Abstract
Non-invasive evaluation of right ventricular (RV) systolic function in neonates with pulmonary hypertension (PH) with traditional metrics including RV fractional area change (FAC) and tricuspid annular systolic plane excursion (TAPSE) has improved outcomes. Apical three-chamber (3C) RV–FAC, a novel tripartite assessment of the RV, has recently been described in healthy infants. We assess the utility of 3C RV–FAC and biplane RV–FAC in delayed transitioning and neonatal PH. Echocardiograms for 22 normal infants and 22 infants with PH were retrospectively analyzed for RV systolic function indices including four chamber (4C), 3C, and biplane RV–FAC, TAPSE, Tei index, and RV systolic excursion velocity (S’). 4C, 3C, and biplane RV–FAC correlated with PH severity and was decreased in neonates with PH compared to normal neonates (biplane RV–FAC 31.7 ± 13.4% vs. 41 .9 ± 4.7%, p = 0.002). TAPSE was significantly decreased in neonates with PH, but did not correlate with PH severity. Other RV systolic function metrics were not significantly different between normal neonates and neonates with PH. 3C RV–FAC and biplane RV–FAC are lower in neonates with PH. 3C and biplane RV–FAC may allow for improved assessment of global RV systolic dysfunction in newborns with delayed transitioning or PH compared to the commonly used regional methods.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Enhanced understanding in the non-invasive evaluation of neonatal pulmonary hypertension (PH) has led to improved diagnosis and management [1]. Complete evaluation requires quantitative assessment of right ventricular (RV) systolic function, due to limited accuracy and reliability of qualitative assessment [2]. Methods in the assessment of RV systolic function in neonates include tricuspid annular plane systolic excursion (TAPSE), RV fractional area of change (RV–FAC), RV strain, and RV myocardial performance index [3,4,5,6,7].
TAPSE and RV–FAC are clinically accepted standards for the assessment of RV systolic function in the evaluation of PH with reported normative values in healthy term and preterm infants [5, 6]. Studies have shown a good correlation between MRI-derived RV ejection fraction (EF) and these echocardiographic markers of RV systolic function [8]. However, these measures do not incorporate the entirety of a geometrically complex RV. The traditional assessment of RV systolic function from the apical four chamber (4C) view used for calculating RV–FAC does not include the RV outflow tract and thus is not a true global measure of RV systolic function [7, 9].
Jain et al. demonstrated that FAC obtained from a RV-focused apical three-chamber (3C) view, which demonstrates the tripartite RV including its outflow tract, were higher compared to traditional 4C RV–FAC [7]. We propose that RV–FAC obtained from a RV-focused apical 3C view may add additional insight in the assessment of global systolic function of the tripartite RV in neonates with delayed transitioning and PH. In this study, we evaluated the utility of RV–FAC obtained from the apical 3C view in the assessment of RV systolic function in neonates with delayed transitioning and PH. A biplane FAC obtained by combining the apical 3C and 4C views will also be evaluated.
Methods
The institutional research ethics board approved this retrospective study. Echocardiographic indices of RV systolic function were retrospectively assessed in 22 consecutive newborns with varying severity of delayed transitioning or PH, and in 22 consecutive healthy newborns. Infants with congenital heart disease were excluded. Those with a small patent ductus arteriosus or patent foramen ovale were included. Normative data in newborns of these various functional indices were used as a reference for identifying RV systolic dysfunction [5,6,7]. Classification of delayed transitioning and PH severity was based on Doppler interrogation of the tricuspid regurgitation jet if present, patent arterial duct shunting, and interventricular septal position in end-systole. Echocardiographic parameters were used to classify PH based on RV pressure as mild (> 1/2 to < 2/3 systemic pressure), or moderate to severe (≥ 2/3 systemic pressure).
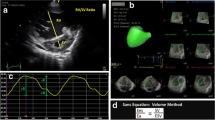
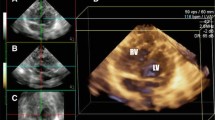
Echocardiography was performed at a mean age of 2 days in both groups. The RV-focused apical 4C view was obtained in the standard fashion [10]. The RV-focused apical 3C view was obtained, as previously described [7]. Briefly, the transducer was rotated counterclockwise from the standard RV 4C view until the left heart was completely out of view, the long axis of the aortic root and ascending aorta was in the center of the image, and there was visualization of the RV inflow, apical trabecular region and outflow. Care was taken not to foreshorten the apex of the RV. This view (Fig. 1) is able to simultaneously visualize the tricuspid valve and RV inflow, the RV apical trabecular component, and the RV outflow and pulmonary valve as well as the inferior and anterior free walls of the RV.
