical interventions impact risk of inpatient mortality in those with hypoplastic left heart syndrome undergoing Norwood procedure. The secondary aims were to determine the impact of these on billed charges, postoperative length of stay, and risk of cardiac arrest. Admissions from 2004 to 2015 in the Pediatric Health Information System database with hypoplastic left heart syndrome and Norwood procedure were identified. Admission characteristics, patient interventions, and the presence of comorbidities were captured. A total of 5,138 admissions were identified meeting inclusion criteria. Of these 829 (16.1%) experienced inpatient mortality, and 352 (6.7%) experienced cardiac arrest. The frequency of inpatient mortality did not significantly change over the course of the study era. The frequency of cardiac arrest significantly decreased from 7.4% in 2004 to 4.3% in 2015 (p = 0.04). The frequency of pharmacologic therapies, particularly vasoactive use, decreased as the study period progressed. Regression analyses demonstrated a significant association between cardiac arrest and inpatient mortality with arrhythmias, acute kidney injury, and pulmonary hypertension. Similarly, regression analyses demonstrated a significant association between increase in billed charges and length of stay with year of surgery, presence of heart failure, syndromes, and acute kidney injury. For patients with hypoplastic left heart syndrome undergoing the Norwood procedure, the frequency of pharmacologic therapies and cardiac arrest has decreased over time. There are significant associations between acute kidney injury, arrythmias, and pulmonary hypertension with cardiac arrest and mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypoplastic left heart syndrome (HLHS) is a group of clinical entities characterized by hypoplasia of the left heart structures and systemic outflow tract obstruction. The term was first used by Noonan and Nadas in 1958 [1]. The Norwood procedure with a modified Blalock-Taussig shunt or a right ventricle to pulmonary artery conduit are the main options for stage 1 surgical palliation for patients born with this condition [2, 3]. The period after the Norwood procedure is considered to be a high-risk period as many complications could arise [4]. Although risk factor identification after the Norwood procedure has increased over the years, most data focus on demographic, preoperative, and surgical risk factors [5,6,7,8]. There is limited information regarding the association of medical interventions such as the type of vasoactive agent selected with clinical outcomes. Therefore, the purpose of these analyses was to use data from a national database to help determine how specific comorbidities and medical interventions impact risk of inpatient mortality in those with hypoplastic left heart syndrome undergoing Norwood procedure. Secondary aims were to determine the impact of these specific comorbidities, interventions, and medications on billed charges, postoperative length of stay, and risk of cardiac arrest.
Methods
As this study utilized deidentified data from a national database, no consents were obtained by the authors of this study. This study is in concordance with the Helsinki declaration.
Pediatric Health Information System Database
Data for this study were obtained from the Pediatric Health Information System (PHIS) database. PHIS is an administrative and billing database that contains inpatient, emergency department, ambulatory surgery, and observation data from not-for-profit, tertiary care pediatric hospitals in the United States. The 53 hospitals that contribute data to PHIS are affiliated with the Children’s Hospital Association (Lenexa, KS), a business alliance of children’s hospitals. Data quality and reliability are assured through a joint effort between the Children’s Hospital Association and participating hospitals. For the purposes of external benchmarking, participating hospitals provide discharge/encounter data including demographics, diagnoses, procedures, and charges. Data are deidentified at the time of data submission, and data are subjected to several reliability and validity checks before being included in the database.
Admission Identification
Pediatric health information systems database data from 2004 to 2015 were utilized for this study. Data from these years were utilized as ICD-9 codes as the identifiers.
Firstly, admissions with hypoplastic left heart syndrome were identified. Of these admissions, those under 2 months of age were then further identified. Next, a Norwood procedure was then identified. As there is no single ICD-9 code for a Norwood procedure, a Norwood procedure was considered to be done when an arch repair and either Blalock-Taussig shunt or right ventricle to pulmonary artery conduit placement was done at the same intervention. Thus, the inclusion criteria for admissions for this study were: (1) diagnosis of hypoplastic left heart syndrome; (2) pediatric admissions under 2 months of age; (3) Norwood procedure identified by arch repair done concomitantly with Blalock-Taussig shunt placement or right ventricle to pulmonary artery conduit. Any admissions not meeting these criteria were excluded. From this point forward, the word “admission” will be used to refer to admissions meeting these inclusion criteria unless otherwise specified.
Admission Characteristics
Several data points were captured for each of the included admissions. Age of admission, gender, year of admission were captured for all admissions. Postoperative length of stay, billed charges, and inpatient mortality were also recorded for all admissions. Any use of “mortality” from here on after will refer to inpatient mortality during the admission of interest.
The presence of specific congenital malformations of the heart were captured using the ICD-9 codes outlined in supplementary Table 1. The presence of specific cardiac surgeries during the admissions were also captured using the ICD-9 codes outlined in supplementary Table 1.
The presence or absence of the following comorbidities was recorded as well: heart failure, tachyarrhythmia, bradyarrhythmia, acute kidney injury, pulmonary hypertension, hypothyroidism, and the presence of syndromes.
Severity of illness measures include the comorbidities listed above. Clinical or laboratory data such as near infrared spectroscopy, serum lactate, or venous saturation were not available for use.
