Abstract
Mechanical circulatory support in the form of ventricular assist devices (VADs) in children has undergone rapid growth in the last decade. With expansion of device options available for larger children and adolescents, the field of outpatient VAD support has flourished, with many programs unprepared for the clinical, programmatic, and administrative responsibilities. From preimplantation VAD evaluation and patient education to postimplant VAD management, the VAD program, staffed with an interdisciplinary team, is essential to providing safe, effective, and sustainable care for a new technology in an exceedingly complex patient population. Herein, this paper describes the Boston Children’s Hospital VAD experience over a decade and important lessons learned from developing a pediatric program focusing on a high-risk but low-volume population. We highlight the paramount role of the VAD coordinator, clinical infrastructure requirements, as well as innovation in care spanning inpatient and outpatient VAD supports at Boston Children’s Hospital.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The last decade has seen a tremendous growth and evolution in the use of ventricular assist devices (VADs) for the management of heart failure in children. With advancements in VAD technology and expanding clinical experience with pediatric implantation, the indications for VAD implantation in children have broadened from merely a life-sustaining device, to a therapy directed at improving patients’ overall health and happiness. Mirroring the field of adult VAD support, pediatric VADs are now being utilized not only as a bridge-to-transplantation, but also for the purpose of promoting myocardial recovery (bridge-to-recovery, BTR), allowing time for further delineation of care strategies (bridge-to-decision, BTD) and as a permanent therapeutic option (destination therapy, DT) [1,2,3].
The field of pediatric VAD support has followed steadily on the heels of that of adults. The first adult VADs developed in 1960s targeted patients with end-stage heart failure refractory to maximal medical management. The ultimate and original goal of VAD therapy was to solve donor scarcity by providing a technological alternative to heart transplantation. However, it became increasingly evident that early VAD designs were not going to easily supplant heart transplant due to substantial morbidity and mortality associated with implantation and long-term support. In the last five decades, there has been dramatic innovation in VAD’s design with the development of newer generation intracorporeal continuous flow VADs that have overtaken the older generation paracorporeal pulsatile flow devices [4,5,6]. These newer devices have higher survival and substantially lower rate of adverse events such as bleeding, stroke, and infection [4].
Children have benefited from the technological surge and clinical experience garnered in the field of adult VAD support by the increased attention focused on the underserved population of pediatric heart failure patients. Extracorporeal membrane oxygenation (ECMO) has been the mainstay of pediatric mechanical circulatory support due to its applicability to patients of all sizes from infancy to adulthood. However, ECMO has been plagued by the inability for long-term support beyond weeks without accruing significant morbidity and mortality and the inability to easily mobilize and rehabilitate patients [7]. The Berlin Heart EXCOR® was the first pediatric specific device that gained widespread usage due to its higher survival to transplantation and lower adverse event profile compared with ECMO [8]. With the EXCOR®, children could be extubated, fed, ambulated, mobilized, and rehabilitated while awaiting transplantation [9,10,11]. Children could be supported for weeks, months, and even years while awaiting transplantation, all the while remaining, however, in hospital for the duration of their support. The expanding use of the Berlin Heart® highlighted the significant care needs required for these patients and their families—care that extended beyond day-to-day medical management—but also to finding innovative ways of rehabilitating, feeding, mobilizing, and supporting this new expanding cohort and their families [12]. And thus, the pediatric VAD programs began to emerge with a new appreciation for dedicated personnel who had a unique set of skills. One, who could coordinate complex care, was knowledgeable about technical aspect of devices, could educate staff and patients alike, and advocate for these patients within a complex health care system that was unfamiliar to the nuances of VAD care. At our institution, as well as many others, a nurse VAD coordinator was ideally suited for this role.
