Abstract
The NKX2-5 gene is a vital regulator of cardiac formation and development. Recently, the roles of NKX2-5 63A>G polymorphism and 606G>C polymorphism in congenital heart disease (CHD) have been extensively studied, with conflicting results. The aim of the present study was to better elucidate the associations between NKX2-5 genetic polymorphisms and CHD risk through a meta-analysis. Eligible articles were searched in PubMed, MEDLINE, EMBASE, Google Scholar and CNKI up to December 2015. Odds ratios (ORs) and 95 % confidence intervals were used to detect any potential associations between NKX2-5 genetic polymorphisms and CHD risk. Heterogeneity between studies was assessed with Q test and I 2 statistic. Subgroup analysis and sensitivity analysis were performed to test the reliability and stability of the results, and funnel plots were applied to estimate publication bias. A total of 13 case–control studies including 2245 CHD patients and 1953 healthy controls were analyzed. The overall meta-analysis results showed that NKX2-5 63A>G polymorphism and 606G>C polymorphism were not significantly associated with CHD risk. Subgroup analysis was further performed for NKX2-5 63A>G polymorphism based on types of CHD and ethnicity of study population, and similar negative results were found in all subgroups. Our findings suggested that NKX2-5 63A>G polymorphism and 606G>C polymorphism may not be implicated in the pathogenesis of CHD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Congenital heart disease (CHD), characterized by structural and/or functional anomaly of heart or intrathoracic great vessels due to abnormal cardiac development, is the most prevalent type of birth defect, with an estimated incidence of 4–50 in every 1000 live births, and is the leading non-infectious cause of infant death worldwide [1]. Despite rapid improvement in surgical treatment and interventional therapy over the past few decades, the morbidity and mortality of CHD patients remained significantly higher than that of the general population, and its associated complications such as heart failure, arrhythmia or sudden cardiac death may occur even after effective correction of cardiac abnormalities [2, 3].
To date, the exact cause of CHD is still unclear; however, there is growing evidence to support that genetic factors play a crucial part in its pathogenesis. Firstly, family clustering of CHD with variable phenotypes has been observed extensively, and a higher risk of developing cardiac malformations exists in offspring of CHD patients [4, 5]. Secondly, it was reported that 8–13 % of CHD patients have chromosome abnormalities [6], and mutations of several genes have been found to be associated with CHD [7–11]. Nevertheless, the etiology of CHD is highly complex and the genetic determinants underlying CHD are not fully elucidated.
The NKX2-5 gene, a highly conserved cardiac-specific transcription factor encoder located on chromosome 5q34, is a vital regulator of cardiac formation and development [12]. Previous studies have shown that knockout of NKX2-5 gene in mice could lead to embryonic or premature death, with arrested heart development and various kinds of cardiac defects [13, 14]. Besides, over 40 missense and nonsense mutations of NKX2-5 gene have been identified in CHD patients [15, 16], and abnormal expression levels of NKX2-5 were also found to be associated with multiple cardiac malformations [17, 18]. Therefore, NKX2-5 is thought to be an ideal candidate gene for CHD susceptibility.
Recently, numerous studies have been done to investigate the roles of NKX2-5 genetic polymorphisms, particularly the exon 1 63A>G polymorphism (rs2277923) and the exon 2 606G>C (rs3729753) polymorphism in the pathogenesis of CHD. But results were controversial, and statistical power of individual studies was insufficient [19–31]. Therefore, we conducted the present meta-analysis to better assess the associations between NKX2-5 genetic polymorphisms and the risk of CHD.
Materials and Methods
Literature Search Strategy
Electronic databases of PubMed, MEDLINE, EMBASE, Google Scholar and China National Knowledge Infrastructure (CNKI) were searched without time limit using the following keywords: “congenital heart disease,” “congenital heart defect,” “congenital cardiovascular malformation,” “NKX2-5,” “NKX2.5,” “NK2 homeobox 5,” “NK2 transcription factor-related, locus 5,” “cardiac-specific homeobox,” “CSX,” “polymorphism,” “variant,” “genotype” and “allele.” The initial search was conducted in May 2015, and the latest update was performed in December 2015. Besides, the reference lists of all relevant articles were reviewed manually for further identification of potentially eligible articles.