From the RV-focused apical 4C and 3C views, the RV endocardium was contoured, excluding trabeculations, both in end-systole and end-diastole. RV–FAC was calculated as the difference between end-diastolic and end-systolic RV area expressed as a percentage of end-diastolic RV area. Three measurements of RV–FAC from three consecutive cardiac cycles were averaged. The results of 4C and 3C RV–FAC were then averaged to obtain a biplane global RV–FAC. Values were then compared to reported age-dependent normal values [3, 5, 7].
Additional measures of RV function, including, TAPSE, Tei index and the RV S’ were calculated in all patients. TAPSE was measured from a two-dimensional M-mode obtained from the 4C view, positioning the cursor on the lateral tricuspid annulus near the free RV wall and aligning it as close as possible to the apex of the heart [10]. The Tei index, or the myocardial performance index, was calculated as the sum of the isovolumic contraction and the isovolumic relaxation time divided by the ejection time [11]. This measurement, as well as the RV S’ or systolic excursion velocity, was obtained using the 4C view with the sample volume positioned at the lateral tricuspid annulus using pulsed tissue Doppler imaging [12].
Statistical Analysis
All statistical analyses were performed using SPSS 19.0 (SPSS Inc, Chicago, IL). The differences in characteristics between the groups were analyzed. All data were expressed as mean ± SD and median with ranges or percentages depending on the type of data. Multiple groups were initially compared by ANOVA or a Kruskal–Wallis test and then, groups were separately compared using unpaired student’s t test, Mann–Whitney U Test, Fisher’s exact test, or Chi-square tests depending on the type and distribution of the data. Pearson correlation coefficients were calculated to determine the strength of the relationship. Univariate and multivariate regression were performed to assess independent associations. p values < 0.05 were considered statistically significant.
Results
Patient Demographics
A total of 44 patients, 22 with delayed transitioning or PH, and 22 normal neonates were included in the study. Of the delayed transitioning or PH cohort, 14 had moderate to severe PH and 8 had mild PH. The clinical characteristics are noted in Table 1. At the time of the echocardiogram, neonates with PH (n = 22) had a mean age of 2.5 days (range 0–7 days) at a mean gestational age of 35.5 weeks. Normal newborns (n = 22) had a mean age of 2.5 days (range 0–7 days) at a mean gestational age of 38 weeks.
Right Ventricular Systolic Function
Compared with normal neonates, infants with PH had lower 4C, 3C, and biplane RV–FAC (Fig. 2). Also, all three FAC parameters were normal in all newborns in the normal cohort. The cohort with moderate to severe PH had lower RV–FAC and an increased percentage of patients with abnormal RV–FAC compared to the entire cohort of patients with PH. However, traditional RV function parameters like TAPSE indexed to body surface area (BSA), Tei index absolute and indexed to BSA, and S’ mean showed no clinically significant difference in identifying neonates with delayed transitioning or PH (Table 2). TAPSE itself was lower in neonates in the PH cohort and moderate to severe PH cohort compared to normal neonates.
While RV 4C FAC was abnormal only in 50% of all PHN and 71% of moderate-to-severe PHTN groups, both 3C and biplane FAC were abnormal in 59% of all PH and 86% of moderate-to-severe PH cohorts suggesting higher sensitivity of these parameters in identifying these groups. By multivariate logistic regression analysis, biplane FAC was independently associated with PH when adjusted for age, gestational age, RV size and presence of patent ductus arteriosus (odds ratio of 1.13; 95% CI—1.04 to 1.23). Similar independent associations were demonstrated when comparing normal with moderate to severe PH (odds ratio of 1.49; 95% CI—1.14 to 1.94). Biplane RV–FAC had weak correlation with TAPSE (r = 0.59, p < 0.001), Tei index (r = −0.53; p = 0.005) and S’(r = 0.3; p = 0.09) in this cohort.
Discussion
To our knowledge this is the first study evaluating the utility of FAC obtained from the apical 3C view in the assessment of RV systolic function in neonates with delayed transitioning or PH. While cardiac catheterization is the gold standard for diagnosis of PH, echocardiography is frequently used in evaluation of PH in the high-risk population of neonatal PH. Echocardiographic assessment of PH includes assessment of RV systolic function which is challenging due to the complex RV geometry.