By 2010, many centers that performed pediatric VAD implantations started using newer generation, intracorporeal devices that were intended for use in adults. Most of these centers were closely integrated with adult VAD programs that facilitated their access to these devices. Most notably was the early experience with intracorporeal axial flow VAD—the HeartMate II® in older children and adolescents [13,14,15]. In 2012, another type of intracorporeal continuous flow VAD—the HeartWare HVAD system®—gained Food and Drug Administration approval for use in adults with heart failure. Its smaller size opened the door for application to the wider pediatric population, and changed the landscape of pediatric VAD support. [16, 17] The HVAD has been utilized in children and adolescents as small as 15 kg for the purpose of bridge-to-transplantation, bridge-to-recovery, and destination therapy [17,18,19,20]. The significant advantage of the HeartWare® device over the EXCOR® has been its ability for hospital discharge, permitting patients to return home and resume activities of daily living: extracurricular activities, play, and school [16, 21, 22]. However, this opportunity for outpatient management has highlighted the complexity of supports required to accomplish and sustain this goal. Questions that we faced included: How do we get these children and their families home? What staffing and programmatic infrastructure is required to care for these patients while in hospital and follow them as outpatients in clinic? Who teaches them about their equipment and their day-to-day care? Who is medically responsible for them in the community? Who manages their anticoagulation? Who manages their other medications? How do we provide psychological support to both the patients and their families? How do we get these children’s back to school? Is there an opportunity to participate in a cardiac rehabilitation program? And the questions go on…
The rapid growth of pediatric VAD support has outpaced the infrastructure and personnel required to sustain it. Many centers are now realizing the tremendous care needs of this unique and high-risk population for whom meticulous attention to detail and continuity of care is paramount to ensure optimal outcomes with this fledging technology.
Herein, we describe our center’s experience developing a pediatric VAD program. We highlight the challenges and opportunities that come from providing comprehensive support to inpatient and outpatient pediatric VAD recipients and their families. We discuss the interdisciplinary approach across the continuum of their care and review the literature related to the development of pediatric VAD programs.
Methods
Origins of a Pediatric VAD Program: Boston Children’s Hospital
Boston Children’s Hospital’s (BCH) Advanced Cardiac Therapies Program evaluates and manages children with systolic and diastolic heart failure due to acquired or congenital heart disease. Since its inception in 1986, Boston Children’s has performed more than 300 heart transplants, making it one of the largest pediatric heart transplant programs in the country. Specialists from Boston Children’s cardiovascular program provide pre- and postoperative care for patients and their families. Current “bridges” to transplant include: the use of continuous vasoactive drugs, extracorporeal membrane oxygenation (ECMO), and ventricular assist devices (VAD).
Pediatric VAD implantation at Boston Children’s Hospital spans the past 10 years. Since the first VAD implant in 2005 to December 2016, surgeons at Boston Children’s Hospital have implanted a total of 63 devices in 55 patients (aged 18 days–23 years). This group is composed of 30 patients supported with the Berlin Heart EXCOR®, seven patients supported with the Abiomed® 5000, four patients supported with the Impella® 2.5, nine patients supported with the RotaFlow Maquet®, and 16 patients supported with the HeartWare® VADs (Table 1).
The formative years of pediatric VAD support consisted of the inpatient management of the Berlin Heart EXCOR®. Clinical care of this device was challenging with a steep learning curve for surgical implantation, management of anticoagulation, and monitoring of the device. In addition, care of these patients was emotionally taxing due to ever present risk of devastating adverse events such as stroke and bleeding. Patients had always been evaluated for possible VAD implantation as a bridge-to-transplantation by the multidisciplinary Heart Failure and Heart Transplant team. The purpose of the evaluation was to identify absolute or relative contraindications to VAD placement and mitigate patient- and device-specific risk factors. Surgical considerations were given special attention, and relevant cardiac imaging studies were reviewed. Following implantation, patients were managed in the cardiac intensive care unit (CICU) by intensivists with the Heart Transplant and Heart Failure team acting as a consultant service providing guidance on anticoagulation initiation, titration, and management. Many of the early EXCOR® patients were participants in the North American Berlin Heart Investigational Device Exemption (IDE) trial [8, 11], using a standardized protocol for their postoperative anticoagulation and VAD care. Anticoagulation decisions were made in consultation with one primary attending physician from the Heart Transplant Team, to ensure consistency and continuity of care. At this time, there was no dedicated VAD nursing staff apart from the Heart Transplant nurse practitioners and a specialized team of CICU nurse competencies for the CICU nursing staff.
