Abstract
Left ventricular outflow tract velocity time integral (LVOT-VTI), a Doppler-derived measure of stroke distance, is used as a surrogate marker of cardiac function in adults. LVOT-VTI is easily obtained, independent of ventricular geometry and wall motion abnormalities. We investigated the relationship between LVOT-VTI and conventional measures of function in young patients by comparing controls to children with dilated cardiomyopathy (DCM). Sixty-two healthy and 52 DCM patients over 1 year were studied retrospectively. The average pulsed (PW) and continuous wave (CW) LVOT-VTIs from apical views were measured from three cycles. Body surface area (BSA) and Ejection fraction (EF) were obtained. We compared LVOT-VTIs between study and control groups and assessed BSA’s impact on LVOT-VTI. The entire cohort was classified into three levels of LV function which were compared. We determined LVOT-VTI cutoff values that indicated an EF <50%. The mean PW-LVOT-VTI in the DCM group was significantly lower than that of the normal group (0.15 vs. 0.18 m; p < 0.0012). The mean CW-LVOT-VTI was significantly lower in DCM (0.20 vs. 0.24 m; p < 0.0001). There was no impact of BSA on LVOT-VTI except when comparing BSA and CW-LVOT-VTI in the normal group. There was a positive relationship between LVOT-VTI and EF for PW (Rs = 0.29, p = 0.0022) and CW (Rs = 0.22, p = 0.0364) and a difference in mean LVOT-VTI between EF groups (p < 0.0001). ROC analysis demonstrated that PW-LVOT-VTI <0.17 m (AUC = 0.73; p < 0.0001) and CW-LVOT-VTI <0.22 m (AUC = 0.76; p < 0.0001) was associated with EF <50%. This study indicates that LVOT-VTI can be a useful alternative measure of LV performance in children over 1 year.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Left ventricular outflow tract velocity time integral (LVOT-VTI) is a Doppler-derived measure of the distance traveled by midstream blood through the left ventricular outflow tract in a single cardiac cycle (i.e., stroke distance). LVOT-VTI is a straightforward parameter to obtain, both by transthoracic and transesophageal echocardiographic images and is easily reproducible with low interobserver variability [1,2,3].
LVOT-VTI has been well described in the adult literature as a useful surrogate marker of cardiac output and global ventricular performance [4, 5]. Studies have validated the correlation between cardiac output measured by stroke distance and cardiac catheterization in adults [5,6,7,8]. Data in adult subjects have also shown that LVOT-VTI is an independent predictor of heart failure [9, 10].
LVOT-VTI has a potential application in describing global ventricular function in children with abnormal ventricular geometries (e.g., single ventricle patients), where traditional echocardiographic measures of ventricular function, such as ejection fraction and fractional shortening, are of limited value. It may also be a useful tool for monitoring ventricular function in the operating room [11]. Although there is some literature describing Doppler-derived stroke distance measurements in healthy children [1, 12,13,14], there are currently no available published data pertaining to LVOT-VTI in children with abnormal ventricular function.
The aim of this study was to determine how LVOT-VTI values vary over a range of ventricular functions in children with normal ventricular geometries and whether these values may be a useful diagnostic tool for identifying children with poor ventricular function. We also investigated how LVOT-VTI varies with Body surface area (BSA) in children in order to determine whether LVOT-VTI should be indexed to BSA in children before using it as a diagnostic tool.
Materials and Methods
Patient Population
A pediatric echo database of transthoracic echocardiograms (TTE) was examined, and patients with normal echocardiograms or with a diagnosis of dilated cardiomyopathy (DCM) between January 2004 and July 2009 were selected. Demographic data extracted from the database included age, BSA, gender, and heart rate. The Stanford University Institutional Review Board approved this study.
Echocardiogram Data
The ultrasound equipment used for the echocardiographic studies was the Siemens Sequoia C512; rev 12.0 (Siemens Medical Solutions USA, Inc., Mountain View, CA) or the Phillips IE33 (Philips Medical Systems, Bothell, WA). All offline measurements were made using syngo Dynamics workstation (Siemens Medical Solutions USA, Inc., Syngo Dynamics Solutions).
