Abstract
Critically ill pediatric patients supported on ventricular assist devices (VADs) are increasingly being anticoagulated on bivalirudin, but with difficulty monitoring anticoagulation. Activated partial thromboplastin time (aPTT) has recently been shown to poorly correlate with bivalirudin plasma concentrations, while dTT had excellent correlation. However, aPTT is the more common monitoring test and dTT testing is rarely used. In addition, effects of frequent clinical VAD scenarios (such as inflammation) on the accuracy of aPTT and dTT testing remains uncertain. We reviewed the effects of clinical scenarios (infection/inflammation, chylothorax, and steroids administration) on anticoagulation monitoring in 10 pediatric VAD patients less than 3 years at Cincinnati Children's Hospital Medical Center from 10/27/2020 to 5/6/2022 using bivalirudin for anticoagulation. There were 16 inflammation/infection, 3 chylothorax, and 6 steroids events. Correlation between dTT and aPTT was significantly lower after infection/inflammation, with dTT increasing prior to inflammation/infection while aPTT remained unchanged. In addition, steroids are administered to VAD patients to reduce inflammation and thus additionally stabilize anticoagulation. However, this anticoagulation stabilization effect was reflected more accurately by dTT compared to aPTT. In children requiring VAD support utilizing bivalirudin anticoagulation, inflammation/infection is a common occurrence resulting in anticoagulation changes that may be more accurately reflected by dTT as opposed to aPTT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Critically ill pediatric patients supported on ventricular assist devices (VADs) have historically been anticoagulated with unfractionated heparin (UFH), but with difficulty with therapeutic monitoring and risk of thrombotic and hematologic events [1, 2]. Thus, direct thrombin inhibitors, such as bivalirudin, are increasingly being used in this population [3, 4]. Bivalirudin has a short half-life and the distinct advantage of the ability to bind both free and thrombus-bound thrombin with resultant fibrinolysis [5, 6]. It additionally does not rely on a cofactor for efficacy, while heparin requires antithrombin III (ATIII) for its anticoagulation effects. Neonates, young infants, and critically ill patients are known to have lower ATIII levels [7]. In pediatric VAD patients on UFH, bleeding and thrombosis are both frequent complications, occurring in 37% and 26% of children, respectively [2]. Bivalirudin has thus far demonstrated lower major bleeding and stroke rates with better cost-effectiveness compared to heparin in this population [4, 8,9,10]. Given bivalirudin’s decreased binding to plasma proteins compared to UFH, it may have a more predictable anticoagulation effect than that of UFH [11].
Despite its advantages, bivalirudin monitoring has been difficult in children [2, 12, 13]. There is limited information on its pharmacokinetics in pediatrics and no consistently accepted real-time therapeutic monitoring [14]. Two frequently used laboratory tests include activated partial thromboplastin time (aPTT) and dilute thrombin time (dTT). APTT has been shown to poorly correlate with bivalirudin plasma concentrations by liquid chromatography with tandem mass spectrometry (r2 = 0.1), while correlation between dTT and these concentrations is excellent (r2 = 0.87) [15, 16]. Factors VIII, XI, and XII are activated by artificial surface contact, which may result in altered aPTT in VAD patients. Whether this fully explains the inconsistencies with aPTT in VAD monitoring is unclear [17]. While dTT is reported to have excellent correlation with research-only measurements of bivalirudin levels, the effects of various clinical scenarios on dTT and its correlation with aPTT are also unknown. Better understanding of the relationships of dTT and aPTT in these common VAD scenarios could promote safer utilization of bivalirudin in the pediatric population.
This retrospective cohort study aimed to compare the effects of inflammation, chylothorax and steroid usage on aPTT and dTT results. We hypothesized that aPTT would be more affected by these clinical events, and that correlation between dTT and aPTT would decrease during these evaluated clinical events.
Materials and methods
Patients
This is a single-center retrospective cohort study of all pediatric VAD patients less than 3-year-old anticoagulated with bivalirudin from October 2020 to May 2022. Patient demographics, clinical events, and anticoagulation lab values were collected from the electronic medical record. VAD support type included Berlin Heart EXCOR®, CentriMag™, or PediMag™. This study has been approved by the institutional review board at Cincinnati Children's Hospital (IRB 2022-0508).
