Abstract
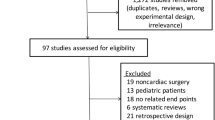
This report aims to provide a general description of the cardiovascular effects of dexmedetomidine, emphasizing its effects on conduction, and to give an evidence-based review of the literature regarding the use of dexmedetomidine to treat and prevent tachyarrhythmias in infants and children. A computerized bibliographic search of the literature on the use of dexmedetomidine to treat and prevent arrhythmias in infants and children was conducted. The cardiovascular effects of dexmedetomidine have been well studied in animal and adult human models. Growing experience, mostly in the pediatric population, has demonstrated the potential therapeutic applications of dexmedetomidine in the acute treatment of arrhythmias. Additionally, its use during cardiac surgery has been associated with a decreased incidence of postoperative ventricular and supraventricular tachyarrhythmias. Although dexmedetomidine is not currently approved by the Food and Drug Administration for the pediatric population, findings have shown it to be effective in various clinical scenarios for sedation. In addition, recent studies show that dexmedetomidine may have promising properties for the acute treatment and prevention of tachyarrhythmias.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dexmedetomidine (Precedex; Hospira Worldwide Inc., Lake Forest, IL, USA) is an α2-adrenergic receptor agonist used with increasing frequency in both the intensive care unit (ICU) and the perioperative setting. Although the chemical structure of dexmedetomidine resembles that of clonidine, its α2:α1 specificity ratio is 1,600:1 compared with 200:1 for clonidine.
In 1999, dexmedetomidine initially received approval by the United States Food and Drug Administration (FDA) for short-term (<24 h) provision of sedation for adult patients in the ICU setting who were receiving mechanical ventilation with endotracheal intubation. More recently, dexmedetomidine has received FDA approval for monitored anesthesia care in adults. To date, although dexmedetomidine does not have FDA approval for any pediatric indication, clinicians have an increasing body of clinical experience with its use in many scenarios including intraoperative application as part of a balanced anesthetic technique, provision of sedation during mechanical ventilation, sedation and anxiolysis for the nonintubated pediatric ICU patient, prevention of emergence delirium, and use as an agent for procedural sedation [29, 31].
The adverse effects of dexmedetomidine that have received the most attention in the adult population and continue to provide the most concern are hypotension and bradycardia. In particular, the morbidity and even the potential mortality related to the negative chronotropic and dromotropic effects of dexmedetomidine have been highlighted in the adult literature [2, 10, 14, 27, 33]. The incidence of such problems is greater when dexmedetomidine is administered with other medications that possess negative chronotropic effects (propofol, succinylcholine, digoxin, pyridostigmine) in scenarios (hypothermia or during vagotonic procedures such as laryngoscopy) that may have exaggerated their negative chronotropic effects and after large or rapid bolus doses [1, 8, 9, 16, 19, 23, 24, 30].
Nevertheless, anecdotal experience with dexmedetomidine in the pediatric population has demonstrated its potential therapeutic applications in the treatment of tachyarrhythmias. Its administration during surgery for congenital heart disease (CHD) may decrease the incidence of postoperative arrhythmias. This report reviews the electrophysiologic properties of dexmedetomidine as well as reports outlining its potential application in the treatment or prevention of tachyarrhythmias.
Electrophysiologic Properties
The electrophysiologic properties of dexmedetomidine have been assessed in two pediatrics studies [4, 11]. The first study by Hammer et al. [11] was a prospective nonrandomized series in which each patient served as his or her own control. In this study, 12 children ranging in age from 5 to 17 years underwent standard ablation of supraventricular accessory pathways, then had electrophysiologic variables measured before and after the administration of dexmedetomidine (1 μg/kg during 10 min followed by a 10-min continuous infusion of 0.7 μg/kg/h).
