Abstract
Bleeding and thrombotic events remain a significant cause of morbidity in pediatric patients supported with ventricular assist devices (VADs). The objective of this study is to identify the association between markers of anticoagulation and bleeding and thrombosis events during Berlin Heart ExCor support. A retrospective, single-center analysis of 9 patients supported with the Berlin Heart ExCor was performed. Inflammatory and anticoagulation parameters including C-reactive protein, fibrinogen, partial thromboplastin time (PTT), and platelet count were measured at 48 and 24 h before and after bleeding or thrombosis events. Patients served as their own controls, and the same parameters were measured during a control period where subjects did not experience either event. All patients received the anticoagulation regimen proposed by Berlin Heart. A total of 31 bleeding or thrombotic events were identified and matched to 18 control events. Patient with predominantly thrombotic events tended to weigh less than those with bleeding events (Δ7.7 kg, p < 0.001). PTT levels were higher before and after bleeding (Δ17.36, p = 0.002) and thrombosis (Δ8.75, p < 0.001) events relative to control. Heparin dose decreased after a thrombosis event (Δ−5.67, p = 0.097), and this decrease was significantly different from control (p = 0.032). Non-collinearity between heparin dose and PTT should prompt further inflammatory and hematological investigation. In addition, heavier patients were more prone to bleeding complications. The role of inflammation in the development of thrombus or hemorrhages in the pediatric VAD population needs to be studied further.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pediatric mechanical circulatory support (MCS) has become increasingly utilized to bridge children with end-stage heart failure to transplantation [1, 2]. Although extensive outcome data are limited, heart transplant recipients with pre-transplant ventricular assist device (VAD) or total artificial heart (TAH) support have equivalent survival as compared to transplant without previous MCS, for up to 6 years post-transplantation [2–7]. Furthermore, the introduction of MCS has led to a significant decrease in waiting-list mortality for children awaiting heart transplantation [8–10]. However, VAD therapy in children still lags behind adults in terms of number of available devices and carries higher incidences of bleeding or thrombotic events.
The Berlin Heart ExCor device (Berlin Heart GmbH, Berlin, Germany) is the only widely used durable VAD approved by the FDA as bridge to transplant for the pediatric population [11]. Despite the advanced anticoagulation regimen used as well as the use of recommended, intensive monitoring of platelet function, the rates of thromboembolism resulting in mortality are quoted at 29–42% [12–14]. In infants (<1 year) weighing less than 5 kg, mortality has been quoted at 64% and in congenital heart disease subgroup at 93% with the Berlin ExCor [13]. Furthermore, Berlin ExCor is not approved for destination therapy, so significant neurological injury precluding transplantation candidacy typically translates into mortality after discontinuation of VAD support. Therefore, analysis of factors contributing to thromboembolism or bleeding in these patients may provide insight into improving VAD therapy in children.
Systemic inflammation is known to be triggered by the use of MCS, and the interaction of inflammation and coagulation is increasingly appreciated across a variety of patient populations [15]. Among the pediatric Berlin ExCor population, the use of a steroid protocol has been noted to decrease the degree of inflammatory markers which trigger the coagulation cascade and was associated with a modest decrease in the incidence of cerebrovascular events [16]. Use of thromboelastography (TEG) as a more sophisticated measure of anticoagulation has considerably simplified the clinical manipulation of anticoagulation and antiplatelet therapy; however, TEG is not widely available in all centers [12]. Without TEG, the correlation between inflammatory markers, partial thromboplastin time (PTT), heparin dosage, and thromboembolic events has not clearly been defined in the Berlin Heart Excor population.
With these issues in mind, the goal of the current study was to study the association between markers of anticoagulation and thrombotic/bleeding events in our pediatric Berlin Heart ExCor population.
Methods
Study Population
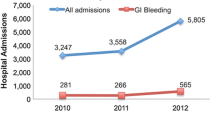
This study was approved by our Institutional Review Board. This single-center retrospective study reviewed the medical records of 9 pediatric patients supported with Berlin Heart EXCOR Pediatric VAD at our center from 2010 to 2015. Relevant medical information was extracted from electronic and physical medical records. All patient data were collected from the time of implantation of the Berlin Heart EXCOR device to time of transplantation or death.
Berlin Heart EXCOR Pediatric VAD was considered for patients with decompensated heart failure who were candidates for heart transplantation and required MCS. All patients were bridge to transplantation only, as the Berlin Heart EXCOR is not approved for destination therapy use.