Definitions
Inflammation/infection was defined as an increase in CRP above 2 mg/dL, procalcitonin above 0.5 ng/mL, or positive respiratory viral panel or culture (including blood, urine, or respiratory). Chylothorax was defined as the presence of lymphatic fluid in the pleural space secondary to a leak from the thoracic duct or its branches, as determined by clinical documentation (note) or by laboratory data (pleural fluid with elevated triglyceride, cholesterol and/or lymphocyte count). Steroid usage included initiation of any corticosteroid regimen, excluding steroid administration during CPB.
APTT and dTT monitoring
For each clinical event, all paired aPTT and dTT values obtained for 5 days before and 10 days after the event were included. Each patient had between 2 and 4 simultaneously collected aPTT and dTT levels per 24 h. Lab values obtained for the 5 days prior to the clinical event allowed for a baseline correlation of both lab tests to be established before the clinical event. The 15-day paired groupings of aPTT and dTT were separated into groups before and after each clinical event, and then all patient lab values for each group were combined prior to proceeding with analysis.
DTT was obtained using a HemosIL Thrombin Time kit on the ACL Top 750 instrument, with which plasma samples were diluted 1:4 in buffer. Fibrinogen in the test sample was converted to fibrin by the addition of purified bovine thrombin and the time required to form the clot was measured. APTT was obtained using a SynthASil® kit on the ACL Top 550 instrument; plasma samples were incubated at 37 °C with a liquid buffered reagent (which includes synthetic phospholipid for optimal platelet-like activity and a highly defined non-settling colloidal silica for optimal activation of the contact phase of coagulation). Calcium was then added to induce coagulation and time required for clot formation was measured.
Statistical analysis
Data were summarized as median, first and 3rd quartile for continuous variable and frequency for categorical variable. Median, as opposed to mean, was used account for any significant effects from rare lab outliers due to inaccurate lab draws. Differential changes of aPTT and dTT with time were analyzed using mixed model linear regression with a random intercept to account for repeated measurements per subject. Time relative to events was represented as days before events (coded as negative) and days after events (positive). Time-method interaction term was included to test for slope difference between aPTT and dTT before or after events. Correlations between aPTT and dTT before and after specific events were analyzed using aPTT as outcome variable and dTT as explanatory variable with random intercept to account for repeated measures per subject and group–dTT interaction to test for slope (reported standardized beta coefficient) difference before versus after events. All analyses were performed in SAS 9.4 (SAS Institute, Carry, NC). For all statistical tests, a p value < 0.05 was considered significant.
Results
Ten pediatric VAD patients less than 3 years were included in this study; 5 had single ventricle physiology, 3 had cardiomyopathy, and 2 had biventricular congenital heart disease (Table 1). Seven patients were supported on a Berlin Heart EXCOR® and three on a CentriMag™ (with one patient being transitioned to and one patient transitioned from PediMag™ to CentriMag™ while on bivalirudin). VAD implant duration ranged from 30 to 155 days (median 84, IQR 35–124 days). Incidence of clinical events included 16 events of inflammation, 3 of chylothorax, and 6 of steroids. Median day of event was post-VAD implant day 35 for inflammation/infection, 37 for chylothorax, and 14 for steroids. Of note, no bleeding or thromboembolic events occurred during any of the 15 day data collection time periods for each event.
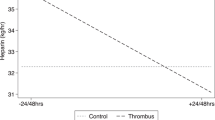
For infection/inflammation events, dTT slightly increased for the 5 days before the documented event (slope of 1.23 s/day; 95% CI ± 0.46) then stabilized after inflammation (slope of −0.001 s/day; 95% CI ± 0.21), and the two slopes differed significantly (p = 0.031). In contrast, there was no difference in aPTT slopes before compared to after inflammation (p = 0.112). There was no difference in the aPTT versus dTT before-inflammation or after-inflammation slopes (Fig. 1a). Correlation between dTT and aPTT before inflammation was greater (r = 0.76) than after inflammation (r = 0.49; Fig. 1b).