RV–FAC is a two-dimensional measure of RV global systolic function, traditionally obtained from an apical 4C view. This 4C assessment is highly reproducible with established reference values in term and preterm infants [5, 13]. 4C RV–FAC has been shown to have moderate correlation with MRI-derived RV systolic function [8, 14]. Studies in adult patients have shown that RV–FAC correlates with RV EF and TAPSE [15, 16]. In addition, RV–FAC was shown to be higher in survivors compared to non-survivors in a population of pediatric patients with idiopathic pulmonary arterial hypertension [17].
While RV–FAC is less sensitive to abnormal geometry and regional abnormalities, it is affected by loading conditions. Further, the 4C RV–FAC does not include the contribution of the RV outflow tract to systolic function. In pediatric patients on prostacyclin therapy, RV–FAC did not significantly increase, while other markers of RV systolic function including TAPSE and RV strain improved over the study period. The authors suggested this may be due to the inability to visualize the entire tripartite RV from the apical 4C view [18]. The use of both apical four- and three- chamber views to calculate a true “global” measure of RV systolic function, similar to the apical views of the left ventricle, is intrinsically appealing [7, 19]. Recent reports have described RV measure of RV–FAC obtained from an apical 3C view in normal neonates demonstrating 3C RV measure of RV–FAC measurements were higher and more reliable compared to 4C RV measure of RV–FAC [7].
The results of the present study show that RV measure of RV–FAC obtained from the 3C view was feasible in all PH and healthy infants. Importantly, 3C RV measure of RV–FAC was associated with increased PH severity in this neonatal population. The RV-focused apical 3C view and the biplane RV measure of RV–FAC obtained by combining the apical 3C and 4C views, may be more sensitive than the conventionally used methods in the evaluation of neonatal PH. The 3C view, by eliminating the contribution of the interventricular septum and including the RV infundibulum, is likely a more accurate estimate of the RV systolic function compared to the conventionally used 4C view.
In contrast to the report of Jain et al. the 3C RV measure of RV–FAC was slightly lower compared to the 4C RV measure of RV–FAC in normal infants [7]. These differences may reflect timing of echocardiograms, as all studies were performed on day of life one and two in the report by Jain et al., while studies were completed within the first week of life in the current study. In contrast, the 3C RV–FAC was slightly higher than the 4C RV–FAC in newborns with delayed transitioning or PH, with a seemingly greater difference between the two measures with increasing severity. This latter finding may additionally be reflective of regional changes which may take place in the pressure-loaded RV. While this is speculation, this suggests the importance of including assessment of all three components of the RV.
Consistent with prior reports, TAPSE was associated with PH with lower TAPSE in neonates with PH compared to normal infants [20, 21]. However, TAPSE did not correlate with the severity of PH in the current study. Additional metrics of RV systolic function including Tei index and S’ mean were not significantly different between neonates with PH and normal neonates. Although there was a trend of increased Tei index in patients with moderate to severe PH. Again, these findings related to the regional assessment of the basal (inflow) RV may point towards the regional effects on the pressure-loaded RV.
There are several limitations of the current study including its retrospective nature, modest sample size, and lack of comparison of the non-invasive assessments of RV systolic function and systolic pressure to a gold standard. Additional studies in a larger cohort should be conducted to confirm the associations of the current study and determine if there is an association with clinical outcomes. In addition, differences in loading conditions in infants with PH due to various different etiologies were not accounted for, although significant congenital heart disease was excluded. Finally other metrics of pulmonary hypertension were not assessed in this cohort including pulmonary artery acceleration time, eccentricity index, or systolic to diastolic duration ratio and future studies should correlate these indices with 3C and biplane RV–FAC.
Conclusions
Right ventricular systolic function is an important determinant of outcomes in neonates with PH. This study demonstrates the feasibility and utility of RV–FAC obtained by a RV-focused apical 3C view and biplane FAC in the non-invasive assessment of RV systolic function in neonates with delayed transitioning and PH. While 3C, 4C, and biplane RV–FAC are all abnormal with worsening neonatal PH, a higher percentage of PH cohort were identified to be abnormal when 3C and biplane FAC were assessed compared to only 4C FAC. This suggests gained insight from this biplane evaluation in the assessment of global RV systolic dysfunction in newborns with delayed transitioning and PH compared to commonly used regional methods.