Inclusion Criteria
The inclusion criteria for the present study were set prior to the literature search. Eligible studies met the following conditions: (1) article already published electronically; (2) case–control study of unrelated CHD patients and healthy controls; (3) evaluation of the association between NKX2-5 63A>G polymorphism (rs2277923) and/or 606G>C polymorphism (rs3729753) and the risk of CHD; (4) presentation of sufficient data to calculate the odds ratios (ORs) and corresponding 95 % confidence intervals (CIs); and (5) full text in English or Chinese available. If the report was duplicated or identical patients were enrolled in two studies, only the most recent and complete article was included. Pedigree studies, case reports, case series, reviews, editorials, expert opinions and studies with CHD being considered as a component of any known genetic disorders were intentionally excluded.
Data Extraction and Quality Assessment
From each included studies, the following data were extracted: first author, year of publication, country of origin, ethnicity of study population, the number of cases and controls, types of CHD, allelic and genotypic frequency of NKX2-5 63A>G polymorphism and/or 606G>C polymorphism in CHD patients and control subjects, and whether the distributions of NKX2-5 genetic polymorphisms in the control group were in accordance with Hardy–Weinberg equilibrium (HWE). The Newcastle–Ottawa quality assessment scale (NOS), a classical rating tool which evaluates the quality of non-randomized studies from three perspectives: selection, comparability and exposure, was used to assess the validity of all case–control studies included [32]. This rating system has a score range of 0–9, and studies with a score of more than 7 were assumed to be of high quality. Two reviewers (XCX and XHS) performed the data extraction and quality assessment independently. When necessary, the reviewers wrote to the authors for extra information or raw data. Any discrepancies between two reviewers were resolved by discussion until reaching a consensus. The final results were reviewed by a senior reviewer (LR).
Statistical Analysis
All data analyses were performed with Review Manager version 5.3.3 (The Cochrane Collaboration, Software Update, Oxford, United Kingdom). HWE was explored by using the Chi-square test. ORs and corresponding 95 % CIs were used to evaluate associations of NKX2-5 63A>G polymorphism and 606G>C polymorphism with CHD risk. In addition, Q test and I 2 statistic were employed to evaluate heterogeneity between studies. If probability value (P value) was less than 0.1 or I 2 was greater than 50 %, between-study heterogeneity was considered to be significant, and the random-effect model (REM) would be adopted for analyses. Otherwise, if studies were considered to be homogenous, the fixed-effect model (FEM) would be applied for analyses. Subgroup analysis was performed based on types of CHD and ethnicity of study population if a subgroup contained at least four individual studies. Sensitivity analysis was carried out through removing one individual study each time. Publication bias was further assessed with funnel plots. And a P value of 0.05 or less was regarded as statistically significant in comparison between CHD patients and healthy controls.
Results
Included Studies
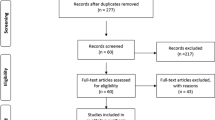
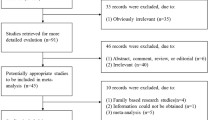
The literature search generated 243 results. After exclusion of irrelevant or duplicate articles by reading titles and abstracts, 74 articles were selected for further evaluation. Among these, a total of 13 case–control studies including 2245 CHD patients and 1953 healthy controls met our inclusion criteria [19–31] (see Fig. 1), 13/13 were about the NKX2-5 63A>G polymorphism, and 6/13 were about the NKX2-5 606G>C polymorphism. All included studies were published between 2005 and 2015. Of these, there were 11 studies of Asian ethnicity and 2 studies of Caucasian ethnicity. HWE test for the control group of each included studies revealed that 10 studies were in agreement with HWE, whether the remaining 3 studies by Ouyang et al. [25], Peng et al. [27] and Xiong et al. [29] met HWE were unavailable since only allelic frequencies were provided. Eight articles were published in English, and the other five were published in Chinese. Characteristics of included studies are summarized in Table 1, and distributions of NKX2-5 63A>G polymorphism and 606G>C polymorphism are summarized in Table 2 and Table 3.
Risk of Bias in Included Studies
As shown in Table 1, the average NOS score of included studies was 7.31 (range from 7 to 8), which implied that all eligible articles were of relatively high quality. The improper selection of controls and mismatching age of CHD cases and control subjects were the major sources of biases.