a demonstrates the change in aPTT and dTT values over time (described as slope, with 95% confidence intervals) before and after inflammation. There was no difference between the slopes of aPTT and dTT before compared to after inflammation. When assessed separately, aPTT slope was no different before and after inflammation, while dTT slope was significantly higher before (1.23 ± 0.46 s/day) than after inflammation (−0.00 ± 0.17, p < 0.0307). b demonstrates that correlation between aPTT and dTT before inflammation (r = 0.7647) was significantly higher than after inflammation (r = 0.4944)
a demonstrates the change in aPTT and dTT values over time (described as slope, with 95% confidence intervals) before and after steroids administration. There was no difference between the slopes of aPTT and dTT before compared to after steroids. When assessed separately, aPTT slope was significantly higher before (−0.55 ± 0.73 s/day) than after steroids (0.63 ± 0.37 s/day, p = 0.0285) while dTT slope was no different before and after infection. b demonstrates that correlation between aPTT and dTT before steroids (r = 0.7233) was significantly higher than after infection (r = 0.3350)
For steroids, there was no difference between the slope of dTT before compared to after steroid administration (p = 0.193). APTT decreased before (−1.55 s/day; 95% CI ± 0.37) then increased after steroid administration (0.63 s/day; 95% CI ± 0.37), and the two slopes differed significantly (p = 0.026). There was no difference in the aPTT and dTT before-steroids or after-steroids slopes (Fig. 2a). Correlation between dTT and aPTT before was greater (r = 0.72) than after steroid administration (r = 0.34; Fig. 2b).
For chylothorax, dTT increased before (2.25 s/day; 95% CI ± 0.32) then decreased after chylothorax diagnosis (−0.92 s/day; 95% CI ± 0.21), and the two slopes differed significantly (p < 0.001). APTT increased before (0.41 s/day; 95% CI ± 0.64) then decreased after chylothorax diagnosis (−0.20 s/day; 95% CI ± 0.32), and the two slopes differed significantly (p = 0.003). There was no difference in the aPTT versus dTT before-chylothorax or after-chylothorax slopes (Fig. 3a). Correlation between dTT and aPTT was no different before (r = 0.48) and after chylothorax diagnosis (r = 0.51; Fig. 3b).
a demonstrates the change in aPTT and dTT values over time (described as slope, with 95% confidence intervals) before and after chylothorax. There was no difference between the slopes of aPTT and dTT before compared to after chylothorax. When assessed separately, aPTT and dTT slopes were both significantly higher before than after chylothorax (aPTT slope before: 2.41 ± 0.64 s/day, after: −0.20 ± 0.32, p = 0.0034; dTT slope before: 2.25 ± 0.41, after: −0.92 ± 0.21, p < 0.0001). b demonstrates that there was no difference in correlation between aPTT and dTT before and after chylothorax
Discussion
Inflammation/infection and steroids can impact anticoagulation monitoring in children supported with a ventricular assist device. In our cohort of children less than 3 years on VAD support, we found that correlation between aPTT and dTT before inflammation/infection decreased after these events. Prior to the inflammatory event, dTT levels increased while aPTT remained unchanged, thus resulting in worse correlation after inflammation. This may be secondary to infection or VAD-associated inflammation that results in fibrinogen levels either decreasing (consumption or decreased production) or increasing (acute phase reactant). Activation of the contact pathway factors XI and XII may shorten the aPTT. We also found that steroid administration impacts aPTT greater than dTT with resultant decreased correlation between the two labs after steroids. Thus, the administration of steroids might be beneficial in management and stability of anticoagulation in this population, particularly when monitoring with aPTT. Chylothorax diagnosis was preceded by an increase in both dTT and aPTT, which correlated similarly before and after the event, likely due to known loss of coagulation factors in chylous fluid affecting both laboratory tests.
Inflammation/infection events occurred most frequently and had the most evident effect on correlation between dTT and aPTT. Correlation between the two lab values was reduced by one-third following inflammation/infection events in the setting of increasing dTT levels leading up to the event with subsequent normalization, but no apparent effect on aPTT. DTT likely increased prior to the event due to coagulation abnormalities that often occur during systemic inflammation, then normalized after the event due to interventions to reduce inflammation, including antibiotics or steroids. This accurately reflects expected coagulation cascade alterations that occur with inflammation and subsequently resolve with intervention [15]. APTT may not have demonstrated any change due to a balance of inflammation-associated consumptive coagulopathy, which can decrease aPTT, and elevated von Willebrand factor and factor VIII, which acutely increase during systemic inflammation and thus increase aPTT.