After the administration of dexmedetomidine, the authors reported that sinus node function was depressed, as evidenced by an approximate 38 % increase in the corrected sinus node recovery time (p < 0.01) and a 30 % increase in the sinus cycle length (p < 0.01). The atrioventricular (AV) nodal properties also were prolonged, as evidenced by an increase in the PR interval from 144 ± 19 to 162 ± 17 ms (p < 0.01), an increase in the Wenckebach cycle length, and a 20 to 25 % increase in the AV nodal refractory periods (p < 0.02). Atrial tissue refractoriness was not affected. A trend toward prolongation of the ventricular tissue properties was evident based on a slightly increased effective refractory period from 220 ± 22 to 230 ± 19 ms (p = 0.06) and a QTc interval increased from 394 ± 9 to 424 ± 9 ms (p < 0.01).
The study, however, did not include a formal control group, and the measurements were performed under the effect of other medications including ketamine and propofol. Although the electrophysiologic effects of these latter drugs are not well described, they could have potentially influenced the effects of dexmedetomidine in a synergistic or additive manner.
Furthermore, this study did not take into consideration the negative correlation effect that exists between heart rate (HR), PR interval, and the other AV nodal periods, so no adjustments were made. Despite the negative dromotropic effects noted by the investigators, none of the patients experienced sinus pause or any type of AV block.
A broader picture showing the effect of dexmedetomidine on the cardiac conduction system was provided by a subsequent prospective, observational controlled study by Chrysostomou et al. [4], who investigated changes noted on the surface electrocardiogram. The study included 76 children ranging in age from 0 to 17 years with CHD who were evaluated after surgery for CHD. Of the 76 patients in the cohort, 51 received dexmedetomidine for sedation, and 25 who did not receive dexmedetomidine served as a control group.
The dexmedetomidine group received a 1-μg/kg (interquartile range [IQR], 0.5 μg/kg) loading dose followed by a maintenance infusion at 1 μg/kg/h (IQR, 0.5 μg/kg) for 15 h (IQR, 10 h). The administration of dexmedetomidine was followed by a decrease in HR from 140 ± 22 to 115 ± 23 bpm (p < 0.001). Neonates and infants had a greater decrease in HR than older children (p < 0.001), whereas other parameters were similar.
In the dexmedetomidine group, when correction for HR was not used, the PR interval increased from 115 ± 28 to 122 ± 29 ms (p = 0.01), the QRS interval decreased from 84 ± 21 to 80 ± 21 ms (p = 0.02), and the QTc interval did not change (433 ± 47 to 435 ± 36 ms; p = 0.69). However, when the intervals were corrected for HR, the PRc was not prolonged (174 ± 38 to 167 ± 35 ms; p = 0.07). When the electrocardiographic (ECG) parameters were compared with those of the control group, which had not received dexmedetomidine, no differences were observed other than a trend toward a lower HR (p = 0.08).
Because the authors saw similar changes in the control group, they speculated that these changes likely reflected the normal postoperative course after cardiothoracic surgery and cardiopulmonary bypass. In contrast to the study by Hammer et al. [11], this study evaluated parameters during maintenance dexmedetomidine infusion and not after the loading dose. It is conceivable that electrophysiologic changes observed during peak dexmedetomidine levels dissipate with time. Additionally, no other anesthetic agents were being administrated in this group.
Antiarrhythmic Properties
The antiarrhythmic mechanism of dexmedetomidine action is not completely understood, and to date, no human electrophysiologic studies have evaluated this effect in detail. The currently proposed mechanism appears to be mediated primarily through enhancement of vagal neural activity. The dorsal motor nucleus of the vagus nerve and the nucleus ambiguous are important regions from which efferent parasympathetic nerves originate. The activity of these regions is regulated directly by the nucleus of tractus solitarius, at which an afferent vagal sensory input terminates [12, 17]. These nuclei are rich in α2-adrenoreceptors, and their activation by dexmedetomidine can lead to an enhancement of vagal activity. As shown in Fig. 1, similar to β-adrenergic receptor blockade and vagal maneuvers, this enhanced vagal activity can lead to decreased myocyte cyclic adenosine monophosphate (cAMP) and a reduction in the L-type Ca2+ current, which in turn leads to prolonged repolarization and a prolonged effective refractory period [21]. Subsequent physiologic changes seen vary among myocardial cells and depend on the location and density of the parasympathetic innervation and muscarinic receptors. Sinoatrial and AV nodes appear to have the highest density of muscarinic receptors, followed by the atria and ventricles [32]. In addition, this parasympathomimetic antiarrhythmic effect is more pronounced when cAMP is already stimulated and increased by either endogenous or exogenous catecholamines.