Anticoagulation Regimen
An anticoagulation regimen recommended by Berlin Heart was followed for all patients. Heparin infusion was started 24-h post implantation if hemostasis was achieved and platelet count was greater than 20,000/μL. Heparin was started at 10 U/kg/h and up titrated to maintain aPTT between 60 and 80 s. Dipyridamole was started at 4 mg/kg/day divided into 4 doses at 48-h post implantation. Low-dose acetylsalicylic acid (ASA) was started 96-h post implantation if there was hemostasis, platelet count greater than 70,000/μL, and all drains were removed. ASA was started at 1 mg/kg/day and was titrated up to 5 mg/kg/day according to the results of twice weekly platelet aggregation studies, with a goal of 70–90% inhibition in response to arachidonic acid. In refractory cases, clopidogrel was used in addition to dipyridamole. Clopidogrel dose was adjusted up to a dose of 1 mg/kg/day for goal inhibition of 60–80%. Warfarin was started when the patient was stable, tolerating oral diet and when aPTT was therapeutic, with a target INR of 2.7–3.5. Heparin was discontinued once INR was stable. Berlin Heart recommends enoxaparin rather than warfarin in patients younger than 12 months, which requires frequent anti-Xa levels on initiation as well as weekly. Our center was not equipped to meet this requirement, and thus warfarin was used. Once patients tolerated a regular diet, they were also supplemented with omega-3 fish oil, vitamin C, and vitamin E.
Initial monitoring of anticoagulation included PTT levels every 6 h, antithrombin III levels daily, and platelet aggregation studies for ASA efficacy twice weekly. Laboratory monitoring was weaned according to dosage stability and as clinically indicated.
Study Endpoints
All patients who underwent Berlin Heart EXCOR Pediatric VAD at our center were included in this study. Clinically documented, significant thrombosis or bleeding events requiring intervention (e.g., transfusion or operative intervention), including all CNS bleeding/thrombosis events, throughout the duration of VAD support were included as study events. All bleeding or thrombosis events were confirmed via echocardiogram or computed tomography scan, with the exception of VAD thrombi, which were confirmed via visual inspection. Thrombosis/bleeding events that were clustered less than 24 h apart in the same patient were considered a single event.
Control events were taken from each patient and designed to represent a neutral time period during each patient’s clinical course. In this way, patients served as their own controls. Control events were defined at the median time between two bleeding/thrombosis events. In the event that only one event occurred in a patient, a control event was obtained at 1 month prior to the first bleeding/thrombosis event. In the event that 3 events occurred, 2 control points were defined using the median time between each consecutive time points. All patients’ data were collected from the time of implantation to the time of transplantation or death.
Variables and Definitions
Weight, temperature, and hematological surrogates of inflammation including white blood cell count (WBC), C-reactive protein (CRP), Antithrombin III, lactate, max temperature (T max), and infectious complications were recorded. Parameters of coagulation including PTT, fibrinogen, and platelet count were tabulated, as well as antiplatelet dose (ASA, dipyridamole, and clopidogrel) and anticoagulant dose (heparin and warfarin).
All values were collected from each patient’s electronic medical record. Variables were recorded for these parameters within a ±48 h timespan of an event, with measures taken at −48, −24, +24, and +48 h as available. Control values for the above parameters were similarly queried for a ±48 h time period at the median point between two successive events, as well as 1 month prior to a patient’s first event, if applicable.
Statistical Analysis
Mixed effects linear regression models were used to examine within-subject differences in variables queried across time between a control condition and thromboembolic or bleeding events. The change in these markers between the control condition and events was assessed with a time × condition interaction, where time was aggregated as pre-event (−48 & −24 h) versus post-event (+24 & +48 h). Models were fitted with a random intercept for subject with random slopes for the event, and time nested within the subject level random effect. The fixed effects in the model were the event indicator (binary), the time indicator (pre vs. post), and the interaction of event-by-time. Analyses were conducted in Stata version 13.1, StataCorp LP (College Station, TX). A p < 0.05 was considered as statistically significant for all analyses performed.
Results
Nine patients underwent Berlin ExCor VAD implantation at our institute during the study period. Of these, 7 underwent LVAD and 2 underwent BIVAD implantation. In these 9 patients, a total of 21 thromboembolic and 10 hemorrhagic events were identified. Using the above control event identification criteria, 18 control events distributed over all 9 subjects were identified.