Similarly, correlation between dTT and aPTT was reduced by half following steroid administration. Steroids are typically used for VAD-associated inflammation following elevation in inflammatory markers, particularly CRP. Steroid administration resulted in altered aPTT levels without apparent effects on dTT, which is likely secondary to aPTT being more affected by pro-inflammatory factors than dTT. Given that steroids reduce inflammation, aPTT may increase as these pro-inflammatory factors decrease, thus worsening correlation with dTT. Importantly, steroids tend to decrease several procoagulant factors and have been reported to induce fibrinolysis, but prior studies also suggest that steroids may impair fibrinolytic activity [18]. Thus, steroids should have limited effect on anticoagulation levels, which is more accurately reflected by dTT than aPTT in this study.
Chylothorax is a known complication of pediatric cardiothoracic surgery and particularly frequent in neonates and infants [19, 20]. Loss of factors associated with chylothorax (including antithrombin III, prothrombin, and fibrinogen) leads to unpredictable anticoagulation and difficulty achieving therapeutic goals [21, 22]. In addition, chylothorax secondary to systemic venous thrombosis may have resultant coagulation abnormalities due to a consumptive coagulopathy, although incidence of venous thrombosis was not investigated in this study and has not been reported in the VAD population. Although both aPTT and dTT increased prior to chylothorax diagnosis, dTT had a greater increase compared to aPTT, despite its lab value normal range being much lower than that of aPTT. Following chylothorax with presumed clinical management (which frequently includes low-fat diet with factor repletion), both labs normalized.
There were several limitations in this study, including that of a retrospective cohort design, which does not allow causal inference and carries an intrinsic risk of confounding. Only 10 patients were included given the clinical constraints placed as study inclusion criteria in order to demonstrate similar baseline coagulation profiles by age and similar device types, and all patients were from one center. Changes in bivalirudin dosing and administration of blood products or immunoglobulins were not accounted for when considering changes in lab values, which could be evaluated on future study. In addition, dTT and aPTT have different normal lab value ranges and there is no standardization of the two labs’ values. Lastly, our institution does not use hepzyme PTT as some others do, which can be used to eliminate the effects of heparin on aPTT levels, and thus this anticoagulation lab monitor could not be evaluated by this study, potentially limiting generalizability. However, we hope this study reflects the utility and interpretation of the lab tests we did include in specific clinical scenarios in young children on VADs.
Conclusion
In children on VAD support and bivalirudin anticoagulation, inflammation/infection is a common occurrence with known coagulation factor effects, reflected in our study of both dTT and aPTT monitoring. Inflammation/infection events were preceded by uptrending dTT likely due to coagulation abnormalities following systemic inflammation that subsequently normalized following intervention. APTT remained unchanged prior to and following these events from balanced pro- and anti-coagulant effects on aPTT during inflammation that both resolve with intervention. Steroid administration mirrored this worsening correlation following the event, with steroids having a greater impact on aPTT stabilization due to their ability to decrease the inflammatory effects on aPTT accuracy of bivalirudin anticoagulation effect. Chylothorax results in loss of coagulation factors leading prolongation of both aPTT and dTT, resulting in unpredictable monitoring. Further study to evaluate the impact of inflammation, infection, and chylothorax on lab monitoring in this population is warranted.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- VAD:
-
Ventricular assist device
- aPTT:
-
Activated partial thromboplastin time
- DTT:
-
Dilute thrombin time
References
Schweiger M, Hubler M, Albisetti M. Heparin anticoagulation monitoring in patients supported by ventricular assist devices. ASAIO J. 2015;61:487–8.
Huang JY, Monagle P, Massicotte MP, VanderPluym CJ. Antithrombotic therapies in children on durable ventricular assist devices: a literature review. Thromb Res. 2018;172:194–203.
Sylvia LM, Ordway L, Pham DT, DeNofrio D, Kiernan M. Bivalirudin for treatment of LVAD thrombosis: a case series. ASAIO J. 2014;60:744–7.
Burstein D, Kimmel S, Putt M, Rossano J, VanderPluym C. Cost-effectiveness of bivalirudin in pediatric ventricular assist devices. J Heart Lung Transplant. 2022. https://doi.org/10.1016/j.healun.2022.10.006.
Rimsans J, Sylvester KW, Connors JM. Direct thrombin inhibitor for LVAD thrombosis: a closer look. Clin Appl Thromb Hemost. 2017;23:405–9.
Ryerson LM, Balutis KR, Granoski DA, Nelson LR, Massicotte MP, Lequier LL, et al. Prospective exploratory experience with bivalirudin anticoagulation in pediatric extracorporeal membrane oxygenation. Pediatr Crit Care Med. 2020;21:975–85.