Proposed antiarrhythmic mechanism of dexmedetomidine action. ATP adenosine triphosphate, α 2 -receptor alpha2-adrenoreceptor, β-receptor beta adrenoreceptor, cAMP cyclic adenosine monophosphate, DMNV dorsal motor nucleus of the vagus, Gs stimulatory G protein, Gi inhibitory G protein, μ 2 receptor muscarinic cholinergic receptor, P inorganic phosphate
This proposed hypothesis concerning dexmedetomidine’s mechanism of action corresponds to what has been published to date regarding its antiarrhythmic effects. Dexmedetomidine has been successfully used to treat inappropriate sinus tachycardia, junctional and atrial ectopic tachycardias, and AV nodal-dependent reentrant supraventricular tachycardias (SVT). It also has been used to treat and prevent postoperative ventricular tachycardias [3, 5–7, 18, 20, 22].
Furthermore, besides its hypothesized parasympathomimetic, antiarrhythmic mechanism of action, dexmedetomidine possesses central sympatholytic properties through presynaptic activation of α2-adrenoreceptors in sympathetic nerve endings and subsequent negative feedback to the synaptic vesicle, resulting in inhibition of norepinephrine release. Snapir et al. [28] showed that in healthy adult volunteers and at the usual recommended dosage, dexmedetomidine can decrease plasma epinephrine and norepinephrine levels by approximately 70 %. This is of particular importance because dexmedetomidine may be used with the intention of attenuating the hypercatecholaminergic state seen after cardiac surgery and cardiopulmonary bypass and thereby decreasing the incidence of inappropriate tachycardia, particularly the catecholamine-driven ventricular and supraventricular tachyarrhythmias.
Applications of Dexmedetomidine in the Treatment of Tachyarrhythmias
The negative chronotropic effects of dexmedetomidine have been used as a therapeutic maneuver in various clinical scenarios. In the adult population, clinical experience has demonstrated its potential efficacy in treating inappropriate sinus tachycardia during off-pump coronary artery bypass grafting (CABG) and in preemptively decreasing the incidence of postoperative hyperadrenergic hemodynamic responses [15, 22].
In the study by Jalonen et al. [15], 80 adult patients scheduled for elective coronary artery bypass grafting were randomized to receive either a saline placebo or a dexmedetomidine infusion. Dexmedetomidine (1.5 μg/kg) was administered as a bolus dose during 30 min, followed by an infusion. Dexmedetomidine decreased the incidence of intraoperative (2 vs. 13 patients) and postoperative (5 vs. 16 patients) sinus tachycardia and also decreased the need for the use of β-adrenergic antagonists (3 vs. 11 patients).
The potential beneficial negative chronotropic effects of dexmedetomidine were further observed by Herr et al. [13] in their prospective trial comparing dexmedetomidine-based sedation with propofol-based sedation in 295 adults undergoing CABG surgery. At sternal closure, the patients were randomized to receive dexmedetomidine (bolus of 1 μg/kg during 20 min followed by an infusion of 0.2–0.7 μg/kg/h) to maintain a Ramsay sedation score of 3 or higher or to receive a propofol-based sedation regimen during mechanical ventilation. An evaluation of adverse events showed that no episodes of ventricular tachycardia occurred among the dexmedetomidine-sedated patients compared with a 5 % incidence among the patients sedated with propofol (p = 0.007). Additionally, the patients receiving dexmedetomidine had a decreased need for β-adrenergic antagonists (p = 0.014).