Eight subjects had bleeding events (average 1.25 events/subject) and 5 subjects had thrombosis events (average 4.2 events/subject). Overall, the first events occurred on 17.44 ± 11.73 days after VAD implantation. First events were thrombosis events in 2 patients (mean time to event: 22 ± 13 days), and bleeding events in 7 patients (mean time to event: 16 ± 12 days). Median duration of VAD support (IQR) was 122 (60–157) days. Of all the events, the BIVAD patients had 6.25% of events, all of which were bleeding events (Table 1).
Weight
There were no differences in patients’ weights temporally surrounding thromboembolic, bleeding, or control events (all p > 0.10). However, when comparing thromboembolic and bleeding events, subjects that had predominantly thrombotic events had an average weight that was 7.7 ± 1.9 kg (p < 0.001) lower than those who had predominantly hemorrhagic events in the pre-event phase (24–48 h prior to event). Similarly, in post-event phase (24–48 h after event), subjects that had predominantly thrombotic events were 7.3 ± 1.5 kg (p < 0.001) lighter than the subjects that had predominantly hemorrhagic events (Table 2).
Anticoagulation Parameters
There were no differences in heparin dose surrounding a bleeding event. Heparin dose approached a significant decrease in patients after thrombotic events (Δ−5.67, p = 0.097) and showed no change in the control condition (Δ0.16, p = 0.87). However, the decrease in heparin after the thrombosis event was significantly different from change in the control events (p = 0.032) (Fig. 1). PTT levels were consistently higher before and after both bleeding (Δ17.36, p = 0.002) and thrombotic (Δ8.75, p < 0.0.001) events relative to the control events (Table 2). Before bleeding events, fibrinogen levels were not different from control (Δ20.58, p = 0.67); however, after the event fibrinogen levels were slightly lower than control (Δ−73.90, p = 0.062) resulting in an interaction effect of bleeding events with time (p = 0.023) (Fig. 2). There were no differences in fibrinogen levels surrounding thrombosis events.
Platelet Function
After bleeding events, platelet levels decreased (Δ−43.10, p = 0.014), and this decrease was significantly different from control events (p = 0.009) where no change was seen. Prior to thrombosis events, platelet levels were not different from controls; however, after the event, platelet levels were lower relative to control events (Δ−80.99, p = 0.032) (Fig. 3).
On examination of antiplatelet medications, there were slightly higher pre-event clopidogrel inhibition levels (Δ17.4.0, p = 0.06) and aspirin inhibition (Δ23.9, p = 0.07) in thrombotic events when compared to controls. Correspondingly, more inhibition by clopidogrel was seen prior to the bleeding events than prior to control events (Δ18.6, p < 0.001) on platelet aggregation studies. This effect continued in the post-event phase as well (Δ17.2, p < 0.001).
Other values examined including Tmax, WBC, CRP, and lactate did not demonstrate significant effects of control versus bleeding or thrombotic event or interactions with time. Patient outcomes, stratified by the presence or absence cerebrovascular event (both bleeding and thrombotic), are presented in Table 3.
Discussion
Heart failure is an increasing problem in the pediatric population with limited VAD options and multiple center-specific anticoagulation regimens with varying results [11]. The incidence of VAD complications due to thrombosis or bleeding continues to be high in the pediatric population. The current study was undertaken to examine the association of markers of inflammation and anticoagulation with thrombotic and hemorrhagic events in the pediatric Berlin Heart EXCOR population.
Our study found several noteworthy relationships. First, in comparing bleeding versus thrombotic events, the mean weight of the patients experiencing thrombotic events was found to be lower than those experiencing hemorrhagic events in both the pre- and post-event phases. Anticoagulation regimens in young children are confounded by differing clotting factor regulation mechanisms and differing pharmacokinetic parameters, and this finding may be due to younger patients being inherently more procoagulable [17, 18]. This relationship may also be due to the smaller pump sizes (10 cc) used in smaller children and requires further study.
