Abstract
Up to 10% of Fontan patients require pacemakers; an epicardial approach has historically been used. A transvenous approach can be used but carries risk of Fontan obstruction, thromboembolism, and can be technically challenging. The safety and efficacy of these approaches is not well described. The aim of this study was to compare epicardial and transvenous pacemaker outcomes in Fontan patients, specifically, device performance and adverse event rate. A retrospective review was performed on Fontan pacemaker patients followed at a single institution. Thirty-one Fontan pacemaker patients were identified between 1985 and 2017. Twenty-six had an epicardial system, five transvenous, and three converted from epicardial to transvenous. Average atrial lead sensing at placement was 3.23 versus 2.35 mV (p = 0.52) for epicardial and transvenous leads, respectively. Median atrial and ventricular lead longevity was 86.4 versus 98.8 months (p = 0.56) and 73.2 versus 140 months (p = 0.3) with generator longevity of 65.5 versus 73.9 (p = 0.16) months for epicardial versus transvenous systems, respectively. One major complication occurred in a transvenous patient, and two minor complications occurred in epicardial patients. All transvenous patients received warfarin except one, who converted to dabigatran. Epicardial patients received aspirin (n = 20), warfarin (n = 3) or a warfarin/aspirin combination (n = 3). No thromboembolic events occurred. System revision was required in 13 epicardial and 5 transvenous patients. There were two deaths, none related to the pacemaker system. Transvenous pacemakers can be utilized with equal efficacy compared to epicardial pacemakers with trends toward longer lead longevity in transvenous pacemaker systems.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In children with complex congenital heart disease, single-ventricle palliation may be necessary for long-term survival. The final step in single-ventricle palliation is a Fontan operation, of which there are several variations. The classical approach consists of direct cavo-atrial connection to the pulmonary artery. Newer techniques include the lateral tunnel, which utilizes a prosthetic baffle and portion of the lateral atrial wall and an extra-cardiac conduit involving a tube graft conduit to connect the inferior vena cava and the pulmonary artery. In either method, a fenestration can be utilized to reduce pressure in the Fontan circuit.
Regardless of the Fontan subtype, arrhythmias are a common post-operative comorbidity. Sinus node dysfunction is the predominant arrhythmia after Fontan operation and may occur as a result of scarring of the right atrium, damage to right atrium secondary to cannulation, or damage to the sinus node artery intraoperatively. Other atrial tachyarrhythmias can occur as well, with as many as 50% of Fontan patient developing an atrial tachycardia [1, 2].
Postoperatively, pacemaker implantation is commonly required. Previous studies have shown that almost 10% of Fontan patients require postsurgical pacemaker implantation [3]. Historically an epicardial approach has been used, requiring either a sternotomy or thoracotomy. An alternative to the epicardial approach is a transvenous approach. The transvenous approach is standard of care for atrial pacing in biventricular hearts as it provides superior pacing and sensing thresholds, lower lead current, and longer lead longevity [4]. The transvenous approach has not been commonly used in the Fontan population due to concern for multiple complications including Fontan pathway obstruction and thrombus formation. In addition, accessing myocardial tissue can be technically challenging in an extra-cardiac conduit [5, 6].
Currently, there is little information comparing the long-term safety and efficacy of these two approaches. The aim of this study was to compare epicardial and transvenous pacemaker results in Fontan patients by evaluating device performance and rate of adverse events.
Methods
A retrospective chart review was performed on Fontan patients followed at the University of Iowa Stead Family Children’s Hospital between 1985 and 2017 who had undergone pacemaker placement via either a transvenous, epicardial, or hybrid approach. Patients received regular follow-up and pacemaker interrogation occurred on a scheduled basis. University of Iowa Institutional Review Board approval was obtained for this study.
Thirty-one patients were identified from the original cohort having had both a Fontan operation and pacemaker placement. Of these, twenty-six initially had an epicardial pacemaker placed, while five had a transvenous pacemaker. Three patients who initially had an epicardial pacemaker placed were eventually converted to transvenous pacemakers.
Atrial sensitivity was compared at implantation of the pacemaker device as well as the atrial sensitivity threshold at the subject’s most recent clinic visit. Pacemaker sensitivity was defined as minimum intra-cardiac signal that was sensed by pacemaker to initiate the pacemaker response. Longevity of the atrial lead, ventricular lead, and generator were also measured as outcome variables. Clinical thromboembolic events were evaluated, and adverse events excluding lead revision were categorized as major and minor adverse events. Lead revisions were assessed separately and accounted for in assessing lead longevity. Minor adverse events were defined as those that did not require re-intervention or hospitalization. Statistical comparisons of the continuous variables were made by non-paired T test, while categorical variables were compared using Chi-squared test.
