Abstract
Pulmonary vein stenosis (PVS) carries significant morbidity and mortality for affected children, and its management often requires multiple angioplasty procedures. PVS angioplasty can be complicated by systemic embolic events such as stroke, but incidence and risk factors are poorly understood. We reviewed pediatric catheterizations involving PVS angioplasty and/or stent placement performed at Boston Children’s Hospital between July 2005 and February 2014. A total of 406 cases were performed in 144 distinct patients. Patients underwent a median of two catheterizations, at median age 1 year and weight 6.9 kg. Eleven (2.7 %) catheterizations were complicated by clinically apparent systemic embolic events, comprising 10 strokes (one with associated hepatic embolism) and 1 renal infarct. Prevalence of clinically evident stroke among this cohort was 7.6 %. Using a prior (uncomplicated) catheterization to allow each patient to serve as their own control, we sought to identify potentially modifiable risk factors for systemic embolic events. Although this analysis was limited by low power, complicated and uncomplicated angioplasties did not appear to differ in case time, contrast dose, anticoagulation management, use of cutting balloons, number of catheter exchanges, or size of long sheath used. Significant non-embolic adverse events were common, occurring in 25 % of catheterizations. Systemic embolism appears to complicate PVS angioplasty at a rate much higher than that described for other congenital catheterizations. This risk may be inherent to the procedure rather than related to any modifiable or operator-dependent factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pediatric intraluminal pulmonary vein stenosis (PVS), although rare, imposes a high burden of morbidity and mortality on affected children [1, 9]. Our center offers a multimodality treatment approach, comprising initial diagnostic catheterization (with or without palliative angioplasty) followed by an attempt at curative surgery (typically ‘sutureless’ repair [5]). Post-operative disease recurrence is managed with angioplasty (involving both conventional and cutting balloons) with or without stent placement [6]. Experimental chemotherapy is considered in patients with aggressive disease [7]. In most patients with recurrent disease, multiple angioplasty procedures are required for ongoing palliation.
Anecdotally, therapeutic catheterization in PVS carries a significant risk of adverse events (AEs). Several recent sentinel cases involving embolic stroke following pulmonary vein dilation have highlighted this potential risk. The risk of AEs accompanying pulmonary vein dilation is poorly understood, and the rate of thromboembolism is unknown. This gap in knowledge hampers counseling of families facing a potentially lethal disease on the one hand and a potentially morbid procedure on the other.
We sought to identify the incidence of clinically relevant systemic embolism following PVS angioplasty and to identify any potentially modifiable risk factors for embolic AEs. We also sought to better characterize the demographics and burden of catheterization-related AEs in our PVS patient population.
Materials and Methods
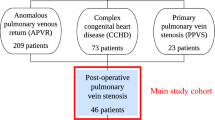
This retrospective, single-center cohort study included all cardiac catheterizations at Boston Children’s Hospital involving pulmonary vein angioplasty in children (<18 years) between July 2005 and February 2014 (dates were selected to allow use of a searchable AE database). This retrospective review was approved by our Committee for Clinical Investigation.
Catheterizations were identified through search of an electronic database. Procedure notes for PVS angioplasty catheterizations were reviewed for patient details (age, cardiac diagnosis, details of presenting catheterization, surgical management of PVS, weight, hematocrit), procedural characteristics (fluoroscopy time, dose of angiographic contrast, case time defined as access obtained to sheaths removed or sutured in place, time spent in left atrium defined as interval from first to last left atrial/PV saturation, pressure, or angiogram as assessed from the case time log), and AEs (excluding vascular access complications, need for inotropic support during the procedure, or need for intensive care admission post-procedure). To minimize the possibility of missing clinically important embolic complications, discharge summaries and (when available) follow-up clinic notes were also reviewed. We defined a periprocedural systemic embolic AE to be any of the following, confirmed by imaging (CT, MRI, ultrasound, or conventional angiography), demonstrated within 14 days of the catheterization and prior to next intracardiac procedure: embolic stroke, renal infarction, mesenteric infarction, myocardial infarction, or hepatic infarction. Events were noted—but excluded from analysis—if an additional intracardiac procedure (catheterization or surgery) intervened between PVS catheterization and presentation of the embolic AE.