When comparing bleeding or thrombotic events to control events, several interesting relationships were noted. In following the anticoagulation protocol proposed by Berlin Heart, several associations between events and coagulation parameters were noted. Heparin dosage was higher in patients prior to thrombotic events when compared to controls and decreased after the event, indicating a possible pattern of heparin resistance prior to thrombus formation, with post-event resolution. Several clotting factors including tissue factor and thrombin are known to increase in activity surrounding sepsis, and heparin itself is known to have anti-inflammatory properties, with non-specific binding to several inflammatory cytokines [19, 20]. Thus, one possible explanation for this pattern is subclinical inflammation leading to heparin resistance and subsequent thrombosis. However, in the current study, no trends in inflammatory markers (e.g., CRP) were noted, although the small sample size and power limits conclusions drawn. Furthermore, more sensitive markers of inflammation including direct measurement of tissue factor/thrombin activity were not available to assess for subtle changes in inflammation.
Despite the pattern of heparin dosage noted, the PTT levels were higher pre-event than control in both bleeding and thrombosis groups. However, all PTT levels were within therapeutic range as designated by Berlin Heart (60–80 s). This inconsistency in the relationship between heparin dose and PTT is interesting and warrants further investigation into mechanisms underlying the development of heparin resistance during VAD support and its association with bleeding/clotting events.
As anticipated, fibrinogen levels were lower post-bleed than in controls likely due to ongoing blood loss. This was mirrored by the platelet levels which decreased following both bleeding and thrombotic events, likely as part of consumptive coagulopathy. The 6-min aggregation in response to clopidogrel was higher pre-bleed than control, which may have contributed to the development of significant bleeding in these patients. This continued after the event as expected likely due to the irreversible binding of clopidogrel to its targeted receptors. Despite slightly higher levels of clopidogrel and aspirin inhibition in the thrombosis group pre-event, thrombosis still occurred, suggesting other mechanisms of coagulation aside from platelet activation—possibly related to inflammatory activation of the coagulation cascade.
In spite of thrombotic and bleeding cerebrovascular events, most of the children had sufficient neurological recovery to undergo heart transplantation (6/9, 67%). Three patients had cessation of VAD support due to prohibitive neurologic injury; two of these children suffered from severe intracerebral hemorrhage, while one suffered a severe cerebral infarction.
The systemic inflammatory response associated with cardiopulmonary bypass has been a topic of interest for many years, and its association with coagulation is becoming increasingly appreciated [15, 21–23]. In the adult LVAD population, infectious complications have been found to be linked to cerebrovascular events, with a proposed mechanism of increased inflammation leading to hypercoagulable states [21, 22]. Specifically in children, the Berlin experience demonstrated that CRP levels greater than 6.3 mg/dL was an independent predictor of in-hospital mortality in children implanted with Berlin Heart ExCor, further highlighting the importance of underlying inflammation in these patients [23]. In a single-center review of 13 children supported with Berlin Hearts, Yu et al. found a positive correlation between CRP and both monocyte count and inotrope use, while they found a negative correlation between CRP and total lymphocyte count [24]. They concluded that a high inflammatory state exists in patients prior to VAD implantation, which subsequently prolongs after VAD implantation. This was worse in children with BIVADs possibly due to their higher INTERMACS stage at the time of implantation [24]. However, the association between elevated CRP and thrombotic events was not specifically highlighted. In our study, we did not find any correlation between pre-event CRP and a bleeding or thrombotic event, although our retrospective study design did not follow complete CRP trends over time, and therefore, we could not adequately evaluate the predictive value of CRP on thrombotic or hemorrhagic events.
The limitations of our study include those inherent to a small retrospective study design. The study design only allowed for point comparisons between event and control and did not allow trending of variables, which may have proven more useful in predicting bleeding/thrombosis events. The heterogeneous patient population results in several confounding variables that may limit the strength of associations that can be drawn. Finally, the small sample size limits statistical power of analyses performed.
Conclusions
In our study, smaller children had more thrombotic events than bigger children who had more bleeding events. The discrepancy in the relationships between medication dosage and anticoagulation/antiplatelet effect should prompt further inflammatory and hematological investigation to better predict bleeding and thrombosis events in the pediatric VAD population.