Expansion and Redefinition of the VAD Program
The first HeartWare implantation at Boston Children’s Hospital in 2012 compelled restructuring and expansion of the program to accommodate the increase in volume of patients and clinical demands associated with transition to outpatient care. Around the same time, the rapid expansion of adult VAD programs across North America spurred the Joint Commission to formalize credentialing requirements for adult VAD centers (Table 2). While these requirements were not designed for the pediatric population, the Heart Center at Boston Children’s Hospital acknowledged the need to stay ahead of programmatic development by allocating resources to fund device acquisition and dedicated VAD staff.
It Takes a Village: VAD Program Staffing
The VAD Program is staffed by an interdisciplinary team composed of a Medical Director (cardiology attending with specialized training in VAD pre-, peri-, and postimplantation management), Surgical Director (cardiovascular surgeon who primarily implants all VADs and is credentialed for heart transplantation), VAD trained cardiologist, full-time VAD Coordinator, part-time administrative assistant, and dedicated support from social work, palliative care, and inpatient clinical nurse specialists.
The reasons for having a dedicated team of clinicians for this small but complex population included: standardizing clinical care, minimizing medical errors, ensuring continuity of care, fostering therapeutic alliances with patients and their families, enriching our local knowledge, and developing research that can be shared with the community.
Staffing the program with full-time nurse coordinator was paramount to the success of the program, however was no easy feat. Justifying the need of a nurse or nurse practitioner for a program that was in its infancy with a small number of resource intense patients relative to other programs was a significant challenge. To gain support to fund a VAD coordinator position, we referred to the experience garnered by adult VAD programs and the newly emerging Joint Commission requirements for adult VAD programs’ certification. Prominently highlighted throughout the Joint Commission expectation for “Program Management” and “Delivery and Facilitating Clinical Care” was a VAD coordinator (Table 2). Beyond clinical care, the VAD coordinator would also play an important role of managing data entry for the pediatric VAD registry, PediMACS, which at the time was new pediatric arm of the Interagency Registry for Mechanically Assisted Circulation Support (INTERMACS). [2].
The Role of VAD Coordinator
With the support of the on-service VAD attending (two attending physicians with special training in pediatric heart failure and VAD care), the VAD Coordinator assumes primary responsibility for day-to-day clinical management of VAD patients both in the inpatient and outpatient setting. These responsibilities include but are not limited to: daily communication with all outpatient VAD patients, daily inpatient rounds with multidisciplinary team, documenting VAD management recommendations in the electronic medical record (EMR) for inpatients, teaching patients, families, trainees, and staff about device management, data entry into PediMACS on all supported patients, and facilitating evaluations for VAD candidacy.
VAD Evaluation
The VAD team is consulted to evaluate mechanical circulatory support options for patients managed at Boston Children’s Hospital with decompensated heart failure. Referrals are made by their primary cardiologist, cardiac intensive care physician, or cardiovascular surgeon. An order was created in the EMR that allows providers to order a “VAD consult.” Once ordered, the VAD coordinator and the VAD physician utilize an evaluation order set to individualize preoperative assessments while ensuring that all patients receive a minimum set of standard investigations and assessments prior to VAD implantation. The evaluation process for VAD includes the following: (1) educating the potential patient and caregivers on device specifics, risk and benefits of support, and anticipated quality of life on support; (2) laboratory testing and diagnostic imaging to identify medical or anatomic risks or contraindications to VAD; (3) collaboration with Heart Transplant team to determine candidacy; and (4) consultation with social work, psychology, and palliative care team for all patients. Once the evaluation is complete, the VAD Coordinator synthesizes the information and presents the evaluation with the patient’s primary VAD attending to the multidisciplinary VAD team meeting. In addition, the VAD team presents their recommendations at the weekly inpatient Heart Transplant/Heart Failure service meeting. A clear indication for VAD placement is established from the following choices: (1) bridge-to-heart transplantation, (2) bridge to decision, (3) bridge to recovery, or (4) destination therapy.