NKX2-5 63A>G Polymorphism and CHD Risk
A total of 13 studies with 2230 CHD cases and 1940 control subjects were enrolled for NKX2-5 63A>G polymorphism [19–31]. Since Ouyang et al. [25], Peng et al. [27] and Xiong et al. [29] failed to report genotypic frequency of NKX2-5 63A>G polymorphism in CHD patients and healthy controls, we accessed the association between NKX2-5 63A>G polymorphism and CHD risk by comparing distribution of alleles in CHD cases and control subjects. REM was employed for analysis on account of striking between-study heterogeneity (I 2 = 81 %, P for the heterogeneity <0.00001), and no significant association with CHD risk was found for NKX2-5 63A>G polymorphism (OR 1.10, 95 % CI 0.88–1.38, P = 0.39) (see Fig. 2).
NKX2-5 606G>C Polymorphism and CHD Risk
For NKX2-5 606G>C polymorphism, a total of 6 studies including 1330 CHD patients and 1167 healthy controls were investigated [19, 24, 27, 29–31]. In order to explore the association between NKX2-5 606G>C polymorphism and CHD risk, we compared allelic frequency in CHD cases and control subjects because Peng et al. [27] and Xiong et al. [29] did not present distribution of genotypes in CHD patients and healthy controls. Heterogeneity between studies was found to be trivial (I 2 = 0 %, P for the heterogeneity = 0.59), and thus, analysis was performed with FEM. No significant association was detected between NKX2-5 606G>C polymorphism and CHD risk (OR 1.11, 95 % CI 0.78–1.58, P = 0.57) (see Fig. 3).
Subgroup Analysis
For NKX2-5 63A>G polymorphism and CHD risk, subgroup analysis was performed by stratifying available data based on types of CHD and ethnicity of study population. In the ventricular septal defect (VSD) and atrial septal defect (ASD) subgroups, we failed to detect any significant association for NKX2-5 63A>G polymorphism (VSD, OR 1.12, 95 % CI 0.83–1.51, P = 0.47, I 2 = 77 %, P for the heterogeneity = 0.0002; ASD, OR 0.79, 95 % CI 0.53–1.19, P = 0.26, I 2 = 74 %, P for the heterogeneity = 0.002) (see Table 4). In addition, no significant association was found between NKX2-5 63A>G polymorphism and the risk of CHD in the Asian subgroup (OR 1.02, 95 % CI 0.84–1.23, P = 0.87, I 2 = 73 %, P for the heterogeneity <0.0001) (See Table 4). Subgroup analysis for NKX2-5 606G>C polymorphism and CHD risk could not be carried out due to lack of relevant data.
Sensitivity Analysis
Sensitivity analysis was performed by removing one individual study each time. For NKX2-5 63A>G polymorphism and 606G>C polymorphism, removing any study did not impact the overall results. However, we found that between-study heterogeneity for NKX2-5 63A>G polymorphism was drastically reduced (I 2 = 44 %, P for the heterogeneity = 0.06) after eliminating studies by Shi et al. [28] and Ketharnathan et al. [22], which suggested that these two studies were the main source of heterogeneity.
Publication Bias
Potential publication bias was evaluated with funnel plots. Visual inspection of funnel plots revealed no apparent asymmetry for NKX2-5 63A>G polymorphism and 606G>C polymorphism. And these results suggested that significant publication bias was unlikely.
Discussion
CHD contains a variety of structural cardiovascular malformations that are actually or potentially of functional significance [33]. Historically, few CHD patients reached adulthood, but owing to the tremendous advances in interventional therapies and surgical treatment, the average life expectancy of CHD patients has been significantly prolonged in the last two decades [34]. However, despite substantially improved prognosis, CHD remains to be the leading cause of mortality for infants worldwide.
To date, the etiology of CHD is still largely unknown in spite of extensive research. However, it has become evident recently that several genes are implicated in the pathogenesis of CHD [5]. Of these, the NKX2-5 gene, which encodes a homeodomain and NK2-specific domain containing cardiac transcription factor of 324 amino acids, is a crucial regulator of cardiac formation and development [12, 26]. It is the earliest expressed transcription factor encoder during embryonic cardiac development and plays a vital role in regulating expression of genes essential for heart formation. Previous animal studies have demonstrated that disruption of NKX2-5 gene would impact specification of cardiac progenitor cells, morphogenesis of heart, differentiation of cardiomyocytes as well as formation and development of cardiac conduction system [13, 35–37]. In addition, more than 40 mutations of NKX2-5 gene have been found in both familiar and sporadic CHD cases, and altered transcription activity of NKX2-5 was also shown to cause cardiac abnormalities [15, 16].