To assess for possible modifiable risk factors for systemic embolic events, cases were matched with controls as follows: if the patient had undergone prior PVS angioplasty, the most recent such catheterization not complicated by systemic embolism was used as a control; otherwise, a control patient matched for age and weight was randomly selected from candidate patients. Case and control catheterizations were reviewed in further detail to assess for additional potential risk factors for embolism, namely intraprocedural activated clotting time (ACT) <200 or <250 s (at any time after initial heparin bolus administered), use of post-procedure therapeutic heparin infusion, recanalization of an atretic pulmonary vein, number of distinct veins dilated/stented, new pulmonary vein stent placement, use of cutting balloons, thrombus/air seen in long sheath, thrombus seen in pulmonary veins, largest long sheath used, estimated number of catheter exchanges (estimated by total number of catheters used in the left atrium), and junior operator (<2 years in practice).
Statistical analysis was performed using IBM SPSS Statistics version 19 (PASW, Inc., Chicago, IL). PVS case characteristics are reported as median [interquartile range (IQR), absolute range]. To assess for differences in exposures between cases and controls, McNemar’s test was used for dichotomous variables, and Wilcoxon’s signed-rank test was used for ordinal variables. Significance was set at p < 0.05, with no correction for multiple comparisons.
Results
A total of 406 pediatric PVS angioplasty catheterizations were performed during the study period. These cases involved 144 distinct patients, with each patient undergoing a median of 2 (IQR 1–4, range 1–19) catheterizations. Of this cohort, 94 (65 %) are alive at last follow-up (median follow-up interval 1.7 year). Median age at first PVS angioplasty was 0.5 year (IQR 0.3–1.4 year, range 6 days–14.7 year). Approximately 60 % of patients underwent at least one surgical procedure to treat PVS. Further details of this patient cohort are described in Table 1.
Important case features of the 406 PVS angioplasty catheterizations include the following. Median age at catheterization was 1 year (IQR 0.5–2.2 year, range 6 days–16.7 year), with median weight 6.85 kg (IQR 4.9–10.4 kg, range 2.1–98.5 kg). Median fluoroscopy time was 73 min (IQR 54–94, range 12–234 min), median contrast dose 5 mL/kg (IQR 3.6–6.7 mL/kg, range 0.3–16.5 mL/kg), median case time 141 min (IQR 111–177 min, range 32–250 min), and median time in the left atrium 82 min (IQR 57–118, range 8–300 min).
Eleven catheterizations (2.7 %) were found to be complicated by systemic embolic events, comprising 10 strokes (one with associated hepatic embolism) and 1 renal infarct. One patient suffered two events (strokes) at distinct catheterizations. Details of these 11 cases are described in Table 2. Of the 10 affected patients, 2 (20 %) are alive at last follow-up.
An additional two strokes occurred in patients who underwent pulmonary vein angioplasty and surgical vein repair in close succession; as the source/timing of these events is unclear, they were not included in our analysis.
The results of a case–control analysis are shown in Table 3. All but one of the cases had a prior catheterization suitable for use as the control. No risk factors were identified as being associated with embolic AE. There were trends toward association for largest long sheath used (p = 0.08) and number of catheters used in the left atrium (p = 0.08), but the magnitude of the differences does not suggest clinical relevance (median 7 French vs 6 French; median 16 catheters vs 14 catheters). No cases complicated by embolism involved new pulmonary vein stent placement.
Looking more broadly at PVS catheterization AEs, at least one (non-access related) AE was reported in 102 of 406 catheterizations (25 %). The most frequently reported AEs were catheter-mediated supraventricular tachycardia (23 cases), post-angioplasty pulmonary vein tear/flap/aneurysm (13 cases), significant reperfusion edema/pulmonary hemorrhage (12 cases), and transient complete heart block (11 cases). The spectrum of non-embolic AEs is shown in Table 4.
Discussion
The high rate of mortality in pediatric PVS patients is well described, with multi-center series reporting 3-year survival from presentation 49–58.7 % [9, 10] and a large series from our center reporting 4-year survival at 44 % [1]. Less is known about the morbidity associated with PVS management. This study is the first to characterize the significant burden of systemic embolic AEs in pediatric patients requiring catheter management of PVS.
Clinically evident embolic AEs complicated 2.7 % of catheterizations in our series. If the additional two perioperative strokes excluded from analysis were in fact due to the preceding catheterization, the incidence would rise to 3.2 %. Viewed from the standpoint of stroke prevalence, at least 7.6 % of the PVS patients in this cohort suffered a clinically relevant stroke over the course of their treatment. In contrast, a large multi-center study on congenital catheterization outcomes identified only one stroke out of 2148 interventional congenital catheterizations [2], suggesting that the PVS population is at much higher risk than other patients. One may hypothesize that the high rate of embolism following PVS angioplasty is due to some combination intimal disruption with subsequent thrombosis at the angioplasty site, mobilization of pre-exiting thrombus in vessels subject to stagnant flow and its sudden relief, clot formation in long sheaths or on catheters/balloons placed into the left atrium, clot formation on stents placed within obstructed veins, or embolization of obstructing neointimal tissue [8].