Wong TE, Huang YS, Weiser J, Brogan TV, Shah SS. Antithrombin concentrate use in children: a multicenter cohort study. J Pediatr. 2013;163:1329-1334.e1.
Bates A, Buchholz H, Freed D, MacArthur R, Pi DT, Conway J. Bivalirudin experience in a heterogeneous ventricular assist device population. ASAIO J. 2020;66:677–82.
VanderPluym CJ, Cantor RS, Machado D, Boyle G, May L, Griffiths E, et al. Utilization and outcomes of children treated with direct thrombin inhibitors on paracorporeal ventricular assist device support. ASAIO J. 2020;66:939–45.
Puri K, Tunuguntla HP, Hensch LA, Loh J, Hui SK, Razavi A, et al. Bivalirudin or unfractionated heparin for anticoagulation in pediatric patients on continuous flow ventricular assist device support: single-center retrospective cohort study. Pediatr Crit Care Med. 2022;23:e465–75.
Zaleski KL, DiNardo JA, Nasr VG. Bivalirudin for pediatric procedural anticoagulation: a narrative review. Anesth Analg. 2019;128:43–55.
Teruya J, Hensch L, Bruzdoski K, Adachi I, Hui SR. Monitoring bivalirudin therapy in children on extracorporeal circulatory support devices: thromboelastometry versus routine coagulation testing. Thromb Res. 2020;186:54–7.
Molinaro RJ, Szlam F, Levy JH, Fantz CR, Tanaka KA. Low plasma fibrinogen levels with the clauss method during anticoagulation with bivalirudin. Anesthesiology. 2008;109:160–1.
Rabinowitz EJ, Ouyang A, Armstrong DR, Wallendorf M. Poor reliability of common measures of anticoagulation in pediatric extracorporeal membrane oxygenation. ASAIO J. 2021;68:850–8.
Engel ELM, Martin J, Palumbo J, Lorts A, Geer R, Luchtman-Jones L. Use of bivalirudin-specific monitoring assays in ventricular assist device patients. Blood. 2021;138:3236.
Teruya J, Bruzdoski K, Hensch L, Hui SR, Kostousov V. How to best monitor bivalirudin anticoagulant effect for ECMO and VAD-comparison of four assay methods. Int J Lab Hematol. 2022;44:589–94.
Adatya S, Uriel N, Yarmohammadi H, Holley CT, Feng A, Roy SS, et al. Anti-factor Xa and activated partial thromboplastin time measurements for heparin monitoring in mechanical circulatory support. JACC Heart Fail. 2015;3:314–22.
van Zaane B, Nur E, Squizzato A, Gerdes VE, Buller HR, Dekkers OM, et al. Systematic review on the effect of glucocorticoid use on procoagulant, anti-coagulant and fibrinolytic factors. J Thromb Haemost. 2010;8:2483–93.
Perry T, Bora K, Bakar A, Meyer DB, Sweberg T. Non-surgical risk factors for the development of chylothorax in children after cardiac surgery—does fluid matter? Pediatr Cardiol. 2020;41:194–200.
Buckley JR, Graham EM, Gaies M, Alten JA, Cooper DS. Clinical epidemiology and centre variation in chylothorax rates after cardiac surgery in children a report from the pediatric cardiac critical care consortium. Cardiol Young. 2017. https://doi.org/10.1017/S104795111700097X.
Bernet-Buettiker V, Waldvogel K, Cannizzaro V, Albisetti M. Antithrombin activity in children with chylothorax. Eur J Cardiothorac Surg. 2006;29:406–9.
Zuluaga MT. Chylothorax after surgery for congenital heart disease. Curr Opin Pediatr. 2012;24:291–4.
Acknowledgements
This work was conducted with support from the Heart Institute Research Core (HIRC) at Cincinnati Children’s Hospital.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by KB, AL, ZG, and TP. The first draft of the manuscript was written by KB and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
Angela Lorts is a consultant for Abbott, SynCardia, Medtronic, Abiomed and Berlin Heart Inc.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Brandewie, K., Lorts, A., Luchtman-Jones, L. et al. Impact of inflammation and steroids on anti-coagulation in children supported on a ventricular assist device. J Artif Organs (2024). https://doi.org/10.1007/s10047-024-01442-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10047-024-01442-2