The presence of the following interventions was recorded: need for peritoneal dialysis, continuous renal replacement therapy, peritoneal dialysis, extracorporeal membrane oxygenation.
The presence of the following medications was recorded: epinephrine, norepinephrine, dopamine, dobutamine, milrinone, vasopressin, sodium bicarbonate, calcium chloride, calcium gluconate, angiotensin converting enzyme inhibitor, beta blocker, alpha blocker, aspirin, warfarin, heparin, sildenafil, and inhaled nitric oxide. These were selected as they represent agents frequently used in the postoperative setting and are captured in the database.
Statistical Analyses
Continuous variables were described as median and range, while categorical variables were described as absolute frequency and percentage. Analyses of continuous variables across groups were conducted using a Mann–Whitney U test, while analyses of categorical variables were conducted using a Fisher exact test.
First, the frequency of interventions and medications was quantified by year. This was done to determine trends of use of various interventions throughout the era. An ANOVA was completed to compare variables on year-by-year trend over the study period. Additionally, the frequency of cardiac arrest and inpatient mortality were also quantified by year.
Next a series of regression analyses was conducted. Separate logistic regression analyses were conducted with cardiac arrest and mortality as the dependent variables and the comorbidities, interventions, and medications being included as independent variables. Next, separate linear regression analyses were conducted with billed charges and postoperative length of stay as the dependent variables and with the same independent variables as the prior mentioned regressions. All regressions were conducted as backwards stepwise regressions with 20 iterations using the likelihood ratio selection method. For the logistic regressions, the results are reported as odds ratio with 95% confidence interval, while for the linear regressions, the results are reported as beta-coefficient and p value.
All statistical analyses were conducted using SPSS, Version 23.0. A p value of less than 0.05 was considered statistically significant. Any use of the word “significant” throughout this manuscript implies statistical significance unless otherwise specified.
Results
Cohort Information
A total of 5,138 admissions were identified meeting the inclusion criteria outlined above. Of these a total of 829 (16.1%) experienced inpatient mortality. Of these 5,138 admissions, 352 (6.7%) experienced cardiac arrest. Median billed charges for admissions with survival to discharge were US$422,58 compared to US$743,851 for admissions that experienced inpatient mortality (p < 0.01). Median postoperative length of stay for admissions with survival to discharge was 26.0 days compared to 19.0 days in admissions that experienced inpatient mortality (p = 0.15) (Table 1).
Clinical Outcomes by Year
The frequency of cardiac arrest decreased significantly over the course of the study era. In 2004, the cardiac arrest frequency was 7.4%. This increased and decreased over the study era and was ultimately 4.3% in 2015 (p = 0.04) (Table 2).
The frequency of inpatient mortality did not significantly change over the course of the study era. It was 17.9% in 2004 compared to 15.8% in 2015 (p = 0.06) (Table 2).
Medications by Year
The following medications were used in significantly decreasing frequency when frequency of use was compared between all the years from 2004 to 2015: epinephrine (92.1 to 71.8%, p < 0.01), dopamine (87.1 to 52.3%, p < 0.01), dobutamine (31.3 to 2.5%, p < 0.01), milrinone (88.9 to 71.5%, p < 0.01), vasopressin (10.0 to 6.5%, p < 0.01), sodium bicarbonate (68.9 to 48.9%, p < 0.01), sodium chloride (70.8% versus 42.1%), sodium gluconate (63.4 to 40.6%, p < 0.01), angiotensin converting enzyme inhibitor (51.1% versus 36.8%, p < 0.01), alpha blocker (16.1 to 11.1%, p < 0.01), heparin (46.8 to 21.4%, p < 0.01) (Table 3).
The following medications were used in significantly increasing frequency when frequency of use was compared between 2004 and 2015: beta blocker (5.5 to 12.1%, p < 0.01) and inhaled nitric oxide (1.3 to 10.8%, p < 0.01) (Table 3).
With respect to aspirin there was a statistically significant change. Between 2004 and 2015 the frequency had decreased but between 2004 and 2014 there was a general increase in the use (Table 3).
No significant difference was noted in the frequency of use of norepinephrine, warfarin, and sildenafil (Table 3).
Regression Analyses, Billed Charges
Regression analyses demonstrated the following were associated with a significant increase in billed charges: year of surgery, heart failure, presence of a syndrome, bradyarrhythmia, tachyarrhythmia, acute kidney injury, pulmonary hypertension, dopamine, milrinone, inhaled nitric oxide, nicardipine, aspirin, right ventricle to pulmonary artery conduit (in comparison to Blalock-Taussig shunt), cardiac arrest, and extracorporeal membrane oxygenation.
The following were associated with a significant decrease in billed charges: epinephrine, norepinephrine, sodium bicarbonate, calcium gluconate, calcium chloride, sildenafil, steroids, angiotensin converting enzyme inhibitor, sodium nitroprusside, and continuous renal replacement therapy (Tables 4 and 5).
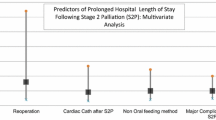
Regression Analyses, Postoperative Length of Stay
Regression analyses demonstrated the following were associated with a significant increase in postoperative length of stay: heart failure, presence of a syndrome, bradyarrhythmia, tachyarrhythmia, acute kidney injury, pulmonary hypertension, nicardipine, aspirin, cardiac arrest, extracorporeal membrane oxygenation.