VAD Implantation Planning
Once a patient is accepted for a VAD implantation, the VAD Coordinator coordinates all the logistics surrounding the implant operation. This includes: collaborating with the device clinical specialists to ensure equipment is available and not close to expiration, ensuring insurance preapproval for device implant has been obtained, setting up device equipment for the OR, completing regulatory paperwork for device implant and managing the patient in the OR under the guidance of the VAD surgeon and attending. The VAD attending remains in the OR for the duration of the implant, adjusting the device parameters based on the patient’s hemodynamics and echocardiogram.
VAD Postoperative Management
The VAD coordinator and the attending physician accompany the patient from the operating room to the CICU, where they provide VAD sign out to the CICU team, outlining the events in the operating room, the settings of the VAD, and the VAD management plan. A postoperative device-specific VAD order set is completed by the VAD coordinator in conjunction with CICU providers. This order set clearly defines the device settings, alarm parameters, hemodynamic parameters, laboratory investigations, antimicrobial plan, and anticoagulation plan. At this time, the VAD coordinator will also provide refresher education to the nursing team, while the VAD attending physician does the same for the CICU-attending physicians and trainees. The CICU team is instructed to call the VAD pager with any changes in device performance, alarms, or increase in bleeding or clotting. The VAD pager is covered 24 hours a day, and answered immediately.
The VAD coordinator takes rounds daily with the interdisciplinary team and writes a daily progress note summarizing the patient’s clinical course, device settings and parameters, device alarms, and plan of care. The VAD team is exclusively responsible for initiation and titration of all anticoagulation and antiplatelet therapy which is vital to reducing variability in anticoagulation levels, as other centers have demonstrated improved outcomes with a select group managing antithrombosis regimes for the pediatric VAD population [23]. As the patient recovers, the VAD coordinator bridges the gap of communication from the CICU to the inpatient step-down cardiac floor by providing updates to nursing administration to assure staffing is adequate to accept the VAD patient on the anticipated transfer date. Once the patient is ready for transfer to the step-down cardiac floor, the VAD Coordinator serves as a clinical resource to the house staff and the nursing staff. Scheduled education sessions are provided in addition to as needed educational offerings to maintain provider comfort in managing the device and competencies. The VAD coordinator takes rounds daily and coordinates long-term care plans. For patients supported on devices that preclude discharge (paracorporeal devices), the VAD coordinator helps implement the long-term goals of care and serves as the fulcrum of the interdisciplinary care team which includes occupational therapy, physiotherapy, speech language pathology, nutrition, feeding team, neurocognitive/neurodevelopment, and palliative care team. An individualized health plan is created with patient-specific goals outlined by providers and family.
Preparing VAD Patients and Families for Discharge
The preparation for outpatient care begins in the preimplant period. During the VAD evaluation, the VAD coordinator identifies obstacles to discharge including medical comorbidities, psychosocial issues, family issues, and financial burdens. We try to address as many of these obstacles early in the VAD course, so that the postoperative VAD period focuses most on patient, family, and community education. The VAD coordinator begins discharge device education with the family when the patient is still in the CICU. This is a good time to initiate discussions regarding parental expectations for discharge and outpatient management. This provides an opportunity to reconcile any discordant views between the family and the VAD team regarding care needs and expectations. Social work spends time with the family identifying social, emotional, and financial obstacles to establishing seamless outpatient care. A checklist has been developed that outlines all the necessary steps prior to discharge (Table 3). First and foremost on that list are patient and family competencies for managing the device and driveline dressing changes. Families universally express anxiety around learning a new technology that is life sustaining for their child. Families find it overwhelming to learn all the didactic material in a short period of time. To alleviate part of their anxiety, fear, and concern, we initiate training early in the postoperative perioperative period and gradually introduce complexity. Utilizing OPENPediatrics® (https://www.openpediatrics.org), we specifically created educational videos for our pediatric population that they can reference from home. The videos review everything from VAD implantation to day-to-day outpatient care. We supply the family with pediatric tailored written material as a reference. We complete hands on teaching with sample devices and batteries for families to gain familiarity and comfort with manipulating the controller and exchanging batteries. We complete training with specifically developed VAD simulation scenarios that are carried out at the Boston Children’s Hospital Simulation Center (http://simpeds.org/) allowing families an opportunity to practice what they have learned in a controlled environment. Based on their performance in the simulation sessions, we then focus additional training to areas that warrant more attention.