Chrysostomou et al. [3] were the first authors to use dexmedetomidine with the intention of treating tachyarrhythmias. This potential therapeutic role was first described in a retrospective review that outlined the antiarrhythmic effects of dexmedetomidine in 14 pediatric patients. Dexmedetomidine was used as the primary therapy for nine patients and as a rescue therapy for five patients. For the five patients, the primary treatment, which included either amiodarone or amiodarone and hypothermia, had failed. The treated arrhythmias included junctional ectopic tachycardia (JET), junctional accelerated rhythm (JAR), atrial ectopic tachycardia (AET), reentrant SVT, and atrial flutter (AF). Given the retrospective nature of the report, the dosing of dexmedetomidine was not controlled. Ten patients (71 %) received an average initial loading dose of 1.1 ± 0.5 μg/kg and 4 patients were started on a continuous infusion at 0.9 ± 0.3 μg/kg/h without a loading dose. The goals of therapy were conversion to normal sinus rhythm (NSR) within 3 min for SVT and within 2 h for all the other arrhythmias or a sufficient decrease in HR to improve hemodynamic function.
For all six patients with JET, dexmedetomidine was effective and decreased HR from 197 ± 22 to 165 ± 17 bpm within 32 min (range, 10–210 min). Dexmedetomidine was a first-line agent for five of the six patients. All four patients with SVT converted to NSR with the administration of dexmedetomidine. Conversion occurred with the loading dose in three patients, so a continuous infusion was not administered. In the fourth patient, an infusion without a bolus was chosen. In the one patient with AET, dexmedetomidine was administered as a rescue therapy using a loading dose followed by an infusion. Within 85 min, the rhythm converted to NSR. Two patients had JAR, and both received maintenance infusions only, which resulted in a decreased HR in both patients. Dexmedetomidine was not effective in the one patient with AF. In summary, the primary outcome was achieved for 13 (93 %) of 14 patients. Four patients experienced adverse effects. In three patients, hypotension responded to the administration of fluid. There was also a brief episode of complete AV block in one patient that was not thought to be related to dexmedetomidine. Nine patients, including the patients with JET and JAR, required transient pacing during the administration of dexmedetomidine to improve AV synchrony.
The same investigators evaluated the potential use of dexmedetomidine as a preemptive measure to prevent postoperative tachyarrhythmias in a prospective observational cohort of 32 pediatric patients undergoing surgery for CHD [5]. As a control group, 20 patients who did not receive dexmedetomidine were used. The dexmedetomidine infusion (0.76 ± 0.04 μg/kg/h) was started after the induction of anesthesia and then continued into the postoperative period for 38 ± 4 h. Postoperative arrhythmias occurred in only 2 (6 %) of the 32 patients who received dexmedetomidine versus 10 (50 %) of the 20 patients who did not receive dexmedetomidine (p = 0.001). The difference in arrhythmias included a 0 % versus a 25 % incidence of ventricular tachycardia (p = 0.01) and a 6 % versus a 25 % incidence of supraventricular arrhythmias (p = 0.05). Additionally, during the postoperative period, the patients who did not receive dexmedetomidine had a higher HR (141 ± 5 vs. 127 ± 3 bpm; p = 0.03) and more episodes of sinus tachycardia (40 vs. 6 %; p = 0.008). Transient complete heart block occurred for two control patients and for one patient who had received dexmedetomidine.
A third study by the same investigators provides additional information regarding the potential efficacy of dexmedetomidine in the acute treatment of AV nodal-dependent reentrant tachyarrhythmias [6]. As noted by the authors, the current drug of choice for the treatment of reentrant SVT is adenosine followed by verapamil or diltiazem. However, given the limitations of the current drug therapies and the significant adverse events that may be encountered, the authors suggest that an alternative effective and safe agent is needed. They performed a retrospective case series to describe their use of dexmedetomidine for the treatment of reentrant SVT in a cohort of 15 pediatric patients and compared the outcomes with those for a similar number of patients treated with adenosine. The patients ranged in age from 6 to 16 days (median, 10 days). Twenty-seven doses of dexmedetomidine (0.7 ± 0.3 μg/kg) were administered as a slow intravenous push for a total of 27 SVT episodes in the 15 patients. Successful conversion to NSR occurred in 26 of the 27 episodes (96 %) at a median time of 30 s (IQR, 20–35 s). The duration of the sinus pause was 0.6 s (IQR, 0.5–0.8 s). One episode of hypotension occurred and no episodes of bradycardia. The duration of the sedation was 34 ± 8 min. In comparison, five patients received 27 doses of adenosine, with conversion to NSR in 17 (63 %) of 27 episodes (p = 0.0017). Transient bradycardia and hypotension occurred for 3 patients (11 %), agitation for 16 patients (59 %), and bronchospasm for 1 patient. The duration of sinus pause was significantly longer with adenosine (2.5 s; IQR, 2–9 s; p < 0.001).