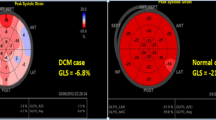
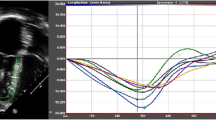
LVOT-VTI was measured from an apical 5 chamber view with the pulsed wave Doppler (PW) sample placed in the LVOT immediately below the hinge points of the aortic valve leaflets (Fig. 1) and continuous wave Doppler (CW) through the entire left ventricular outflow tract/aortic valve/ascending aorta. The outer boundaries of the Doppler signals rather than the modal velocities were traced using a commercially available calibrated offline analysis system. Measurements were taken from three consecutive cardiac cycles and an average obtained in an attempt to minimize the effect of variation of the Doppler velocity and VTI over multiple cardiac cycles. The angle of incidence for VTI for all patients was negligible. The LVOT-VTI average was used for all subsequent data analyses. LVOT-VTI measurements were made by two observers (TT, RP). The ejection fraction data were obtained by performing measurements on the stored images using the 5/6 area-length method [15, 16].
Exclusion criteria included insufficient recordings of apical 5 chamber view to measure LVOT-VTI and missing data regarding body surface area, as well as age less than 1 year, due to the exponential growth rate in infancy.
Statistical Analysis
All data are expressed as mean ± standard deviation or median with a range when appropriate. Unpaired student’s t and Wilcoxin’s two-sample tests were used to calculate differences between groups. Paired data were compared using a paired t test. Spearman correlation coefficients analysis was used to study the influence of body surface area on LVOT-VTI, and to evaluate the relationship between EF and LVOT-VTI. Patients were categorized into one of 3 levels of LV systolic function: Group 1 had severe dysfunction (EF <30%), Group 2 had moderate dysfunction (EF 30–50%), and Group 3 had normal function (EF >50%). An analysis of variance was then conducted to determine if there were differences in the mean LVOT-VTI between different groups. Receiver operating curve characteristics (ROC) analysis was used to determine the threshold value of PW- and CW-derived LVOT-VTI that was associated with decreased ventricular function defined as an EF <50%. A paired t test compared PW and CW-LVOT-VTI values for each subject. A p value of <0.05 was considered significant. Microsoft Excel (Microsoft Corporation, Redmond, WA), and SAS enterprise Guide 5.1 were used for data analysis.
Results
Ninety-two normal and 96 dilated cardiomyopathy patients were initially identified from the database. Of these, 62 normal patients and 54 dilated cardiomyopathy (DCM) patients were used for final data analysis. There was no significant difference in patient characteristics between normal and DCM groups with regard to mean age, BSA or gender (Table 1).
As expected, the median ejection fraction was significantly lower in the DCM group compared with the normal group (p < 0.001, Table 1). The mean PW-derived LVOT-VTI in the DCM group was significantly lower than that of the normal group (0.15 vs. 0.18 m; p < 0.012) (Table 1). The CW-derived LVOT-VTI was also lower in the DCM group compared with the normal group (0.20 vs. 0.24, p < 0.0001). Both PW- and CW-derived LVOT-VTIs correlated with EF (Rs = 0.22–0.29; p = 0.002–0.04).
In the normal patients, there was a positive linear relationship between BSA and CW-LVOT-VTI (Rs = 0.36; p = 0.0057), but not between BSA and PW-derived LVOT-VTI. In DCM patients, there was no relationship between BSA and either PW- or CW-derived LVOT-VTI (Rs = 0.01–0.25; p = 0.15–0.91).
The mean VTI increased across EF categories. The mean LVOT-VTI for the three EF categories across the entire cohort for PW and CW Doppler are shown in Figs. 2 and 3. The mean PW-derived LVOT-VTI corresponding to severe dysfunction, moderate dysfunction, and normal function were 0.13, 0.14, and 0.17 m, respectively. The CW-derived LVOT-VTI corresponding to severe dysfunction, moderate dysfunction, and normal function were 0.19, 0.20, and 0.24 m, respectively. One-way analysis of variance (ANOVA) demonstrated a statistically significant difference in the mean PW- and CW-derived LVOT-VTIs between groups of EF (p = 0.0039 and 0.0014).