The following were associated with a significant decrease in postoperative length of stay: epinephrine, norepinephrine, dopamine, sodium bicarbonate, calcium gluconate, calcium chloride, steroids, angiotensin converting enzyme inhibitor, alpha blocker, and sodium nitroprusside (Tables 4 and 5).
Regression Analyses, Cardiac Arrest
Regression analyses demonstrated the following were associated with a significant increase in the odds of cardiac arrest: bradyarrhythmia, tachyarrhythmia, vasopressin, sodium nitroprusside, and continuous renal replacement therapy.
The following were associated with a significant decrease in the odds of cardiac arrest: more recent year of surgery, sodium bicarbonate, calcium chloride, steroids, angiotensin converting enzyme inhibitor, alpha blocker, aspirin, and right ventricle to pulmonary artery conduit (in comparison to Blalock-Taussig shunt) (Tables 4 and 5).
Regression Analyses, Inpatient Mortality
Regression analyses were associated with a significant increase in the odds of inpatient mortality: bradyarrhythmia, tachyarrhythmia, acute kidney injury, pulmonary hypertension, norepinephrine, dopamine, vasopressin, steroids, peritoneal dialysis, continuous renal replacement therapy, cardiac arrest, and extracorporeal membrane oxygenation.
The following were associated with a significant decrease in the odds of inpatient mortality: more recent year of surgery, hypothyroidism, calcium chloride, angiotensin converting enzyme inhibitor, nicardipine, and aspirin (Tables 4 and 5).
Discussion
This study characterizes the frequency of medical interventions and pharmacologic therapies during the Norwood admission for children with hypoplastic left heart syndrome and attempts to model the impact of these on various admission characteristics.
Of interest, is that most pharmacologic therapies were used in decreasing frequency as the study period progressed. This likely represents advancements in surgical technique, cardiopulmonary bypass, perfusion strategy, and postoperative care. Nearly every vasoactive agent, the only exception being norepinephrine, had a significant decrease in use over the study period. The frequency of calcium supplementation, angiotensin converting enzyme inhibitor, alpha blocker, sodium bicarbonate and heparin also all decreased. Despite this, the frequency of cardiac arrest and inpatient mortality did not increase. Only the use of beta blocker and inhaled nitric oxide increased over the study period. Aspirin also increased over the study period as seen by the interval change all the way until the final year did.
One of the major limitations of these analyses is that the temporal relationship of medical interventions and pharmacologic therapies cannot be fully ascertained. However, of the four endpoints of interest, only cardiac arrest would be impacted by this. Billed charges and postoperative length of stay represent a culmination of the entire admission and thus these would be inclusive of all medical interventions and pharmacologic therapies. Inpatient mortality would occur after any of the medical interventions and pharmacologic therapies as well. Thus, only cardiac arrest is susceptible to temporal bias in the sense that a medication like vasopressin, which was found to be associated with increased odds of cardiac arrest, may have been started because of the cardiac arrest and thus would not have contributed to the cardiac arrest risk itself. Thus, the cardiac arrest may have been the trigger for the intervention and not the result of it. However, for medications such as sodium bicarbonate and calcium gluconate, often administered during cardiac arrest, the medications were found to be associated with cardiac arrest which must lead one to question whether administration of these medications may have actually helped prevent some cardiac arrest. Additionally, if a specific intervention or medication was associated with a significant increase or decrease in both cardiac arrest and inpatient mortality, the similar direction of effect on both endpoints raises the likelihood that intervention or medication is causative. Nonetheless, this is all subjective and causation cannot be truly determined from these analyses.
Using some of this logic a few factors deserve particular attention. The following were associated with significant decrease in both cardiac arrest and inpatient mortality: more recent year of surgery, calcium chloride, angiotensin converting enzyme inhibitor, and aspirin. The following were associated with a decrease in only inpatient mortality: nicardipine.
Calcium is essential to cardiovascular physiology as it is deeply related to myocardial contraction and its serum levels are known to decrease after cardiac surgery utilizing cardiopulmonary bypass in children [9]. Although calcium is often cited as having an impact in hemodynamics and systemic oxygen delivery, to our knowledge there are five studies reporting these effects in pediatric cardiac patients, of which only one involves exclusively patients with single ventricle physiology. Savorgnan and colleagues found that calcium chloride boluses used in response to hypotensive episodes led to an improvement in mean blood pressure and pulmonary-to-systemic blood flow ratio without compromising systemic oxygen delivery in patients with single ventricle physiology that had undergone cardiac surgery [10]. Averin and colleagues reported that calcium chloride infusions in pediatric patients in the cardiac intensive care unit (CICU) significantly improved systemic oxygen delivery independently of baseline calcium level [11]. Particularly, neonates had the most improvement, supporting the evidence that extracellular calcium plays an important role in cardiovascular physiology [11, 12]. Additionally, Karki and colleagues demonstrated that the concurrent infusion of calcium chloride and vasopressin in pediatric patients with acute cardiocirculatory failure can improve the hemodynamic status, organ perfusion and overall organ function [13]. Contrarily, Dyke and colleagues suggested that higher calcium supplementation was associated with higher morbidity and mortality [14]. In this study calcium chloride was used to maintain ionized calcium levels above 1.2 mmol/L [14]. Meanwhile, Murray and colleagues did not find differences in hemodynamic status, vasoinotropic score, postoperative length of stay, time to enteral feeding, length of ventilation, or mortality in neonates who received calcium chloride infusions after cardiac surgery compared to those who did not receive the infusion [15]. The mechanism by which calcium chloride improves the hemodynamic status of the patient may be by its inotropic effect and secondary arterial vasoconstriction [11]. The finding of these analyses supports the use of calcium chloride in neonates that have undergone the Norwood procedure. Nevertheless, more studies are needed to further clarify the impact of calcium chloride in this population.