Boston Children’s Hospital Outpatient VAD Experience
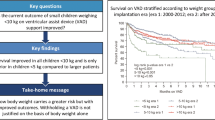
From November 1st 2012 to December 1st 2016, a total of sixteen patients (aged 6–23 years, median 16 years old) have undergone implantation of a HeartWare LVAD® (Table 4). The majority of these patients were adolescents, with the youngest being 6 years of age. The smallest child implanted was 18 kg, with a body surface area of 0.7 m2, and the median weight was 59 kg (range 18–90 kg). All patients had two ventricle circulations with dilated cardiomyopathy being the most common underlying diagnosis. Among the 16 patients, 14 were successfully discharged home and returned to school. Two patients died shortly after implantation in the CICU of multisystem organ failure and did not achieve discharge. The median time to discharge was 31 days (range 17–62 days) with an overall time of support of 114 days (range of 25–656 days). Of the 13 patients discharged, five patients required at least one rehospitalization. All 13 patients resumed school with the youngest attending grade 4 and the oldest attending college and living in residence on campus for over 2 years.
Our 82% rate of discharge home and return to school exceeds what is currently published in the literature [16, 21, 22]. Rossano et al. reported the first Pedimacs registry report on the outcomes of children implanted with durable (long term) continuous flow devices—both HeartWare® VAD and HeartMate II® VAD [22]. Of the 109 children included in the analysis from 35 contributing centers, only 49 (45%) were discharged home. Conditional upon discharge, 30 (61%) patients were rehospitalized at least once. The median duration of support in the Pedimacs was 2.3 months (range 1 day–28 months) which was shorter than our median duration of support of 3.6 months (range 1–21 months). Local expectations for transplant waitlist time are likely to be an important factor that influences pediatric VAD discharge rates. Due to the long waitlist times for pediatric patients in the New England region, we have made it a priority to work toward discharge for all eligible VAD patients, as we expect most waitlist times to fall in the 3–12 months’ range. In addition, we feel that planning for discharge has a positive psychological effect on the patients and their families by focusing their attention on attainable goals of getting home rather than simply waiting for a heart to become available.
Since Rossano et al. publication, other papers have highlighted similar rates of discharge for pediatric patients supported on continuous flow devices [16, 20]. Conway et al. reported the worldwide experience of HeartWare® in 205 children from 34 centers and 12 countries. In this study, 54% of patients were discharged home after VAD implantation after a median duration of hospital stay of 40 days (range 28–71 days) and with a total median duration of support of 86 days (range 24–215 days). We hypothesize that our center has been able to achieve a high discharge rate because longer than average waitlist times allowed for programmatic learning and development of a VAD discharge pathway.
Using Innovative Communication Technology for Managing Technology
Effective communication is one of the major pillars of outpatient VAD management. This includes establishing a simple yet comprehensive way for patients and providers to correspond daily about overall health, VAD parameters, medication changes, future appointments, dressing changes, and new problems. After trialing a home monitoring system (VADWatch ®; Alere™ Standing Stone) with six patients, we created our own home monitoring application—Boston VADKids ® app—that can be used through smartphone, tablet, or computer access (Fig. 1). The application has three purposes: (1) provide a device specific educational resource for the patient/family that is accessible and available in both urgent and non-urgent settings, (2) allow VAD parameters, weight, blood pressure, and temperature for the patient to be entered daily, and (3) facilitate communication between the VAD team and the patient by secure texting. We viewed secure texting as a lynchpin of the application; as many of our patients are adolescents whose primary mode of communication is texting. Benefits of texting include delivery of a secure record of communication to the patient (example: Your INR today was 2.5, please take 5 mg of Coumadin tonight and retest in 1 week). In addition, the secure text feature has been integrated with the smartphone camera allowing the patient/family to send photos of equipment, driveline exit sites, and patients enjoying their life on VAD. We ensure that the secure texts would be answered by a member of the VAD team 24/7. The secure texts can expand to include social work, the cardiovascular surgeon, or members of the Heart Transplant team. In addition, patients have the option to include or exclude their parents on the communications to respect confidentiality and their autonomy. The information input into the application is reviewed daily by the VAD coordinator or the on call VAD attending, and alarms were created to notify the team by email of out of range parameters. Information input into the application is linked to the EMR and can be trended over time. We are currently evaluating the ability of the application to facilitate outpatient management, improve patient and family comfort with the VAD, and augment quality of life. We are hopeful that the application will increase communication and has the potential to decrease rehospitalization and/or adverse events through early identification of problems.