References
Madriago E, Silberbach M (2010) Heart failure in infants and children. Pediatr Rev 31:4–12
Rossano JW, Dipchand AI, Edwards LB et al (2016) The registry of the International Society for Heart and Lung Transplantation: Nineteenth Pediatric Heart Transplantation Report—2016; focus theme: primary diagnostic indications for transplant. J Heart Lung Transplant 35:1185–1195
Blume ED, Naftel DC, Bastardi HJ et al (2006) Outcomes of children bridged to heart transplantation with ventricular assist devices: a multi-institutional study. Circulation 113:2313–2319
Ezon DS, Khan MS, Adachi I et al (2014) Pediatric ventricular assist device use as a bridge to transplantation does not affect long-term quality of life. J Thorac Cardiovasc Surg 147:1334–1343
Chen JM, Richmond ME, Charette K et al (2012) A decade of pediatric mechanical circulatory support before and after cardiac transplantation. J Thorac Cardiovasc Surg 143:344–351
Lin MH, Chou NK, Chen YS et al (2010) Outcome in children bridged and nonbridged to cardiac transplantation. Transplant Proc 42:916–919
Coskun O, Parsa A, Weitkemper H et al (2005) Heart transplantation in children after mechanical circulatory support: comparison of heart transplantation with ventricular assist devices and elective heart transplantation. ASAIO J 51:495–497
Zafar F, Castleberry C, Khan MS et al (2015) Pediatric heart transplant waiting list mortality in the era of ventricular assist devices. J Heart Lung Transplant 34:82–88
Adachi I, Khan MS, Guzmán-Pruneda FA et al (2015) Evolution and impact of ventricular assist device program on children awaiting heart transplantation. Ann Thorac Surg 99:635–640
van der Muelen MH, Dalinghaus M, Maat AP et al (2015) Mechanical circulatory support in the Dutch National Paediatric Heart Transplantation Programme. Eur J Cardiothorac Surg 48:910–916
VanderPluym CJ, Fynn-Thompson F, Blume ED (2014) Ventricular assist devices in children: progress with an orphan device application. Circulation 129:1530–1537
Fraser CD Jr, Jaquiss RD, Rosenthal DN et al (2012) Prospective trial of a pediatric ventricular assist device. N Engl J Med 367:532–541
Almond CS, Morales DL, Blackstone EH et al (2013) Berlin Heart EXCOR pediatric ventricular assist device for bridge to heart transplantation in US children. Circulation 127:1702–1711
Jordan LC, Ichord RN, Reinhartz O et al (2015) Neurological complications and outcomes in the Berlin Heart EXCOR® pediatric investigational device exemption trial. J Am Heart Assoc. doi:10.1161/JAHA.114.001429
Brix-Christensen V (2001) The systemic inflammatory response after cardiac surgery with cardiopulmonary bypass in children. Acta Anaesthesiol Scand 45:671–679
Byrnes JW, Prodhan P, Williams BA et al (2013) Incremental reduction in the incidence of stroke in children supported with the Berlin EXCOR ventricular assist device. Ann Thorac Surg 96:1727–1733
Dabbous MK, Sakr FR, Malaeb DN (2014) Anticoagulant therapy in pediatrics. J Basic Clin Pharm 5:27–33
Andrew M, Mitchell L, Vegh P, Ofosu F (1994) Thrombin regulation in children differs from adults in the absence and presence of heparin. Thromb Haemost 72:836–842
Allen KS, Sawheny E, Kinasewitz GT (2015) Anticoagulant modulation of inflammation in severe sepsis. World J Crit Care Med 4:105–115
Young E (2008) The anti-inflammatory effects of heparin and related compounds. Thromb Res 122:743–752
Levi M, Keller TT, van Gorp E, ten Cate H (2003) Infection and inflammation and the coagulation system. Cardiovasc Res 60:26–39
Aggarwal A, Gupta A, Kumar S et al (2012) Are blood stream infections associated with an increased risk of hemorrhagic stroke in patients with a left ventricular assist device? ASAIO J 58:509–513
Fan Y, Weng YG, Huebler M et al (2011) Predictors of in-hospital mortality in children after long-term ventricular assist device insertion. J Am Coll Cardiol 58:1183–1190
Yu X, Larsen B, Rutledge J et al (2012) The profile of the systemic inflammatory response in children undergoing ventricular assist device support. Interact Cardiovasc Thorac Surg 15:426–431
Acknowledgements
This work was supported by CTSI Grant UL1TR000124UCLA (Clinical and Translational Science Institute).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None declared.
Rights and permissions
About this article
Cite this article
Iyengar, A., Hung, M.L., Asanad, K. et al. Association Between Hematologic and Inflammatory Markers and 31 Thrombotic and Hemorrhagic Events in Berlin Heart Excor Patients. Pediatr Cardiol 38, 770–777 (2017). https://doi.org/10.1007/s00246-017-1578-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-017-1578-9