Recently, multiple studies have tried to explore the associations between certain NKX2-5 genetic polymorphisms and the risk of CHD. Among these, the 63A>G polymorphism and 606G>C polymorphism were the two most intensively investigated sites. These two single-nucleotide polymorphisms are both synonymous variants. Although synonymous polymorphisms do not change the amino acid sequence of encoded proteins, accumulating evidence suggested that they may affect mRNA structure and stability, translation rate and fidelity as well as protein folding [38]. The 63A>G polymorphism (Glu21Glu) is located at exon 1 of NKX2-5 gene. It was firstly reported by Benson et al. [39] in 1999. Afterward, several studies found that this polymorphism was significantly associated with CHD risk in different populations [22, 25, 28]. Moreover, luciferase reporter assays by Ouyang et al. [25] revealed that the A to G substitution of 63A>G polymorphism significantly reduced transcriptional activity of NKX2-5 gene by 20 %, which may account for its association with the occurrence and development of CHD. The 606G>C polymorphism (Leu202Leu), which located at exon 2 of NKX2-5 gene, was also thought to be implicated in the pathogenesis of CHD. However, no functional analysis has been reported about this polymorphism yet.
Despite potential theoretical mechanisms, results regarding associations of NKX2-5 genetic polymorphisms with CHD risk were still contradicted. Hence, we conducted the present meta-analysis to solve the conflict and obtain a more conclusive result. And our overall results suggested that NKX2-5 63A>G polymorphism and 606G>C polymorphism may not be associated with CHD risk. Significant between-study heterogeneity for NKX2-5 63A>G polymorphism was found, and thus, we carried out stratified analyses by categorizing included studies into different subgroups on the basis of types of CHD and ethnicity of study population. Heterogeneity between studies remained notable in each subgroup, and similar to the result of overall meta-analysis, no significant association with CHD risk was detected for NKX2-5 63A>G polymorphism in any subgroups. Sensitivity analysis was further performed to test the stability of results and trace the source of between-study heterogeneity; for two NKX2-5 genetic polymorphisms, removing any study did not change the overall results. However, we found that when studies by Shi et al. and Ketharnathan et al. were omitted, between-study heterogeneity for NKX2-5 63A>G polymorphism was drastically reduced, suggesting that these two studies were the major sources of heterogeneity.
It is worth noting that Wang et al. [40] performed a meta-analysis for associations between NKX2-5 genetic polymorphisms and CHD risk of Chinese population in 2013. Compared with the present study, similar results were found for NKX2-5 606G>C polymorphism in the previous study, but results on NKX2-5 63A>G polymorphism were conflicting. Considering that our findings on NKX2-5 63A>G polymorphism were based on more eligible studies of relatively high quality and the sample size of the present analysis was significantly larger than that of the previous study (2230 cases and 1940 controls vs. 1243 cases and 1139 controls), maybe the results of the current study were more convincing. Overall, results from previous and current meta-analyses support that NKX2-5 606G>C polymorphism may not be involved in the pathogenesis of CHD; however, for NKX2-5 63A>G polymorphism and the risk of CHD, further studies are warranted to draw a more credible conclusion.
This study is certainly not without limitations. Firstly, the number of studies investigating the relationship between NKX2-5 polymorphisms and CHD risk is still limited, and sample size of several included studies was obviously not sufficient, making our results not convincing enough. Secondly, although funnel plots revealed no apparent publication bias, we cannot eliminate the possibility of publication bias since only published studies were included. Thirdly, all included studies were published in English or Chinese; therefore, maybe some qualified articles in other languages were missed. Fourthly, genetic associations of certain NKX2-5 polymorphisms with CHD may also be influenced by gene–gene and gene–environmental interactions. It is possible that one certain polymorphism may be associated with CHD risk, but due to interactions with multiple genes and environmental factors, the association would no longer be observed. Taken these limitations into consideration, the results presented by the current study should be interpreted with caution.
Conclusions
In conclusion, the current meta-analysis suggested that NKX2-5 63A>G polymorphism and 606G>C polymorphism may not be implicated in the pathogenesis of CHD. However, considering that the present results were based on limited number of case–control studies, further multicenter studies with larger sample size from different populations are warranted to confirm our results. Besides, given that cardiac transcription factors play a pivotal role in heart formation, future investigations are needed to explore the potential roles of other polymorphisms of cardiac transcriptional factor genes in the occurrence and development of CHD.