Expanding Indications for Pediatric VAD Support: Laying the Foundation for Destination Therapy VAD
The new generation of intracorporeal continuous flow VADs, such as the HeartWare® and HeartMate II®, have opened the door to the possibility of outpatient VAD management, and with that, expanded the indications for VAD implantation. In the era of paracorporeal VADs such as the Berlin Heart EXCOR®, support could only be considered for the purpose of bridge-to-transplant or recovery as patients had to remain in hospital for the duration of their support. Now with the ability to discharge patients home, destination therapy VAD support could be a consideration for select patients not deemed heart transplantation candidates. The field of DT VAD in adults had already flourished, with a majority of adult VAD implants now being performed for DT rather than as a bridge-to-transplantation [4, 24, 25]. The landmark Randomized Evaluation of Mechanical Assistance in the Treatment of Congestive Heart Failure (REMATCH) trial in adults demonstrated that the implantation of LVADs for DT was superior to standard medical therapy in patients with end-stage heart failure who were not eligible for transplantation [26]. Therefore it is not surprising that consideration of children and adolescents for long-term (permanent) VAD implantation began to progress from a theoretical discussion to a reality. Acknowledging the possibility for many anticipated and unanticipated medical, social, and ethical challenges, a working group at BCH was created in 2013 to begin the discussion surrounding pediatric DT support. This working group consists of VAD surgeons, VAD cardiologists, VAD coordinators, social worker, heart failure cardiologists, cardiac intensivists, cardiac nursing, medical ethicists, palliative care specialists, child life, and community representatives. Over the last three years, a collaborative and multidisciplinary framework for evaluating and consenting/assenting patients and families has been created. The group has also created a framework for withdrawal of care for DT pediatric patients has been created. Many unresolved issues remain; including choice of the best long-term destination therapy device as adult clinical trials of destination therapy using the HeartWare device in the adult population have demonstrated a 30% stroke rate at 2 years follow up, which is much higher than originally anticipated. [27].
Conclusion
VAD management in children requires a well-integrated network of care in the inpatient and outpatient settings. The support of a VAD coordinator has been pivotal to program development and achievement of excellent clinical outcomes. While the field of pediatric VAD support is still in its infancy, we foresee continued evolution of pediatric VAD care in both device utilization and programmatic requirements. We were committed to create a program that in its inception would meet the rigorous expectations of the Joint Commission and were fortunate to have administrative support to make this a realization. However, there are multiple programs nationwide that have smaller surgical volumes, and may have limited resources to validate allocation to a highly specialized but low-volume program. We advocated strongly for a full-time position VAD coordinator, and in doing so have improved patient outcomes by facilitating patient discharge on intracorporeal VADs. This in turn has substantially decreased hospital costs related to long-term VAD therapy and improved inpatient bed utilization. We have also combined the VAD coordinator position with that of the Cardiac Antithrombosis Management Program (CAMP), who oversees standardized anticoagulation and antiplatelet of all patients with acquired or congenital heart disease followed at Boston Children’s Hospital [28]. By doing this, the VAD coordinator’s function covers a wider role of care in the cardiac program, and gains valuable expertise in anticoagulation management which is at the crux of VAD care.
Provision of centralized care to this complex patient population has resulted in institution-specific guidelines for management of the VAD patient, education of providers, patients, and families, and development of VAD-specific quality metrics. We feel that all programs—be it small or large—can expand and improve care if we choose to collaborate and share our clinical expertise on this complex and small-volume population. This extends beyond reporting clinical outcome data to also sharing programmatic guidelines, protocols, and educational material. By doing this, we can collectively save time, resources, and improve standardization of care models across centers.