Discussion
Dexmedetomidine (Precedex) is an α2-adrenergic agonist that shares structural and physiologic similarities with clonidine. It currently is approved by the FDA for continuous infusions up to 24 h long for adult ICU patients initially intubated and receiving mechanical ventilation as well as for monitored anesthesia care. As described earlier, for the pediatric population, besides its potential use in various clinical scenarios for sedation, few reports have suggested its potential use as a therapeutic agent for the treatment and prevention of various tachyarrhythmias, especially in the postoperative setting after cardiac surgery (Table 1).
Although higher doses of dexmedetomidine have been used, dosing in the pediatric population for sedation and analgesia generally includes a loading dose of 0.3–1 μg/kg administered during 5–10 min after a continuous infusion of 0.3–1.5 μg/kg/h. In the setting of arrhythmias, the reported dosing varies. For acute treatment, a loading dose of 0.3–2.0 μg/kg usually is required and can be given as a slow push (particularly for reentrant SVT). When dexmedetomidine is used for prevention of postoperative arrhythmias, a loading dose of 0.5–1.0 μg/kg followed by an infusion of 0.5–1.5 μg/kg/h has been administered.
The precise mechanism for the antiarrhythmic action of dexmedetomidine remains hypothetical. However, the current evidence supports a primary parasympathomimetic effect that results in alteration of the Ca2+ current across the myocyte cell membrane and a secondary or additive central sympatholytic effect.
Although the evidence still is not substantial, dexmedetomidine appears to have several advantages over other conventional antiarrhythmic agents. In the setting of infants with reentrant SVT, compared with adenosine, dexmedetomidine does not appear to cause any significant sinus pause or asystole, so patients do not experience the feeling of “impending doom” usually seen in 7–10 % of patients after adenosine. It has a longer duration of action and thus is useful for patients with multiple breakthrough SVT episodes and causes no bronchoconstriction.
In the setting of postoperative JET, dexmedetomidine has a dual purpose because it can be used both as a sedative/analgesic and as an antiarrhythmic agent. Thus, other medications such as benzodiazepines and opioids can be spared, or their doses can be reduced significantly. Dexmedetomidine can decrease the endogenous hypercatecholaminergic state after cardiac surgery, which is an important factor for patients with JET. Compared with amiodarone, it has a shorter half-life, so if any bradyarrhythmias are encountered, its effect can dissipate within hours instead of days. It prevents shivering, so if hypothermia is implemented, neuromuscular blockade may not be needed.
Dexmedetomidine can be used as an adjunct to other conventional antiarrhythmics. In addition, it has no negative inotropic or protachyarrhythmic effects, in contrast to many other agents such as β-adrenergic antagonists and amiodarone. Therefore, it can be used relatively safely for patients after cardiac surgery, either for the acute treatment or for prevention of tachyarrhythmias.
Despite these novel effects of dexmedetomidine, it is important for the clinician to select the appropriate patients and clinical settings for its safest use. Current data support its use only by experienced personnel including intensivist care physicians, anesthesiologists, and emergency room physicians in a monitored care setting. Although the hemodynamic adverse effect profile (including hypotension, hypertension and bradycardia) is for the most part predictable and can be largely avoided by careful patient selection and dose titration, significant hemodynamic adverse events still may occur [25, 26]. Large doses or rapid intravenous boluses should be used with caution in various patient populations and clinical scenarios including significantly depressed ventricular function and hemodynamic instability, recent high-degree AV block, premature neonates, intravascular volume depletion, hepatic disease, and significant hypoalbuminemia.