References
Abman SH et al (2015) Pediatric pulmonary hypertension: guidelines from the american heart association and american thoracic society. Circulation 132(21):2037–2099
Smith A et al (2019) Accuracy and reliability of qualitative echocardiography assessment of right ventricular size and function in neonates. Echocardiography 36(7):1346–1352
Levy PT et al (2013) Feasibility and reproducibility of systolic right ventricular strain measurement by speckle-tracking echocardiography in premature infants. J Am Soc Echocardiogr 26(10):1201–1213
Czernik C et al (2012) Persistently elevated right ventricular index of myocardial performance in preterm infants with incipient bronchopulmonary dysplasia. PLoS ONE 7(6):e38352
Levy PT et al (2015) Right ventricular function in preterm and term neonates: reference values for right ventricle areas and fractional area of change. J Am Soc Echocardiogr 28(5):559–569
Koestenberger M et al (2011) Systolic right ventricular function in preterm and term neonates: reference values of the tricuspid annular plane systolic excursion (TAPSE) in 258 patients and calculation of Z-score values. Neonatology 100(1):85–92
Jain A et al (2014) A comprehensive echocardiographic protocol for assessing neonatal right ventricular dimensions and function in the transitional period: normative data and z scores. J Am Soc Echocardiogr 27(12):1293–1304
Shiran H et al (2014) Relationship between echocardiographic and magnetic resonance derived measures of right ventricular size and function in patients with pulmonary hypertension. J Am Soc Echocardiogr 27(4):405–412
Lopez, L., et al. (2010). Recommendations for quantification methods during the performance of a pediatric echocardiogram: a report from the Pediatric Measurements Writing Group of the American Society of Echocardiography Pediatric and Congenital Heart Disease Council. J Am Soc Echocardiogr, 23(5): 465–495, quiz 576–7.
Rudski, L.G., et al. (2010). Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr, 23(7): 685–713, quiz 786–788.
Vonk MC et al (2007) Right ventricle Tei-index: a tool to increase the accuracy of non-invasive detection of pulmonary arterial hypertension in connective tissue diseases. Eur J Echocardiogr 8(5):317–321
Kossaify A (2015) Echocardiographic assessment of the right ventricle, from the conventional approach to speckle tracking and three-dimensional imaging, and insights into the "right way" to explore the forgotten chamber. Clin Med Insights Cardiol 9:65–75
Breatnach CR et al (2016) Novel echocardiography methods in the functional assessment of the newborn heart. Neonatology 110(4):248–260
Lai WW et al (2008) Accuracy of guideline recommendations for two-dimensional quantification of the right ventricle by echocardiography. Int J Cardiovasc Imaging 24(7):691–698
Sato T et al (2012) Validation study on the accuracy of echocardiographic measurements of right ventricular systolic function in pulmonary hypertension. J Am Soc Echocardiogr 25(3):280–286
Ghio S et al (2002) Usefulness and limits of transthoracic echocardiography in the evaluation of patients with primary and chronic thromboembolic pulmonary hypertension. J Am Soc Echocardiogr 15(11):1374–1380
Kassem E, Humpl T, Friedberg MK (2013) Prognostic significance of 2-dimensional, M-mode, and Doppler echo indices of right ventricular function in children with pulmonary arterial hypertension. Am Heart J 165(6):1024–1031
Hopper RK et al (2018) Right ventricular function mirrors clinical improvement with use of prostacyclin analogues in pediatric pulmonary hypertension. Pulm Circ 8(2):2045894018759247
Rajagopal S et al (2014) Comprehensive assessment of right ventricular function in patients with pulmonary hypertension with global longitudinal peak systolic strain derived from multiple right ventricular views. J Am Soc Echocardiogr 27(6):657–665.e3
Kurath-Koller S et al (2019) Normal pediatric values of the subcostal tricuspid annular plane systolic excursion (s-tapse) and its value in pediatric pulmonary hypertension. Can J Cardiol 35(7):899–906
Aggarwal S, Agarwal P, Natarajan G (2019) Echocardiographic prediction of severe pulmonary hypertension in neonates undergoing therapeutic hypothermia for hypoxic-ischemic encephalopathy. J Perinatol 39(12):1656–1662
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chikkabyrappa, S.M., Critser, P., Roane, J. et al. Tripartite Assessment of Right Ventricular Systolic Function in Persistent Pulmonary Hypertension of the Newborn. Pediatr Cardiol 41, 1206–1211 (2020). https://doi.org/10.1007/s00246-020-02376-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-020-02376-1