Results
Demographics for the two patient populations are shown in Table 1. There were no statistically significant differences between the indication for Fontan procedure, age at Fontan procedure, indication for pacemaker, or weight at implantation between the two cohorts. Median time from Fontan to epicardial pacemaker placement was 108 and 132 months for transvenous pacemaker.
Table 2 outlines the transvenous population in more detail. Only one patient in the transvenous population had a transvenous ventricular lead. He was not a candidate for an epicardial pacemaker due to significant scaring. Transvenous access was obtained via radiofrequency tunneling from subclavian vein access through the pulmonary artery into the systemic atria.
All but one patient in the transvenous population received warfarin monotherapy for anticoagulation (Table 3), with one patient receiving dabigatran. In the epicardial group, aspirin monotherapy was the primary anticoagulation/antiplatelet therapy utilized. There were no clinically significant thromboembolic events identified, including pulmonary embolism and stroke, in either group.
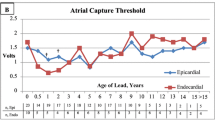
Average atrial sensing (shown in Fig. 1) at placement was 3.23 ± .62 versus 2.35 ± 1.08 mV for epicardial and transvenous leads, respectively (p = 0.52). At the most recent follow-up visit, atrial sensing was 2.91 ± 1.96 mV in the epicardial group and 2.3 ± 1.13 mV in the transvenous leads (p = 0.56). There were too few patients in the cohort to compare ventricular sensing data.
Longevity was defined as duration until replacement was needed without other complication. The mean atrial lead longevity was 86.4 versus 98.8 months in epicardial vs transvenous, while ventricular lead longevity was 73.2 versus 140 months, respectively. Only one patient had a ventricular lead placed transvenously, but had the lead replaced three times. Similarly, generator longevity was 65.5 versus 73.9 months (Table 4). Figure 2, a Kaplan–Meier curve, demonstrates longevity of the pacemakers in the two patient populations. Revision was required in 13 epicardial pacemakers and 5 transvenous patients. The average time to lead revisions in the epicardial group and transvenous groups were 156 and 130 months, respectively. The Fisher exact test statistic value comparing the frequency of revisions was 0.74.
There was one major complication in a transvenous pacemaker patient which was a pocket hematoma requiring hematoma evacuation. There were two minor adverse events, both in the epicardial patient population, of soft tissue/skin infections requiring antibiotic therapy. There were two deaths in the study group, neither related to the pacemaker system.
Discussion
As increasing numbers patients with Fontan physiology are living into adulthood, the incidence of sinus node dysfunction and other atrial arrhythmias is subject to increase, and pacemakers will be required in this population. In non-single-ventricle patients, transvenous pacing is the most common approach, being associated with a lower rate of complications and lower stimulation thresholds compared to the epicardial approach [7]. However, there are very little data regarding the safety of transvenous pacemakers in patients with single-ventricle physiology, or whether transvenous and epicardial system performance is comparable in this complex patient population.
Thromboembolic events are a predominant concern in Fontan patients. Previous research has found the incidence of clinically significant thromboembolism in patients after Fontan procedure is greater than 10% [8], while silent thrombi have been identified on imaging in an even larger percentage of patients. The etiology of the thromboembolic events is not entirely clear, but stagnant venous return and elevated coagulation factors, particularly Factor VIII, likely play a role [9]. Currently, most Fontan patients receive aspirin as long-term anticoagulation or antiplatelet therapy. Studies have shown that this is non-inferior to warfarin [8].
Patients with transvenous pacemakers require additional anticoagulation, and warfarin is commonly used. Identifying the incidence of thromboembolic events in patients with transvenous and epicardial pacemakers is vital to determining which approach should be taken in specific patients. The lack of thromboembolic events is notable from our study, but the sample size was too small to draw further conclusions. In our population, patients underwent only routine clinical follow-up and no additional imaging was done to evaluate for thromboembolisms. In further prospective studies to assess the incidence of thromboembolic events, trans-esophageal echocardiograms may be warranted.
An epicardial approach is associated with inherent increased risk compared to the transvenous approach due to a more invasive surgical procedure. In non-Fontan patients, an epicardial pacemaker has higher pacing thresholds and lower sensing thresholds [10, 11]. The higher pacing threshold in epicardial patients that we identified is consistent with previously established data in dual-ventricle physiology [10, 11]. We found no documented times of any under- or oversensing of atrial tachyarrhythmias in our transvenous population. The limited patient population in our single-center study does not provide enough statistical power to demonstrate any statistical difference in pacing thresholds, but suggests this may be the case.