The Norwood procedure involves the creation of a shunt to reestablish the pulmonary circulation, mainly using an artificial shunt in both the MBTS and Sano conduit. This increases the risk of thrombosis due to blood flow alterations, hypercoagulable state, and foreign material exposure [16]. The reported incidence of thrombosis is as high as 40% [17] and is associated with increased length of stay and mortality [18, 19]. Some of the most important risk factors for thrombosis include small shunt size, small infant size, and high levels of perioperative hemoglobin[20]. Although aspirin is often used to reduce the incidence of thrombosis, current studies report conflicting results [21,22,23]. Its effect would be explained by its irreversible inhibition of cyclooxygenase-1 and -2 that leads to inhibition of platelet adhesion and aggregation, and decreased inflammation and infiltration at the thrombus site [24]. The current guidelines by the American College of Chest Physicians recommends patients undergoing Norwood procedure should receive either aspirin or no antithrombotic therapy as compared to prolonged low molecular weight heparin or vitamin K antagonists postoperatively [25]. It should be noted that there are different implications of utilizing aspirin in the setting of an MBTS versus a Sano conduit. As the MBTS has a smaller diameter than a Sano conduit, the risk of thrombosis is greater. But as frequency of MBTS or Sano conduit varies, the use of aspirin may also vary directly as a result.
The following were associated with significant increase in both cardiac arrest and inpatient mortality: bradyarrhythmia, tachyarrhythmia, vasopressin, and continuous renal replacement therapy. The following were associated with an increase in only inpatient mortality: acute kidney injury, pulmonary hypertension, norepinephrine, dopamine, peritoneal dialysis, cardiac arrest, and extracorporeal membrane oxygenation.
Acute kidney injury is common after cardiac surgery and is associated with poor outcomes [26, 27]. This analysis is in alignment with previous studies that demonstrate acute kidney injury after Norwood is associated with increased mortality. In a retrospective cohort by Wong and colleagues, 75% of their patients developed AKI with 21% developing severe AKI after stage 1 palliation [28]. Severe AKI in this cohort was significantly associated with continuous intravenous loop diuretic infusion, need for ECMO, and in-hospital death [28]. Additionally, AKI was found to be an independent risk factor for developing AKI after stage 2 palliation and with prolonged duration of mechanical ventilation after stage 3 palliation [28]. More studies are needed to further understand AKI in single ventricle patients after undergoing stage 1 palliation, particularly for assessing the long-term implications of AKI in this patient population [29].
Tachyarrhythmias are not an uncommon postoperative complication after the Norwood procedure[30]. Postoperative arrhythmias have been associated with higher risk of interstage death [5, 31]. Although mechanistically the cause of the arrhythmias in this patient population is difficult to identify, a prolonged use of vasoactive agents remains as a common risk factor [32]. A retrospective study performed by McFerson and colleagues in patients after Norwood procedure found that the total duration of epinephrine and the highest milrinone dose were both statistically associated with an occurrence of postoperative tachyarrhythmia [32]. Whether tachyarrhythmias themselves directly mediate mortality by reduction of cardiac output or happen to occur in sicker patients already at greater risk for adverse events cannot be elucidated by these current analyses.
In these analyses, the use of vasopressin was associated with increased risk of inpatient mortality and cardiac arrest. The use of vasopressin after cardiac surgery in pediatric patients has been shown in the past to increase systolic and diastolic blood pressure, and to decrease heart rate in patients with biventricular circulation [33]. However, more recent data have challenged this, demonstrating no significant increase in blood pressure. Furthermore, this more recent data demonstrated that even if blood pressure increased with initiation of vasopressin, systemic oxygen delivery did not improve [34,35,36]. It is possible that vasopressin may be utilized in sicker patients or that vasopressin alters the physiology in a negative way. In the setting of parallel circulation, increasing systemic vascular resistance may promote more pulmonary blood flow at the expense of systemic blood flow. This may negatively impact systemic oxygen delivery while also increasing myocardial work required for the maintenance of a certain stroke volume. Additional studies are necessary to clarify the role of vasopressin after the Norwood procedure.
In this study the use of dopamine was associated with an increased risk of inpatient mortality. Dopamine is a precursor of norepinephrine and is commonly used in patients with low cardiac output to increase oxygen delivery (DO2) [37]. With its activation of adrenergic receptors and its action on the central nervous system and the endogenous sympathetic drive, it also increases systemic oxygen consumption (VO2), thus offsetting the improved DO2 [38, 39]. Li and colleagues performed a study in neonates after the Norwood procedure and demonstrated that dopamine negatively affects VO2–DO2 balance and its early termination significantly decreases VO2, thus improving the balance [39]. This analysis further supports that the use of dopamine after undergoing the Norwood procedure should be done with caution.