Reviewing our program over the past 10 years shows favorable clinical outcomes for patients and a high rate of discharge home, as 82% of patients supported on durable devices were discharged home. Future challenges include the need to develop a multicenter standardization of device-specific care—from a standardized approach to antimicrobial, driveline, and anticoagulation management. These endeavors are currently underway through the efforts of pediatric VAD coordinator online consortia that aim to share center‘s experiences and protocols to evaluate care metrics and improve outcomes.
Beyond the goal of ensuring long-term patient survival and freedom from adverse events, a key priority was achieving the highest quality of life for patients and their families. With advancements in our program and technological utilization; our institution has been able to drive our practice beyond improving the quantity of days of support and focusing on the quality of those days. Ozbaran et al. expressed that the new target for VAD support has been identified in that “nothing less than normal” is expected for these children [29]. When faced with a patient who wishes to do something that has never been done before our center, our VAD Program has developed the mindset of finding solutions rather than implementing restrictions. It is not if each obstacle will be overcome but when. With a singular focus on each individual obstacle that will be overcome, we strive to help our VAD patients and their families achieve all of their goals—whatever they might be.
References
Vanderpluym CJ, Fynn-Thompson F, Blume ED (2014) Ventricular assist devices in children: progress with an orphan device application. Circulation 129:1530–1537. doi:10.1161/CIRCULATIONAHA.113.005574
Blume ED, Rosenthal DN, Rossano JW et al (2016) Outcomes of children implanted with ventricular assist devices in the United States: first analysis of the Pediatric Interagency Registry for Mechanical Circulatory Support (PediMACS). J Hear Lung Transplant. doi:10.1016/j.healun.2016.01.1227
VanderPluym CJ, Blume ED (2016) The role of continuous flow ventricular assist device for destination therapy in children: can it work or is it a bridge too far? Prog Pediatr Cardiol 40:25–27. doi:10.1016/j.ppedcard.2016.01.008
Kirklin JK, Naftel DC, Pagani FD et al (2015) Seventh INTERMACS annual report: 15,000 patients and counting. J Hear Lung Transplant 34:1495–1504. doi:10.1016/j.healun.2015.10.003
Kirklin JK, Naftel DC, Stevenson LW et al (2008) INTERMACS database for durable devices for circulatory support: first annual report. J Hear Lung Transplant 27:1065–1072. doi:10.1016/j.healun.2008.07.021
Kirklin JK (2008) Mechanical circulatory support as a bridge to pediatric cardiac transplantation. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. doi:10.1053/j.pcsu.2008.01.006
Thiagarajan RR (2016) Extracorporeal membrane oxygenation for cardiac indications in children. Pediatr Crit Care Med 17:S155–S159. doi:10.1097/PCC.0000000000000753
Fraser CD, Jaquiss RDB, Rosenthal DN et al (2012) Prospective trial of a pediatric ventricular assist device. N Engl J Med 367:532–541. doi:10.1056/NEJMoa1014164
Bryant R, Steiner M, St Louis JD (2010) Current use of the EXCOR pediatric ventricular assist device. J Cardiovasc Transl Res 3:612–617. doi:10.1007/s12265-010-9218-2
Rockett SR, Bryant JC, Morrow WR et al (2008) Preliminary single center North American experience with the Berlin Heart pediatric EXCOR device. ASAIO J 54:479–482. doi:10.1097/MAT.0b013e318184e200
Almond CS, Morales DL, Blackstone EH et al (2013) Berlin heart EXCOR pediatric ventricular assist device for bridge to heart transplantation in US children. Circulation 127:1702–1711. doi:10.1161/CIRCULATIONAHA.112.000685
Hollander SA, Hollander AJ, Rizzuto S et al (2014) An inpatient rehabilitation program utilizing standardized care pathways after paracorporeal ventricular assist device placement in children. J Hear Lung Transplant 33:587–592. doi:10.1016/j.healun.2013.12.009