References
Hoffman JI, Kaplan S (2002) The incidence of congenital heart disease. J Am Coll Cardiol 39:1890–1900
Van der Bom T, Zomer AC, Zwinderman AH et al (2011) The changing epidemiology of congenital heart disease. Nat Rev Cardiol 8:50–60
Verheugt CL, Uiterwaal CS, van der Velde ET et al (2010) Mortality in adult congenital heart disease. Eur Heart J 31:1220–1229
Samanek M (2000) Congenital heart malformations: prevalence, severity, survival, and quality of life. Cardiol Young 10:179–185
Pierpont ME, Basson CT, Benson DW Jr et al (2007) Genetic basis for congenital heart defects: current knowledge: a scientific statement from the American Heart Association Congenital Cardiac Defects Committee, Council on Cardiovascular Disease in the Young: endorsed by the American Academy of Pediatrics. Circulation 115:3015–3038
Ferencz C, Neill CA, Boughman JA et al (1989) Congenital cardiovascular malformations associated with chromosome abnormalities: an epidemiologic study. J Pediatr 114:79–86
Garg V, Muth AN, Ransom JF et al (2005) Mutations in NOTCH1 cause aortic valve disease. Nature 437:270–274
Muncke N, Jung C, Rudiger H et al (2003) Missense mutations and gene interruption in PROSIT240, a novel TRAP240-like gene, in patients with congenital heart defect (transposition of the great arteries). Circulation 108:2843–2850
Robinson SW, Morris CD, Goldmuntz E et al (2003) Missense mutations in CRELD1 are associated with cardiac atrioventricular septal defects. Am J Hum Genet 72:1047–1052
Garg V, Kathiriya IS, Barnes R et al (2003) GATA4 mutations cause human congenital heart defects and reveal an interaction with TBX5. Nature 424:443–447
Basson CT, Bachinsky DR, Lin RC et al (1997) Mutations in human TBX5 cause limb and cardiac malformation in Holt–Oram syndrome. Nat Genet 15:30–35
Zhang SS, Kim KH, Rosen A et al (2011) Iroquois homeobox gene 3 establishes fast conduction in the cardiac His–Purkinje network. Proc Natl Acad Sci USA 108:13576–13581
Akazawa H, Komuro I (2005) Cardiac transcription factor Csx/Nkx2-5: Its role in cardiac development and diseases. Pharmacol Ther 107:252–268
Terada R, Warren S, Lu JT et al (2011) Ablation of Nkx2-5 at mid-embryonic stage results in premature lethality and cardiac malformation. Cardiovasc Res 91:289–299
Reamon-Buettner SM, Borlak J (2010) NKX2-5: an update on this hypermutable homeodomain protein and its role in human congenital heart disease (CHD). Hum Mutat 31:1185–1194
Stallmeyer B, Fenge H, Nowak-Gottl U, Schulze-Bahr E (2010) Mutational spectrum in the cardiac transcription factor gene NKX2.5 (CSX) associated with congenital heart disease. Clin Genet 78:533–540
Kasahara H, Ueyama T, Wakimoto H et al (2003) Nkx2.5 homeoprotein regulates expression of gap junction protein connexin 43 and sarcomere organization in postnatal cardiomyocytes. J Mol Cell Cardiol 35:243–256
Benson D (2010) Genetic origins of pediatric heart disease. Pediatr Cardiol 31:422–429
Cao Y, Wang J, Wei C (2016) Genetic variations of NKX2-5 in sporadic atrial septal defect and ventricular septal defect in Chinese Yunnan population. Gene 575:29–33
Dinesh SM, Kusuma L, Smitha R et al (2010) Single nucleotide polymorphisms of NKX2.5 found in congenital heart disease patients of Mysore, South India. Genet Test Mol Biomarkers 14:873–879
Han Z, Tang Y, Chen Y, Hu D (2011) Mutation screening of NKX2.5 gene and its relationship to simple congenital heart disease in 81 patients. Chin Circ J 26:461–464
Ketharnathan S, Koshy T, Sethuratnam R, Paul S, Venkatesan V (2015) Investigation of NKX2.5 gene mutations in congenital heart defects in an Indian population. Genet Test Mol Biomarkers 19:579–583