Our study design was chosen to focus on potentially modifiable risk factors for embolic AEs. No such factors were identified, although the low number of cases significantly limits the power to detect such factors. Anticoagulation management appears to have been essentially identical in case and control catheterizations, as do case time and time spent in the left atrium. Cutting balloon use did not differ significantly between cases and controls. Thrombus or air was seen in a long sheath or pulmonary vein in 3 of the 11 cases, but also in 2 of 11 controls, suggesting that such findings are not necessarily predictive of clinical events. Since each patient served as her own control, this analysis is unable to assess patient-specific factors which may put individual children with PVS at higher risk for embolism. For example, we are unable to determine whether cyanotic congenital heart disease may be a risk factor. Many of our PVS patients are on aspirin (warfarin use is rare), but we are unable to assess for any protective effect.
None of the cases complicated by systemic emboli involved placement of a pulmonary vein stent. One of the two strokes excluded from analysis due to close proximity between cath and surgery did involve placement of stent which acutely thrombosed (prompting urgent operative management). Nevertheless, given our findings, it seems unlikely that thrombus formation on bare stent struts plays a major role in the etiology of embolic AEs in this population.
As noted above, these findings must be interpreted with the caveat that the relatively small number of affected cases limits the power of this study to detect potentially relevant risk factors. Additionally, this study may be hampered by incomplete case ascertainment. Given the extent of chart review performed, we think it is unlikely that any clinically apparent strokes were missed. It is important to consider, however, that clinically silent cerebral embolism does occur. In a study of adults undergoing catheterization for coronary angiography, brain MRI performed pre- and post-procedure found clinically silent, new cerebral infarctions in 15 % of patients [3]. If some proportion of PVS catheterizations are indeed complicated by silent strokes (including possibly some of those used as control catheterizations in our analysis), our ability to detect relevant risk factors may be reduced. Moreover, liver function and renal function studies are not uniformly assessed post-procedure on all PVS patients, raising the possibility that hepatic or renal emboli may similarly be missed. Overcoming this limitation would require prospective screening for clinically silent emboli.
Our series gives for the first time a detailed picture of the AEs complicating pulmonary vein angioplasty. We viewed the need for inotropic support and active anesthetic management during pulmonary vein angioplasty as part of the procedural safety net rather than as AEs. Similarly, given the hemodynamic stresses of the procedure and alterations in pulmonary mechanics related to changing pulmonary venous pressures and flow patterns, we did not consider post-procedure mechanical ventilation and admission to the CICU to be AEs. Even when excluding these arguably ‘adverse’ patient experiences, the rate of AEs was high. Many of the AEs were transient and manageable, but essentially all of the events listed in Table 3 have the potential to contribute to hemodynamic or respiratory embarrassment. It is notable that only two cardiac perforations from Brockenbrough were reported in 406 cases, despite potentially small/abnormal left atria in this patient population (for example, in patients with repaired total anomalous pulmonary venous return). Indeed, both of these perforations occurred in the same patient (who had a notably small left atrium); in neither instance did a significant pericardial effusion or hemodynamic instability develop.
Several general features of PVS angioplasty deserve further comment. Our descriptive data demonstrate that these cases tend to be long and to involve high fluoroscopy exposure and contrast dose. One of our group’s strategies to minimize case time is the routine use of long sheaths. This allows rapid catheter exchange, decreases the likelihood of losing wire position during exchanges, and provides the ability to stabilize balloon catheters with forward pressure on the long sheath (to avoid ‘milking out’ of a noncompliant distal vessel). Although entering severely stenotic veins can be time-consuming, the combination of a modified (cut) right or left coronary catheter with a long sheath achieves success almost all of the time. Moreover, angiography performed through the long sheath allows rapid reassessment of vein anatomy between dilations while avoiding the need to insert/remove an angiographic catheter. The pulmonary venous anatomy can be challenging to understand, and multiple-angled views are often necessary to understand lesions and branching patterns (especially if stent placement is being considered). This fact, along with the need to assess for iatrogenic flaps/aneurysms following each dilation, contributes to the high utilization of contrast and fluoroscopy. Aside from long sheath use, other strategies to minimize time spent in the left atrium include performance of pulmonary artery wedge angiograms in each lobe (to localize the ‘target’ before entering the left atrium), the use of accessory wires to stabilize sheath position (for example, leaving a wire in the left upper pulmonary vein while dilating the left lower vein), and intentional overdilation of distal vessels to improve balloon stability across more proximal pulmonary vein lesions. Despite these strategies, the patient burden of time, radiation, and contrast remains significant. The cumulative and long-term sequelae of radiation exposure for these patients remain unknown.