Cabrera AG, Sundareswaran KS, Samayoa AX et al (2013) Outcomes of pediatric patients supported by the HeartMate II left ventricular assist device in the United States. J Heart Lung Transplant 32:1107–1113. doi:10.1016/j.healun.2013.07.012
Adachi I, Burki S, Zafar F, Morales DL (2015) Pediatric ventricular assist devices. J Thorac Dis 7:2194–2202. doi:10.3978/j.issn.2072-1439.2015.12.61
Chen S, Lin A, Liu E et al (2015) Discharge outcomes in children supported with continuous flow left ventricular assist devices. J Hear Lung Transplant 34:S324
Miera O, Kirk R, Buchholz H et al (2016) A multicenter study of the HeartWare ventricular assist device in small children. J Hear Lung Transplant. doi:10.1016/j.healun.2016.01.019
Miera O, Potapov EV, Redlin M et al (2011) First experiences with the heartware ventricular assist system in children. Ann Thorac Surg 91:1256–1260. doi:10.1016/j.athoracsur.2010.12.013
Padalino MA, Bottio T, Tarzia V et al (2014) HeartWare ventricular assist device as bridge to transplant in children and adolescents. Artif Organs 38:418–422. doi:10.1111/aor.12185
Balciotlu O, Erkul S, Ayik F et al (2012) First successful experience with the heartware assist device in child in Turkey. Cardiovasc Ther 30:29. doi:10.1111/1755-5922.12011_1
Sparks J, Epstein D, Baltagi S et al (2015) Continuous flow device support in children using the HeartWare HVAD: 1000 days of lessons learned from a single center experience. ASAIO J 61:569–573. doi:10.1097/mat.0000000000000253
Conway J, Vanderpluym C, Jeewa A et al (2016) Now how do we get them home? Outpatient care of pediatric patients on mechanical circulatory support. Pediatr Transplant 20:194–202. doi:10.1111/petr.12674
Rossano JW, Lorts A, VanderPluym CJ et al (2016) Outcomes of pediatric patients supported with continuous-flow ventricular assist devices: a report from the Pediatric Interagency Registry for Mechanical Circulatory Support (PediMACS). J Hear Lung Transplant. doi:10.1016/j.healun.2016.01.1228
Byrnes JW, Prodhan P, Williams BA et al (2013) Incremental reduction in the incidence of stroke in children supported with the Berlin EXCOR ventricular assist device. Ann Thorac Surg 96:1727–1733. doi:10.1016/j.athoracsur.2013.06.012
Kirklin JK, Naftel DC, Pagani FD et al (2014) Sixth INTERMACS annual report: a 10,000-patient database. J Hear Lung Transplant 33:555–564. doi:10.1016/j.healun.2014.04.010
Long JW, Kfoury AG, Slaughter MS et al (2005) Long-term destination therapy with the HeartMate XVE left ventricular assist device: improved outcomes since the REMATCH study. Congest Heart Fail 11:133–138
Rose EA, Moskowitz AJ, Packer M et al (1999) The REMATCH trial: rationale, design, and end points. Randomized evaluation of mechanical assistance for the treatment of congestive heart failure. Ann Thorac Surg 67:723–730
Rogers JG, Pagani FD, Tatooles AJ et al (2017) Intrapericardial left ventricular assist device for advanced heart failure. N Engl J Med 376:451–460. doi:10.1056/NEJMoa1602954
Murray JM, Hellinger A, Dionne R et al (2015) Utility of a dedicated pediatric cardiac anticoagulation program: the Boston Children’s Hospital experience. Pediatr Cardiol 36:842–850. doi:10.1007/s00246-014-1089-x
Ozbaran M, Yagdi T, Engin C et al (2015) New era of pediatric ventricular assist devices: let us go to school. Pediatr Transplant 19:82–86. doi:10.1111/petr.12399
Funding
This paper was supported in part by the Alexia Clinton Fund and the Cardiac Transplant Research and Education Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr Francis Fynn-Thompson acts as a proctor/consultant for HeartWare Inc. None of the other authors have any financial or otherwise conflicts of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Hawkins, B., Fynn-Thompson, F., Daly, K.P. et al. The Evolution of a Pediatric Ventricular Assist Device Program: The Boston Children’s Hospital Experience. Pediatr Cardiol 38, 1032–1041 (2017). https://doi.org/10.1007/s00246-017-1615-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-017-1615-8