The posthoc Bonferroni test demonstrated that the mean PW-derived LVOT-VTI was significantly different only between the normal and severe dysfunction groups. The mean CW-LVOT-VTI was different between the moderate and severe dysfunction groups (p < 0.05 for both). For CW-derived LVOT-VTI, normal function was not different between either moderate or severe dysfunctions.
ROC analysis defined a PW-derived LVOT-VTI <0.17 m as the cutoff for an EF <50% (AUC 0.73; p < 0.0001) (Fig. 4). A CW-derived LVOT-VTI value of <0.22 m was the cutoff for an EF <50% (AUC 0.76; p < 0.0001). The CW-derived Doppler VTI was higher than the PW equivalent for each patient (mean difference of 0.062 m; p < 0.0001).
Discussion
LVOT-VTI is a useful surrogate marker of cardiac output and ventricular performance. It is a useful and efficient method for predicting prognosis in patients with myocardial infarction [17, 18] and VA ECMO [19], impending hospitalization for heart failure [9, 10], and guiding biventricular pacing optimization [2]. In pediatrics, use of LVOT-VTI is hampered by lack of normal values, and lack of relation to conventional measures of LV systolic function.
In studies analyzing the relationship between LVOT-VTI and function, methods of obtaining the Doppler signal vary significantly. Some studies have used nonimaging transducers equipped with CW Doppler, and have assessed aortic VTI from a suprasternal notch window [3, 6,7,8, 11, 20]; however, others have measured the aortic VTI above the level of the aortic valve with PW Doppler [1, 12]. More recently, studies have used the same technique as reported in this investigation, namely using LVOT-PW Doppler immediately proximal to the aortic valve [4, 13, 14, 21]. These differences in technique may account for some variability in results, and in the normal values reported, since the location of the Doppler sampling has a great impact on the velocity, either peak or integrated.
Relationship Between LVOT-VTI and Standard Measures of Function
This study demonstrated a positive and significant relationship between LVOT-VTI by either PW or CW Doppler and EF. The mean LVOT-VTI of patients with an EF of >50% was 0.18 m by PW Doppler, and 0.24 m by CW measurement. Other reported values from an adult study [7] include a mean LVOT-VTI of 0.197 m, whereas a mean aortic VTI of 0.318 m was seen in healthy children [11]. However, the technique of Doppler measurement was different in both these studies which used the technique of a nonimaging CW Doppler probe from the suprasternal notch window.
The mean LVOT-VTI was significantly lower for the study group compared with the control group (0.15 vs. 0.18 m) for the PW Doppler. For the CW Doppler, the trend was the same (0.20 vs. 0.24 m). Thus, patients with normal function had a mean LVOT-VTI of 0.18 m, which means that some patients with normal function had an LVOT-VTI of less than 0.18 m. This contrasts with the findings of an adult study which found that an LVOT-VTI <0.18 m in adults was independently associated with an increased risk for heart-failure hospitalization and mortality [10].
From our data, it appears that the value of 0.17 is a threshold value for decreased EF. Seventy-nine patients fell into the category ‘normal’ ejection fraction even though 17 of these had a history of DCM. Eleven patients in the normal EF group had a PW-LVOT-VTI <0.17 m and of these, 8 patients (73%) had a history of DCM. Thus, the majority of patients with normal ejection fraction but with a PW-LVOT-VTI <0.17 m had a history of DCM.
Influence of BSA on LVOT-VTI
In children over 1 year of age, this study found a weak correlation with LVOT-VTI and BSA using CW Doppler in normal patients, but this was not reproduced in the disease group and we found no correlation using PW Doppler for both groups. A recent study looking at aortic VTI in children showed a strong correlation with BSA between the ages of 0–3 years, which was not seen between the ages of 3–17 years [12]. However, had the authors further subdivided the 0–3 year age group into neonates, infants <1 year and then 1–3 years we may be able to get more detailed information on whether this correlation is mainly due to the effect of rapid growth in children <1 year of age. An earlier study found no significant effect of age or BSA on peak aortic velocity in children [20], and adult studies have shown that neither aortic VTI [5,6,7] nor LVOT-VTI [4, 9, 10] is related to BSA, height or weight. These and our findings suggest that beyond infancy, LVOT-VTI is independent of patient size.