Although this study was underpowered and no modifiable risk factors for systemic embolic events were identified, we believe that this series is of clinical value. Having a better understanding of the risks associated with transcatheter management will improve the counseling of families both at the time of PVS diagnosis and in the periprocedural interval. Recognition of the significant absolute risk of systemic embolism during PVS angioplasty may reinforce the need for meticulous management of sheaths, catheters, and anticoagulation, although our findings do not suggest that this will mitigate the risk. Identification of cases of both renal and hepatic emboli, in addition to strokes, may suggest that more attention should be paid to assessment of end-organ function post-procedure.
Our findings on AEs must be viewed within the context of the improved quantity and quality of life that PVS angioplasty offers many families. Moreover, one sees that in the majority of cases PVS can be treated without significant AEs and that many of the AEs that do occur are self-limited or transient. Although the risk of stroke appears to be much higher for PVS angioplasty than for other pediatric catheterizations, the absolute risk is low. When faced with these data on the one hand and the bleak natural history of untreated PVS on the other, we believe that many families will continue to pursue angioplasty as a treatment modality.
Multidisciplinary management of PVS includes surgical and medical therapies in addition to transcatheter ones. These treatment modalities carry their own risks [4, 7], above and beyond those described here. It is clear from the collective data on morbidity and mortality that there remains tremendous room to improve as we work to increase both the quality and quantity of life in this vulnerable population.
Statement of Research Ethics: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments. For this type of study, formal consent is not required.
References
Balasubramanian S, Rehman M, Gauvreau K, Jenkins KJ (2012) Bilateral disease and early age at presentation are associated with shorter survival in patients with congenital heart disease and intraluminal pulmonary vein stenosis. Congenit Heart Dis 7(4):378–386
Bergersen L, Marshall A, Gauvreau K, Beekman R, Hirsch R, Foerster S et al (2010) Adverse event rates in congenital cardiac catheterization—a multi-center experience. Catheter Cardiovasc Interv 75(3):389–400
Busing KA, Schulte-Sasse C, Fluchter S, Suselbeck T, Haase KK, Neff W et al (2005) Cerebral infarction: incidence and risk factors after diagnostic and interventional cardiac catheterization—prospective evaluation at diffusion-weighted MR imaging. Radiology 235(1):177–183
Kanter KR, Kirshbom PM, Kogon BE (2014) Surgical repair of pulmonary venous stenosis: a word of caution. Ann Thorac Surg 98(5):1687–1692
Lacour-Gayet F, Zoghbi J, Serraf AE, Belli E, Piot D, Rey C et al (1999) Surgical management of progressive pulmonary venous obstruction after repair of total anomalous pulmonary venous connection. J Thorac Cardiovasc Surg 117(4):679–687
Peng LF, Lock JE, Nugent AW, Jenkins KJ, McElhinney DB (2010) Comparison of conventional and cutting balloon angioplasty for congenital and postoperative pulmonary vein stenosis in infants and young children. Catheter Cardiovasc Interv 75(7):1084–1090
Rehman M, Jenkins KJ, Juraszek AL, Connor JA, Gauvreau K, Muneeb M et al (2011) A prospective phase II trial of vinblastine and methotrexate in multivessel intraluminal pulmonary vein stenosis in infants and children. Congenit Heart Dis 6(6):608–623
Sadr IM, Tan PE, Kieran MW, Jenkins KJ (2000) Mechanism of pulmonary vein stenosis in infants with normally connected veins. Am J Cardiol 86(5):577–579 A10
Seale AN, Webber SA, Uemura H, Partridge J, Roughton M, Ho SY et al (2009) Pulmonary vein stenosis: the UK, Ireland and Sweden collaborative study. Heart 95(23):1944–1949
Seale AN, Uemura H, Webber SA, Partridge J, Roughton M, Ho SY et al (2013) Total anomalous pulmonary venous connection: outcome of postoperative pulmonary venous obstruction. J Thorac Cardiovasc Surg 145(5):1255–1262
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Esch, J.J., Porras, D., Bergersen, L. et al. Systemic Embolic Complications of Pulmonary Vein Angioplasty in Children. Pediatr Cardiol 36, 1357–1362 (2015). https://doi.org/10.1007/s00246-015-1165-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-015-1165-x