The evolving understanding of the physiologic state in which the saturation of the blood going to the pulmonary and systemic circulations is equal and the distribution of flow is dependent on the relative resistances of the two circuits has unveiled that, as in any critical illness, maintaining systemic oxygen delivery is the most vital factors. The balance of systemic oxygen delivery and systemic oxygen consumption is what ultimately modulates the risk for hemodynamic decompensation. The systemic venous saturation ultimately underpins the risk for cardiac arrest in patients. Modulating vital signs for the sake of maintaining arbitrarily normal values is likely not beneficial if systemic oxygen delivery is not maintained. The utilization of hypoxic gas admixture with nitrogen in those with this unique circulation is one such example of an intervention that was utilized to maintain what was perceived to be normal saturations in this circulatory state, without actually improving, and potentially even decreasing, systemic oxygen delivery [40,41,42,43].
Systemic oxygen delivery is a function of oxygen content and cardiac output. Thus, systemic oxygen delivery has multiple components which include, but are not limited to, hemoglobin, intravascular volume status, partial pressure of oxygen, blood pressure, and heart rate. Thus, changes in one of these parameters outside of accepted normal may not result in a change in systemic oxygen delivery if another one of these values changes concomitantly. This demonstrates the need for a global evaluation of patients that focuses on the ultimate endpoint of systemic oxygen delivery.
As this concept is better understood and more wholeheartedly adopted, one can understand that interventions and medications utilized to act on specific vital signs may actually not increase systemic oxygen delivery. In fact, increase in vasoactive support to help augment blood pressure may even lead to detrimental effects by increasing myocardial oxygen consumption. Thus, following systemic oxygen delivery by means of venous saturation, near infrared spectroscopy, lactate levels, and/or end organ function is likely to be more helpful than by following individual vital sign parameters in isolation. Targeting interventions based on optimizing systemic oxygen delivery and systemic oxygen consumption have already been demonstrated to improve short-term outcomes and have been demonstrated to improve some long-term outcomes as well [44,45,46,47,48,49,50]. These data offer some preliminary insights into general trends. These are not patient, nor event specific, however. These current data cannot be generalized into all clinical situations even in this specific patient population. But they do offer a starting point.
While these analyses offer valuable, novel insight, they are not without their limitations. Firstly, the temporal relationship of interventions is not known from the data provided in the database. But as pointed out before, three of the four endpoints (billed charges, postoperative length of stay, and inpatient mortality) modeled are reflective of the entirety of the admission. None of these things can occur before the culmination of the admission. Thus, the only endpoint which may be impacted by this limitation is cardiac arrest. Additionally, doses and duration of medications cannot be extracted from the database. Thus, these cannot be commented on. Regardless, the purpose of these analyses was not to establish causal relationships but simply characterize associations to provoke thought and help stimulate the development of hypothesis that can help guide future studies.
Another limitation of these analyses is that baseline demographics and clinical variables reflecting severity of illness and systemic oxygen delivery are not available from the database. Severity of illness can be gauged, to some degree, by the comorbidities included but this is by no means a complete surrogate.
Yet another limitation is the low frequency of use of some interventions or medications. This issue was present only for a few interventions such as warfarin or sildenafil. As this reflects clinical practice this may not even be a true limitation. The vast amount of data in the database allows for adequate power with respect to most of the interventions and medications included in these analyses. PHIS data are based on administrative information and weights are not contained within; therefore, this information was not part of the analyses.
All statistical analyses are also with their limitations. Statistics, in and of themselves, are based on human construct such as an arbitrary selection of significance levels for p values. The statistical tests ran for these analyses are not without their limitations but were selected as being among the most appropriate tests to answer the questions being posed. The use of stepwise regressions versus more “contemporary” Bayesian methods is beyond the scope of this manuscript but warrants brief mention. Backward stepwise regression using likelihood ratios for selection have been demonstrated by some studies to offer equal, and in some cases, better model quality when compared to Bayesian models [51]. To further strengthen the stepwise approach, the variables of interest entered into the models were selected a priori with some previous, albeit, potentially anecdotal thought. This helps strengthen the reproducibility, stability, and interpretation of resulting models.
Despite the limitations, we feel these analyses offer a novel insight into the frequency and impact of comorbidities, interventions, and medications on characteristics of the Norwood admission for children with hypoplastic left heart syndrome. We stress, however, that these findings are limited due to their source from a national administrative database. The associations delineated here with specific outcomes should be utilized as pilot data to be used for hypothesis generation. The benefit being that future studies, retrospective or prospective, can be designed using some of the findings here. All the associations here warrant further, more specific delineation and all the associations here represent global phenomena and there may be patient or situation specific considerations for any intervention.
Conclusion
In Norwood admission for patients with hypoplastic left heart syndrome, the frequency of pharmacologic therapies and cardiac arrest has decreased over time. There are significant associations between acute kidney injury, arrythmias, and pulmonary hypertension with cardiac arrest and mortality.