Ventricular sensing thresholds were not evaluated in our study and ventricular pacing is less common in Fontan patients. Previous research has identified that transvenous pacemakers have a lower ventricular sensing threshold when compared to epicardial in dual-ventricle patients [12].
The higher pacing threshold and lower sensing thresholds that are required in epicardial pacemakers precipitate earlier lead failure, necessitating more frequent replacements when compared to the transvenous population. Our study’s results suggest this finding is consistent in the Fontan population as well, as atrial lead, ventricular lead, and generator longevity were longer in the transvenous population compared to the epicardial population. Again, the limited sample size precludes identifying statistically significant differences. Compared to non-Fontan patients, lead dislodgement was higher in Fontan patients due to the complex anatomy in the transvenous population.
In addition to comparing thromboembolic events, pacing thresholds, and lead longevity, determining whether or not a transvenous approach has other added risk factors is important. Particularly in an extra-cardiac conduit, there is concern regarding the technical components. Previous studies have suggested that pre-procedural mapping of an extra-cardiac tunnel via the jugular vein can provide important information [13]. Determining the incidence of adverse events in this, and other Fontan patients, is vital information. The frequency of these events was limited in our study and larger patient populations are needed to assess the incidence of adverse events.
Limitations of this study include its small sample size and single-center, retrospective nature, which is prone to selection bias. The clinical practice to determine which patients are candidates for transvenous pacemakers likely varies at different institutions. In addition, a retrospective chart review does not permit further investigation into thromboembolic events. In our small patient cohort, that lack of thromboembolic embolic is inconsistent with data from larger studies, and likely does not represent the true incidence.
Conclusion
This study shows a trend toward superior lead performance and generator longevity of transvenous pacemakers in comparison to epicardial pacemakers in Fontan patients. Adverse events were no different between the two groups. A larger multicenter study with longer follow-up will be required to better compare the safety and efficacy of epicardial and transvenous pacing in the Fontan population.
References
Agir AA, Celikyurt U, Karauzum K, Yilmaz I, Ozbudak E, Bozyel S et al (2014) Clinical ventricular tachycardia and surgical epicardial ICD implantation in a patient with a Fontan operation for double-inlet left ventricle. Cardiovasc J Afr 25(6):e6–e10
Deal BJ, Mavroudis C, Backer CL (2007) Arrhythmia management in the Fontan patient. Pediatr Cardiol 28:448–456
Takahashi K, Cecchin F, Fortescue E, Berul CI, Alexander ME, Walsh EP, Fynn-Thompson FR, Triedman JK (2009) Permanent atrial pacing lead implant route after Fontan operation. PACE 32(6):779–785
Shah MJ, Nehgme R, Carboni M, Murphy JD (2004) Endocardial atrial pacing lead implantation and midterm follow-up in young patients with sinus node dysfunction after the Fontan procedure. PACE 27(7):949–954
Arif S, Clift P, De Giovanni J (2016) Permanent transvenous pacing in an extra-cardiac Fontan circulation. Europace 18:304–307
Moore JP, Shannon KM (2014) Transpulmonary atrial pacing: an approach to transvenous pacemaker implantation after extracardiac conduit Fontan surgery. J Cardiovasc Electrophysiol 25(9):1028–1031
Sachweh J, Vazquez-Jimenez J et al (2000) Twenty years experience with pediatric pacing: epicardial and transvenous stimulation. Eur J Cardio-Thorac Surg 17:455–461
Alsaied T (2015) Strategies for thromboprophylaxis in Fontan circulation: a meta-analysis. Heart 101:1731–1737
Viswanathan S (2016) Thromboembolism and anticoagulation after Fontan surgery. Ann Pediatr Cardiol 9(3):236–240
Heinemann M, Gass M, Breuer J, Ziemer G (2003) DDD pacemaker implantation after Fontan-type operations. PACE 26:492–495
Odim J, Suckhow B (2008) Equivalent performance of epicardial versus endocardial permanent pacing in children: a single-institution and manufacturer experience. Ann Thorac Surg 85:1412–1416
Lofty W, Ranya H et al (2013) Permanent Cardiac pacing in pediatric patents. Pediatr Cardiol 34:273–280
O’Leary E, Alexander M et al (2016) Transvenous approach to pacemaker lead implantation for sinus node dysfunction after extra cardiac lateral tunnel Fontan conduit placement. Heart Rhythm Case Rep 2(6):495–498
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interests.
Inform Consent
Regarding human participants, for this type of study no formal consent is required.
Rights and permissions
About this article
Cite this article
Segar, D.E., Maldonado, J.R., Brown, C.G. et al. Transvenous Versus Epicardial Pacing in Fontan Patients. Pediatr Cardiol 39, 1484–1488 (2018). https://doi.org/10.1007/s00246-018-1920-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-018-1920-x