Liu XY, Yang YQ, Yang Y, Lin XP, Chen YH (2009) Mutation of NKX2-5 gene in patients with atrial septal defect. Zhonghua Er Ke Za Zhi 47:696–700
Liu XY, Yang YQ, Yang Y, Lin XP, Chen YH (2009) Novel NKX2-5 mutations identified in patients with congenital ventricular septal defects. Zhonghua Yi Xue Za Zhi 89:2395–2399
Ouyang P, Saarel E, Bai Y et al (2011) A de novo mutation in NKX2.5 associated with atrial septal defects, ventricular noncompaction, syncope and sudden death. Clin Chim Acta 412:170–175
Pang S, Shan J, Qiao Y et al (2012) Genetic and functional analysis of the NKX2.5 gene promoter in patients with ventricular septal defects. Pediatr Cardiol 33:1355–1361
Peng T, Wang L, Zhou SF, Li X (2010) Mutations of the GATA4 and NKX2.5 genes in Chinese pediatric patients with non-familial congenital heart disease. Genetica 138:1231–1240
Shi L, Shen AD, Li XF, Bai S, Guan XL, Li ZZ (2005) Mutation screening of Nkx2.5 gene and associated study in Exon1 in Chinese with congenital heart disease. J Capital Univ Med Sci 26:525–528
Xiong F, Li Q, Zhang C, Chen Y et al (2012) Analyses of GATA4, NKX2.5, and TFAP2B genes in subjects from southern China with sporadic congenital heart disease. Cardiovasc Pathol 22:141–145
Zhang W, Li X, Shen A et al (2009) Screening NKX2.5 mutation in a sample of 230 Han Chinese children with congenital heart diseases. Genet Test Mol Biomarkers 13:159–162
Zhao X (2014) Mutation screening of NKX2.5 gene and associated study with simple congenital heart disease. Dissertation, University of Science and Technology
Zhang R, Wang J, Yang R et al (2014) Effects of Pro12Ala polymorphism in peroxisome proliferator-activated receptor-γ2 gene on metabolic syndrome risk: a meta-analysis. Gene 535:79–87
Mitchell SC, Korones SB, Berendes HW (1971) Congenital heart disease in 56,109 births incidence and natural history. Circulation 43:323–332
Warnes CA (2005) The adult with congenital heart disease: born to be bad? J Am Coll Cardiol 46:1–8
Hiroi Y, Kudoh S, Monzen K et al (2001) Tbx5 associates with Nk2-5 and synergistically promotes cardiomyocyte differentiation. Nat Genet 28:276–280
Jay PY, Harris BS, Maguire CT et al (2004) Nk2-5 mutation causes anatomic hypoplasia of the cardiac conduction system. J Clin Invest 113:1130–1137
Pashmforoush M, Lu JT, Chen H et al (2004) Nk2-5 pathways and congenital heart disease; loss of ventricular myocyte lineage specification leads to progressive cardiomyopathy and complete heart block. Cell 117:373–386
Sauna ZE, Kimchi-Sarfaty C (2011) Understanding the contribution of synonymous mutations to human disease. Nat Rev Genet 12:683–691
Benson DW, Silberbach GM, Kavanaugh-McHugh A et al (1999) Mutations in the cardiac transcription factor NKX2.5 affect diverse cardiac developmental pathways. J Clin Invest 104:1567–1573
Wang Z, Zou L, Zhong R et al (2013) Associations between two genetic variants in NKX2-5 and risk of congenital heart disease in Chinese population: a meta-analysis. PLoS ONE 8:e70979
Acknowledgments
This work was supported by grants from the National Natural Science Fund of China (81270289, 81300169).
Authors' contribution
X.C.X. and L.R. conceived of the study and participated in its design. X.C.X. and X.H.S. conducted the systematic literature review. X.S.X. performed data analysis. X.C.X. and L.R. drafted the manuscript. All authors have read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest regarding the content herein.
Rights and permissions
About this article
Cite this article
Xie, X., Shi, X., Xun, X. et al. Associations of NKX2-5 Genetic Polymorphisms with the Risk of Congenital Heart Disease: A Meta-analysis. Pediatr Cardiol 37, 953–961 (2016). https://doi.org/10.1007/s00246-016-1377-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-016-1377-8