Additionally, dexmedetomidine should be used with caution in patients already receiving medications that have significant negative chronotropic properties (first-generation calcium-channel antagonists and β-adrenergic antagonists) and those with a low prearrhythmia basal HR. Its respiratory adverse effect profile is limited, so it can be used for both intubated and nonintubated patients. However, due to its sedative effect, whenever feasible, appropriate nothing-by-mouth guidelines should be followed as with any other sedative agent.
With these caveats in mind, dexmedetomidine appears to be a useful therapeutic agent for the prevention and treatment of arrhythmias including reentrant SVT, JET, and AET, as well as for prevention of ventricular tachycardia. Future prospective trials are needed to define its role in these settings.
References
Berkenbosch JW, Tobias JD (2003) Development of bradycardia during sedation with dexmedetomidine in an infant concurrently receiving digoxin. Pediatr Crit Care Med 4:203–205
Bharati S, Pal A, Biswas C, Biswas R (2011) Incidence of cardiac arrest increases with the indiscriminate use of dexmedetomidine: a case series and review of published case reports. Acta Anaesthesiol Taiwan 49:165–167
Chrysostomou C, Beerman L, Shiderly D et al (2008) Dexmedetomidine: a novel drug for the treatment of atrial and junctional tachyarrhythmias during the perioperative period for congenital cardiac surgery: a preliminary study. Anesth Analg 107:1514–1522
Chrysostomou C, Komarlu R, Lichtenstein S, Shiderly D, Arora G, Orr R, Wearden PD, Morell VO, Munoz R, Jooste EH (2010) Electrocardiographic effects of dexmedetomidine in patients with congenital heart disease. Intensive Care Med 36:836–842
Chrysostomou C, Sanchez-de-Toledo J, Wearden P et al (2011) Perioperative use of dexmedetomidine is associated with decreased incidence of ventricular and supraventricular tachyarrhythmias after congenital cardiac operations. Ann Thorac Surg 92:964–972
Chrysostomou C, Morell VO, Wearden P et al (2013) Dexmedetomidine: therapeutic use for the termination of reentrant tachycardia. Congenit Heart Dis 8(1):48–56
Delwadia S, Naguib A, Tobias J (2012) Dexmedetomidine controls supraventricular tachycardia following cardiac surgery in a child. World J Pediatr Congenit Heart Surg 3:406–409
Deutsch E, Tobias JD (2007) Hemodynamic and respiratory changes following dexmedetomidine administration during general anesthesia: sevoflurane vs desflurane. Paediatr Anaesth 17:438–444
Finkel JC, Quezado ZMN (2007) Hypothermia-induced bradycardia in a neonate receiving dexmedetomidine. J Clin Anesth 19:290–292
Gerlach AT, Murphy CV (2009) Dexmedetomidine-associated bradycardia progressing to pulseless electrical activity: case report and review of the literature. Pharmacotherapy 29:1492–1494
Hammer GB, Drover DR, Jackson E (2008) The effects of dexmedetomidine on cardiac electrophysiology in children. Anesth Analg 106:79–83
Hayashi Y, Sumikawa K, Maze M, Yamatodani A, Kamibayashi T, Kuro I (1991) Dexmedetomidine prevents epinephrine induced arrhythmias through stimulation of central alpha two adrenoreceptors in halothane anesthetized dogs. Anesthesiology 75:113–117
Herr DL, Sum-Ping ST, England M (2003) ICU sedation after coronary artery bypass graft surgery: dexmedetomidine-based versus propofol-based sedation regimens. J Cardiothorac Vasc Anesth 17:576–584
Ingersoll-Weng E, Manecke GR, Thistlethwaite PA (2004) Dexmedetomidine and cardiac arrest. Anesthesiology 100:738–739
Jalonen J, Hynynen M, Kuitunen A, Heikkilä H, Perttilä J, Salmenperä M, Valtonen M, Aantaa R, Kallio A (1997) Dexmedetomidine as an anesthetic adjunct in coronary artery bypass grafting. Anesthesiology 86:331–345