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Noonan JA, Nadas AS (1958) The hypoplastic left heart syndrome; an analysis of 101 cases. Pediatr Clin North Am 5(4):1029–1056. https://doi.org/10.1016/s0031-3955(16)30727-1
Norwood WI, Lang P, Casteneda AR, Campbell DN (1981) Experience with operations for hypoplastic left heart syndrome. J Thorac Cardiovasc Surg 82(4):511–519
Ohye RG, Schranz D, D’Udekem Y (2016) Current therapy for hypoplastic left heart syndrome and related single ventricle lesions. Circulation 134(17):1265–1279. https://doi.org/10.1161/circulationaha.116.022816
Ishino K, Stümper O, De Giovanni JJ, Silove ED, Wright JG, Sethia B et al (1999) The modified Norwood procedure for hypoplastic left heart syndrome: early to intermediate results of 120 patients with particular reference to aortic arch repair. J Thorac Cardiovasc Surg 117(5):920–930. https://doi.org/10.1016/s0022-5223(99)70373-9
Hehir DA, Dominguez TE, Ballweg JA, Ravishankar C, Marino BS, Bird GL et al (2008) Risk factors for interstage death after stage 1 reconstruction of hypoplastic left heart syndrome and variants. J Thorac Cardiovasc Surg 136(1):94–99. https://doi.org/10.1016/j.jtcvs.2007.12.012
Kobayashi Y, Kotani Y, Kuroko Y, Kawabata T, Sano S, Kasahara S (2020) Norwood procedure with right ventricle to pulmonary artery conduit: a single-centre 20-year experience. Eur J Cardio-Thoracic Surg 58(2):230–236. https://doi.org/10.1093/ejcts/ezaa041
Ghanayem NS, Allen KR, Tabbutt S, Atz AM, Clabby ML, Cooper DS et al (2012) Interstage mortality after the Norwood procedure: results of the multicenter single ventricle reconstruction trial. J Thorac Cardiovasc Surg 144(4):896–906. https://doi.org/10.1016/j.jtcvs.2012.05.020
Simsic JM, Bradley SM, Stroud MR, Atz AM (2005) Risk factors for interstage death after the Norwood procedure. Pediatr Cardiol 26(4):400–403. https://doi.org/10.1007/s00246-004-0776-4
Atsumi N, Abe M, Sakakibara Y, Terada Y, Jikuya T, Tsutsui T et al (1994) Influence of ionized calcium concentration during cardiopulmonary bypass on pediatric cardiac surgery. Kyobu Geka 47(7):544–548
Savorgnan F, Flores S, Loomba RS, Checchia PA, Bronicki RA, Farias JS et al (2021) Hemodynamic response to calcium chloride boluses in single-ventricle patients with parallel circulation. Pediatr Cardiol. https://doi.org/10.1007/s00246-021-02754-3
Averin K, Villa C, Krawczeski CD, Pratt J, King E, Jefferies JL et al (2016) Initial observations of the effects of calcium chloride infusions in pediatric patients with low cardiac output. Pediatr Cardiol 37(3):610–617. https://doi.org/10.1007/s00246-015-1322-2
Seguchi M, Harding JA, Jarmakani JM (1986) Developmental change in the function of sarcoplasmic reticulum. J Mol Cell Cardiol 18(2):189–195. https://doi.org/10.1016/s0022-2828(86)80471-0
Karki KB, Towbin JA, Harrell C, Tansey J, Krebs J, Bigelow W et al (2019) Concurrent use of calcium chloride and arginine vasopressin infusions in pediatric patients with acute cardiocirculatory failure. Pediatr Cardiol 40(5):1046–1056. https://doi.org/10.1007/s00246-019-02114-2
Dyke PC 2nd, Yates AR, Cua CL, Hoffman TM, Hayes J, Feltes TF et al (2007) Increased calcium supplementation is associated with morbidity and mortality in the infant postoperative cardiac patient. Pediatr Crit Care Med 8(3):254–257. https://doi.org/10.1097/01.Pcc.0000260784.30919.9e
Murray LE, Burchett H, Chowdhury SM, Haney AL, Hassid M, Strelow JR et al (2021) Calcium chloride infusions are not associated with improved outcomes in neonates undergoing cardiac operations. Pediatr Cardiol. https://doi.org/10.1007/s00246-021-02730-x
Silvey M, Brandão LR (2017) Risk factors, prophylaxis, and treatment of venous thromboembolism in congenital heart disease patients. Front Pediatr. https://doi.org/10.3389/fped.2017.00146
Agarwal A, Firdouse M, Brar N, Yang A, Lambiris P, Chan AK et al (2017) Incidence and management of thrombotic and thromboembolic complications following the norwood procedure: a systematic review. Clin Appl Thromb Hemost 23(8):911–921. https://doi.org/10.1177/1076029616679506
White MH, Kelleman M, Sidonio RF, Kochilas L, Patel KN (2020) Incidence and timing of thrombosis after the norwood procedure in the single-ventricle reconstruction trial. J Am Heart Assoc. https://doi.org/10.1161/jaha.120.015882