The increase in cardiac output that occurs with patient growth is most likely accomplished by increase of the cross-sectional area of the ventricular outflow, and not due to an increase in stroke distance. It is possible that CW Doppler may increase in normal patients with age secondary to sampling beyond the subaortic region.
Lack of consistency in our study and in the literature of the effect of BSA on LVOT-VTI may be explained by the different methodology used between studies to measure LVOT-VTI in particular whether PW or CW Doppler is used and the angle of insonance.
Application of LVOT-VTI in Clinical Practice
LVOT-VTI is not commonly used in pediatric practice. It has some potential advantages over the traditional measures of global LV function that are currently used in children with congenital heart disease, such as being a function assessment tool that is independent of ventricular geometry. It may be a potentially useful measure for monitoring function in patients with single ventricle physiology. Future studies addressing the application of LVOT-VTI to cardiac diseases affected by abnormal geometries, such as the various types of anatomies in single ventricle physiology, are needed to investigate potential advantages of LVOT-VTI over traditional measures such as EF or FAC.
Our study has shown that in pediatric patients beyond infancy, LVOT-VTI is related to EF and that either a CW-LVOT-VTI <0.22 m or a PW-LVOT-VTI <0.17 m is a threshold value indicating impaired ventricular function. Although statistically significant differences were shown between LVOT-VTI in the normal and diseased groups, the actual numerical difference is small, and this may impact its practical application as a clinical measure on the basis of this study alone. However, this study establishes a threshold value for abnormal ventricular performance that provides a baseline for further studies on other types of ventricular geometries not amenable to conventional echocardiographic assessments of function. In addition, future studies on reliability of LVOT-VTI versus EF between readers will be pursued.
Limitations and Future Directions
The method of LVOT-VTI is based on Doppler assessment of velocities, and is therefore dependent on angle of insonance and (in the case of PW Doppler) site dependent. It is also dependent on the method of Doppler interrogation used—whether it is by PW or by CW Doppler. Future applications of this method should use methods consistent with those reported in this paper if meaningful comparisons to our outcomes are sought. We did not do a comparison between CW and PW Doppler, although the AUCs in the ROC analysis were similar. The range resolution inherent in PW Doppler makes it tempting to advocate for its exclusive use for LVOT-VTI, even though we did not demonstrate superiority of PW over CW. However, we only studied patients with normal anatomy. A more variable population may result in more variability in CW-LVOT-VTI, especially when there are abnormalities of anatomy beyond the LVOT.
We stratified patients based on EF, which has inherent flaws. Because of this stratification approach, some of our control patients had a normal EF but also a history of DCM, which may have influenced the results in this study.
The potential benefit of LVOT-VTI assessment of function lies in its rapid and easy acquisition. It can be a quick way to confirm suspected abnormal function. LVOT-VTI has the potential to assist in the assessment of ventricular function when conventional methods of LV function are difficult, such as in the setting of abnormal geometry, inadequate views, or significant mitral valve regurgitation.
Conclusions
Results from this study indicate that in children over 1 year of age, an LVOT-VTI of either <0.17 m (by PW Doppler) or <0.22 m (by CW Doppler) indicates impaired ventricular function. Patient size has a minimal-to-no impact on LVOT-VTI values, and thus the threshold values cited above are applicable across a range of patient sizes.