Jooste EH, Muhly WT, Ibinson JW et al (2010) Acute hemodynamic changes following rapid intravenous bolus dosing of dexmedetomidine in pediatric heart transplant patients undergoing routine cardiac catheterization. Anesth Analg 111:1490–1496
Kamibayashi T, Hayashi Y, Mammoto T, Yanatodani A, Sumikawa K, Yoshiya I (1995) Role of the vagus nerve in the antidysrhythmic effects of dexmedetomidine on halothane/epinephrine dysrhythmias in dogs. Anesthesiology 83:992–999
LeRiger M, Naguib A, Galantowicz M, Tobias JD (2012) Dexmedetomidine controls junctional ectopic tachycardia during tetralogy of Fallot repair in an infant. Ann Card Anaesth 15:224–228
Mason KP, Zurakowski D, Zgleszewski SE et al (2008) High-dose dexmedetomidine as the sole sedative for pediatric MRI. Paediatr Anaesth 18:403–411
Ohsugi E, Nagamine Y, Ohtsuka M (2011) The effect of dexmedetomidine in a child with intractable supraventricular tachyarrhythmias after total cavopulmonary connection. Masui 60:493–495
Parent B, Munoz R, Shiderly D, Chrysostomou C (2010) Use of dexmedetomidine in sustained ventricular tachycardia. Anaesth Intensive Care 38:781–782
Ruesch S, Levy JH (2002) Treatment of persistent tachycardia with dexmedetomidine during off-pump cardiac surgery. Anesth Analg 95:316–318
Salmenpera MT, Szlam F, Hug CC Jr (1993) Anesthetic and hemodynamic interactions of dexmedetomidine and fentanyl in dogs. Anesthesiology 78:813–820
Scheinin H, Jaakola ML, Sjövall S, Ali-Melkkilä T, Kaukinen S, Turunen J, Kanto J (1993) Intramuscular dexmedetomidine as premedication for general anesthesia: a comparative multicenter study. Anesthesiology 78:1065–1107
Shah A, Koneru J, Nicoara A et al (2007) Dexmedetomidine-related cardiac arrest in a patient with permanent pacemaker: a cautionary tale. PACE 30:1158–1160
Shepherd SM, Tejman-Yarden S, Khanna S et al (2011) Dexmedetomidine-related atrial standstill and loss of capture in a pediatric patient after congenital heart surgery. Crit Care Med 39:187–189
Sichrovsky TC, Mittal S, Steinberg JS (2008) Dexmedetomidine sedation leading to refractory cardiogenic shock. Anesth Analg 106:1784–1786
Snapir A, Posti J, Kentala E et al (2006) Effects of low and high plasma concentrations of dexmedetomidine on myocardial perfusion and cardiac function in healthy male subjects. Anesthesiology 105:902–910
Tobias JD (2007) Dexmedetomidine: applications in pediatric critical care and pediatric anesthesiology. Pediatr Crit Care Med 8:115–131
Tobias JD (2008) Bradycardia during dexmedetomidine and therapeutic hypothermia. J Intensive Care Med 23:403–408
Tobias JD, Gupta P, Naguib A, Yates A (2011) Dexmedetomidine: applications in the pediatric patient with congenital heart disease. Pediatr Cardiol 32:1075–1087
Wang H, Han H, Zhang L et al (2001) Expression of multiple subtypes of muscarinic receptors and cellular distribution in the human heart. Mol Pharmacol 59:1029–1036
Zhang X, Schmidt U, Wain JC, Bigatello L (2010) Bradycardia leading to asystole during dexmedetomidine infusion in an 18-year-old double-lung transplant recipient. J Clin Anesth 22:45–49
Acknowledgments
We thank Dr. Angelo Rutty from the Heart Institute at the Children’s Hospital of Pittsburgh for the illustration.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tobias, J.D., Chrysostomou, C. Dexmedetomidine: Antiarrhythmic Effects in the Pediatric Cardiac Patient. Pediatr Cardiol 34, 779–785 (2013). https://doi.org/10.1007/s00246-013-0659-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-013-0659-7