Manlhiot C, Brandão LR, Kwok J, Kegel S, Menjak IB, Carew CL et al (2012) Thrombotic complications and thromboprophylaxis across all three stages of single ventricle heart palliation. J Pediatr 161(3):513–9.e3. https://doi.org/10.1016/j.jpeds.2012.03.004
Gedicke M, Morgan G, Parry A, Martin R, Tulloh R (2010) Risk factors for acute shunt blockage in children after modified Blalock-Taussig shunt operations. Heart Vessels 25(5):405–409. https://doi.org/10.1007/s00380-009-1219-1
Li JS, Yow E, Berezny KY, Rhodes JF, Bokesch PM, Charpie JR et al (2007) Clinical outcomes of palliative surgery including a systemic-to-pulmonary artery shunt in infants with cyanotic congenital heart disease. Circulation 116(3):293–297. https://doi.org/10.1161/circulationaha.106.652172
Al Jubair KA, Al Fagih MR, Al Jarallah AS, Al Yousef S, Ali Khan MA, Ashmeg A et al (1998) Results of 546 Blalock-Taussig shunts performed in 478 patients. Cardiol Young 8(4):486–490. https://doi.org/10.1017/s1047951100007150
Motz R, Wessel A, Ruschewski W, Bürsch J (1999) Reduced frequency of occlusion of aorto-pulmonary shunts in infants receiving Aspirin. Cardiol Young 9(5):474–477. https://doi.org/10.1017/S1047951100005370
Funk CD, FitzGerald GA (2007) COX-2 inhibitors and cardiovascular risk. J Cardiovasc Pharmacol 50(5):470–479. https://doi.org/10.1097/FJC.0b013e318157f72d
Monagle P, Chan AKC, Goldenberg NA, Ichord RN, Journeycake JM, Nowak-Göttl U, et al. (2012) Antithrombotic therapy in neonates and children. Chest 141(2):e737S–e801S. https://doi.org/10.1378/chest.11-2308
Morgan CJ, Zappitelli M, Robertson CM, Alton GY, Sauve RS, Joffe AR et al (2013) Risk factors for and outcomes of acute kidney injury in neonates undergoing complex cardiac surgery. J Pediatr 162(1):120–7.e1. https://doi.org/10.1016/j.jpeds.2012.06.054
Blinder JJ, Goldstein SL, Lee VV, Baycroft A, Fraser CD, Nelson D et al (2012) Congenital heart surgery in infants: effects of acute kidney injury on outcomes. J Thorac Cardiovasc Surg 143(2):368–374. https://doi.org/10.1016/j.jtcvs.2011.06.021
Wong JH, Selewski DT, Yu S, Leopold KE, Roberts KH, Donohue JE et al (2016) Severe acute kidney injury following stage 1 norwood palliation: effect on outcomes and risk of severe acute kidney injury at subsequent surgical stages. Pediatr Crit Care Med 17(7):615–623. https://doi.org/10.1097/pcc.0000000000000734
Cooper DS, Goldstein SL, Kwiatkowski DM (2016) Acute kidney injury has a long-term impact on survival after stage 1 palliation of univentricular hearts-it’s not just just one and done. Pediatr Crit Care Med 17(7):697–698. https://doi.org/10.1097/pcc.0000000000000768
Hornik CP, He X, Jacobs JP, Li JS, Jaquiss RDB, Jacobs ML et al (2011) Complications after the norwood operation: an analysis of the society of thoracic surgeons congenital heart surgery database. Ann Thorac Surg 92(5):1734–1740. https://doi.org/10.1016/j.athoracsur.2011.05.100
Mahle WT, Spray TL, Gaynor JW, Clark BJ (2001) Unexpected death after reconstructive surgery for hypoplastic left heart syndrome. Ann Thorac Surg 71(1):61–65. https://doi.org/10.1016/S0003-4975(00)02324-9
McFerson MC, McCanta AC, Pan Z, Collins KK, Jaggers J, Da Cruz EM et al (2014) Tachyarrhythmias after the norwood procedure: relationship and effect of vasoactive agents. Pediatr Cardiol 35(4):668–675. https://doi.org/10.1007/s00246-013-0836-8
Farias JS, Villarreal EG, Flores S, Mastropietro CW, Vogel M, Schulz K et al (2021) Effects of vasopressin infusion after pediatric cardiac surgery: a meta-analysis. Pediatr Cardiol 42(2):225–233. https://doi.org/10.1007/s00246-020-02496-8
Burton GL, Kaufman J, Goot BH, da Cruz EM (2011) The use of arginine vasopressin in neonates following the Norwood procedure. Cardiol Young 21(5):536–544. https://doi.org/10.1017/s1047951111000370
Mastropietro CW, Clark JA, Delius RE, Walters HL 3rd, Sarnaik AP (2008) Arginine vasopressin to manage hypoxemic infants after stage I palliation of single ventricle lesions. Pediatr Crit Care Med 9(5):506–510. https://doi.org/10.1097/PCC.0b013e3181849ce0
Loomba RS, Culichia C, Schulz K, Vogel M, Savorgnan F, Flores S et al (2021) acute effects of vasopressin arginine infusion in children with congenital heart disease: higher blood pressure does not equal improved systemic oxygen delivery. Pediatr Cardiol. https://doi.org/10.1007/s00246-021-02667-1
MacCannell KL, McNay JL, Meyer MB, Goldberg LI (1966) Dopamine in the treatment of hypotension and shock. N Engl J Med 275(25):1389–1398. https://doi.org/10.1056/nejm196612222752501