References
Hanseus K, Bjorkhem G, Lundstrom NR (1994) Cardiac function in healthy infants and children: Doppler echocardiographic evaluation. Pediatr Cardiol 15(5):211–218
Thomas DE, Yousef ZR, Fraser AG (2009) A critical comparison of echocardiographic measurements used for optimizing cardiac resynchronization therapy: stroke distance is best. Eur J Heart Fail 11(8):779–788
Childs C, Goldring S, Tann W, Hillier VF (1998) Suprasternal Doppler ultrasound for assessment of stroke distance. Arch Dis Child 79(3):251–255
Goldman JH, Schiller NB, Lim DC, Redberg RF, Foster E (2001) Usefulness of stroke distance by echocardiography as a surrogate marker of cardiac output that is independent of gender and size in a normal population. Am J Cardiol 87(4):499–502
Haites NE, McLennan FM, Mowat DH, Rawles JM (1984) How far is the cardiac output? Lancet 324(8410):1025–1027
Mowat DH, Haites NE, Rawles JM (1983) Aortic blood velocity measurement in healthy adults using a simple ultrasound technique. Cardiovasc Res 17(2):75–80
Haites NE, McLennan FM, Mowat DH, Rawles JM (1985) Assessment of cardiac output by the Doppler ultrasound technique alone. Br Heart J 53(2):123–129
Huntsman LL, Stewart DK, Barnes SR, Franklin SB, Colocousis JS, Hessel EA (1983) Noninvasive Doppler determination of cardiac output in man. Clin Validat Circ 67(3):593–602
Stevens SM, Farzaneh-Far R, Na B, Whooley MA, Schiller NB (2009) Development of an echocardiographic risk-stratification index to predict heart failure in patients with stable coronary artery disease: the heart and soul study. JACC Cardiovasc Imaging 2(1):11–20
Ristow B, Na B, Ali S, Whooley MA, Schiller NB (2011) Left ventricular outflow tract and pulmonary artery stroke distances independently predict heart failure hospitalization and mortality: the heart and soul study. J Am Soc Echocardiogr 24(5):565–572
Richardson JR, Ferguson J, Hiscox J, Rawles J (1998) Non-invasive assessment of cardiac output in children. J Accid Emerg Med 15(5):304–307
Pees C, Glagau E, Hauser J, Michel-Behnke I (2013) Reference values of aortic flow velocity integral in 1193 healthy infants, children, and adolescents to quickly estimate cardiac stroke volume. Pediatr Cardiol 34(5):1194–1200
Poutanen T, Tikanoja T, Sairanen H, Jokinen E (2006) Normal mitral and aortic valve areas assessed by three- and two-dimensional echocardiography in 168 children and young adults. Pediatr Cardiol 27(2):217–225
Poutanen T, Tikanoja T, Sairanen H, Jokinen E (2003) Normal aortic dimensions and flow in 168 children and young adults. Clin Physiol Funct Imaging 23(4):224–229
Margossian R, Chen S, Sleeper LA et al (2015) The reproducibility and absolute values of echocardiographic measurements of left ventricular size and function in children are algorithm dependent. J Am Soc Echocardiogr 28(5):549–558
Wyatt HL, Meerbaum S, Heng MK, Gueret P, Corday E (1980) Cross-sectional echocardiography. III. Analysis of mathematic models for quantifying volume of symmetric and asymmetric left ventricles. Am Heart J 100(6 Pt 1):821–828
Trent RJ, Rawles JM (1999) Risk stratification after acute myocardial infarction by Doppler stroke distance measurement. Heart 82(2):187–191
Volpi A, De Vita C, Franzosi MG et al (1993) Determinants of 6-month mortality in survivors of myocardial infarction after thrombolysis. Results of the GISSI-2 data base. The Ad hoc Working Group of the Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto Miocardico (GISSI)-2 Data Base. Circulation 88(2):416–429
Punn R, Axelrod DM, Sherman-Levine S, Roth SJ, Tacy TA (2014) Predictors of mortality in pediatric patients on venoarterial extracorporeal membrane oxygenation. Pediatr Crit Care Med 15(9):870–877
Light LH (1978) Implications of aortic blood velocity measurements in children [proceedings]. J Physiol 285:17–18
Jansen AH, Bracke FA, van Dantzig JM et al (2006) Correlation of echo-Doppler optimization of atrioventricular delay in cardiac resynchronization therapy with invasive hemodynamics in patients with heart failure secondary to ischemic or idiopathic dilated cardiomyopathy. Am J Cardiol 97(4):552–557
Acknowledgements
The authors wish to thank B. Rajaratnam and Sang Oh from the Department of Statistics, Stanford University for their help with the initial statistical analysis and data handling.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Navaratnam, M., Punn, R., Ramamoorthy, C. et al. LVOT-VTI is a Useful Indicator of Low Ventricular Function in Young Patients. Pediatr Cardiol 38, 1148–1154 (2017). https://doi.org/10.1007/s00246-017-1630-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-017-1630-9