Ensinger H, Weichel T, Lindner KH, Grünert A, Ahnefeld FW (1993) Effects of norepinephrine, epinephrine, and dopamine infusions on oxygen consumption in volunteers. Crit Care Med 21(10):1502–1508. https://doi.org/10.1097/00003246-199310000-00018
Li J, Zhang G, Holtby H, Humpl T, Caldarone CA, Van Arsdell GS et al (2006) Adverse effects of dopamine on systemic hemodynamic status and oxygen transport in neonates after the Norwood procedure. J Am Coll Cardiol 48(9):1859–1864. https://doi.org/10.1016/j.jacc.2006.07.038
Shime N, Hashimoto S, Hiramatsu N, Oka T, Kageyama K, Tanaka Y (2000) Hypoxic gas therapy using nitrogen in the preoperative management of neonates with hypoplastic left heart syndrome. Pediatr Crit Care Med 1(1):38–41
Tabbutt S, Ramamoorthy C, Montenegro LM, Durning SM, Kurth CD, Steven JM et al (2001) Impact of inspired gas mixtures on preoperative infants with hypoplastic left heart syndrome during controlled ventilation. Circulation 104(12 Suppl 1):I159–I164
Ramamoorthy C, Tabbutt S, Kurth CD, Steven JM, Montenegro LM, Durning S et al (2002) Effects of inspired hypoxic and hypercapnic gas mixtures on cerebral oxygen saturation in neonates with univentricular heart defects. Anesthesiology 96(2):283–288
Thomas L, Flores S, Wong J, Loomba R (2019) acute effects of hypoxic gas admixtures on pulmonary blood flow and regional oxygenation in children awaiting norwood palliation. Cureus 11(9):e5693. https://doi.org/10.7759/cureus.5693
Hoffman GM, Ghanayem NS, Kampine JM, Berger S, Mussatto KA, Litwin SB, et al. (2000) Venous saturation and the anaerobic threshold in neonates after the Norwood procedure for hypoplastic left heart syndrome. Ann Thorac Surg 70(5):1515–20; discussion 21. https://doi.org/10.1016/s0003-4975(00)01772-0
Hoffman GM, Mussatto KA, Brosig CL, Ghanayem NS, Musa N, Fedderly RT et al (2005) Systemic venous oxygen saturation after the Norwood procedure and childhood neurodevelopmental outcome. J Thorac Cardiovasc Surg 130(4):1094–1100. https://doi.org/10.1016/j.jtcvs.2005.06.029
Hoffman GM, Niebler RA, Scott JP, Bertrandt RA, Wakeham MK, Thompson NE et al (2021) Interventions associated with treatment of low cardiac output after stage 1 norwood palliation. Ann Thorac Surg 111(5):1620–1627. https://doi.org/10.1016/j.athoracsur.2020.05.068
Hoffman GM, Scott JP, Ghanayem NS, Stuth EA, Mitchell ME, Woods RK et al (2020) Identification of time-dependent risks of hemodynamic states after stage 1 norwood palliation. Ann Thorac Surg 109(1):155–162. https://doi.org/10.1016/j.athoracsur.2019.06.063
Hoffman GM, Tweddell JS, Ghanayem NS, Mussatto KA, Stuth EA, Jaquis RD et al (2004) Alteration of the critical arteriovenous oxygen saturation relationship by sustained afterload reduction after the Norwood procedure. J Thorac Cardiovasc Surg 127(3):738–745. https://doi.org/10.1016/S0022
Tweddell JS, Hoffman GM, Fedderly RT, Berger S, Thomas JP, Jr., Ghanayem NS, et al. (1999) Phenoxybenzamine improves systemic oxygen delivery after the Norwood procedure. Ann Thorac Surg 67(1):161–7; discussion 7–8. https://doi.org/10.1016/s0003-4975(98)01266-1
Tweddell JS, Hoffman GM, Fedderly RT, Ghanayem NS, Kampine JM, Berger S et al (2000) Patients at risk for low systemic oxygen delivery after the Norwood procedure. Ann Thorac Surg 69(6):1893–1899. https://doi.org/10.1016/s0003-4975(00)01349-7
Morozova O, Levina O, Uuskula A, Heimer R (2015) Comparison of subset selection methods in linear regression in the context of health-related quality of life and substance abuse in Russia. BMC Med Res Methodol. https://doi.org/10.1186/s12874-015-0066-2
Acknowledgements
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interest to disclose.
Ethical Approval
These analyses did not require institutional review board approval as they used previously published data that were deidentified. These analyses are in compliance with the Helsinki declaration of 1975 and its subsequent revisions.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Loomba, R.S., Rausa, J., Farias, J.S. et al. Impact of Medical Interventions and Comorbidities on Norwood Admission for Patients with Hypoplastic Left Heart Syndrome. Pediatr Cardiol 43, 267–278 (2022). https://doi.org/10.1007/s00246-022-02818-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-022-02818-y