Abstract
This study aimed to determine mean pulmonary arterial pressure (PAPmean) and pulmonary vascular resistance (PVR) using transthoracic echocardiography (TTE) measurements of the pulmonary artery flow velocity curve in children with pulmonary arterial hypertension (PAH) and congenital heart disease when the tricuspid regurgitant velocity (TRV) is not sufficient. This study enrolled 29 congenital heart disease cases with pulmonary arterial hypertension and 40 healthy subjects followed at our center. The mean age was 66.9 ± 77.9 months in the patient group and 76.3 ± 62.1 months in the control group. A positive correlation was found between TRV and systolic pulmonary arterial pressure (r = 0.394, p = 0.035, 95 % confidence interval [CI] = 0.032–0.665), whereas a negative correlation was found between corrected acceleration time (AcTc) and PAPmean (r = −0.559, p = 0.002, 95 % CI = −0.768 to −0.242). Furthermore, a negative correlation was found between parameters TRV and AcTc (r = −0.383, p = 0.001, 95 % CI = −0.657 to −0.019). Based on the cutoff criterion of 124 ms for AcTc, sensitivity was found to be 79.3 % and specificity to be 77.5 % in distinguishing between the PAH patients and the healthy control patients (receiver operating characteristic [ROC] area under the curve [AUC] = 0.804, 95 % CI = 0.691–0.890, p < 0.0001). The sensitivity and specificity of the concomitant use of AcTc and/or TRV were found to be 90 and 73 %, respectively, in distinguishing between the PAH patients and the the healthy control patients. The data obtained by TTE also can be appropriate for measuring PAPmean, PVR, and the vasoreactivity test and for determining the priority of implementing cardiac catheterization even if there is no measurable TRV value.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
According to current guidelines, pulmonary arterial hypertension (PAH) is defined by a mean pulmonary artery pressure (PAPmean) of 25 mmHg or higher at rest, a pulmonary vascular resistance index (RpI) higher than 3 Wood U/m2, and a pulmonary capillary wedge pressure (PCWP) of 15 mmHg or lower at cardiac catheterization [1, 11]. The most common cause of childhood PAH is congenital cardiac diseases.
In children with PAH, the status of the pulmonary vascular bed is the main factor for determining clinical manifestations, course, prognosis, and surgical treatment option [16]. The gold standard method for measurement of pulmonary arterial pressure (PAP) and pulmonary vascular resistance (PVR) is cardiac catheterization. However, the invasive process of cardiac catheterization, the necessity of anesthesia during the procedure, the method of measurement, complications that occur during the identification of vasoreactivity with pharmacologic agents, and errors in calculations represent the major risk factors [14, 22].
In clinical practice, the measurement of maximum tricuspid regurgitant flow velocity (TRV), performed by noninvasive transthoracic echocardiography (TTE), can estimate systolic pulmonary artery pressure PAPsystolic and is widely used [30]. With this method, a measurable TRV is essential for the noninvasive determination of PAPsystolic. However, the measurements with cardiac catheterization have shown that PAH may be present in some patients despite the lack of measurable TRV [3].
Studies have determined that measurements of pulmonary artery Doppler flow velocity curves performed by noninvasive TTE are correlated with invasive PAPmean and PVR measurements [19, 26, 29]. Evaluation of the pulmonary vascular bed using echocardiographic techniques and the feasibility of the pulmonary vasoreactivity test (PVT) provide great benefits in both the management and the follow-up evaluation of childhood congenital heart disease (CHD) patients and in the timing of the surgery. Identification of noninvasive echocardiographic parameters that can be used in the diagnosis and follow-up evaluation of patients with pulmonary hypertension reduces the requirements of catheter angiography and protects patients from the risks of this procedure.
The correlation between pulmonary artery flow velocity measurements and TRV has not been established for children with PAH and CHD. We hypothesized that PAPmean and PVR, the most important predictors in the follow-up evaluation of children with CHD and PAH, obtained from the cardiac catheterization are correlated with pulmonary artery flow velocity measurements. For this purpose, measurements of pulmonary artery flow velocity curves were performed with concurrent cardiac catheterization and TTE in the catheterization laboratory for patients with PAH, CHD, and clinical indication for cardiac catheterization in our study.
Methods
Study Design
The study included 29 CHD patients with a diagnosis of PAH established by a mean PAP (PAPmean) of 25 mmHg or higher, an RpI higher than 3 Wood U/m2, and a PCWP of 15 mmHg or lower at cardiac catheterization for diagnostic purposes at the Gazi University Faculty of Medicine, Department of Pediatric Cardiology, between March 2010 and April 2011. The control group included 40 healthy children without clinical or echocardiographic pathology consulted by the Department of Pediatric Cardiology.
The inclusion criteria specified CHDs and PAH. The exclusion criteria ruled out primary pulmonary hypertension, familial pulmonary hypertension, persistent pulmonary hypertension, and evidence of any systemic or lung disease. No patients had artificial ventilation with intubation, cardiac surgery, or stenosis that could create a gradient in the pulmonary valve and outflow tract.
The patient group underwent concurrent cardiac catheterization and TTE at the catheter angiography laboratory. Echocardiographic and invasive hemodynamic measurements were repeated before and after the pulmonary vasoreactivity test. The echocardiographic parameters of the patients were compared with those of the healthy control group. Before the study, ethics committee approval and written consent of parents were obtained for the patients and control subjects.
Echocardiographic Examinations
Echocardiographic examination was performed with Vivid 7 Pro Echo devices (General Electric Medical Systems Company, Milwaukee, WI, USA) using 3-, 5-, and 7-MHz probes. All the measurements were performed by the same specialist in pediatric cardiology. Within the scope of the method used to measure the pulmonary artery flow velocity curve, as described previously [12, 27, 29], pulsed-wave Doppler interrogation of the proximal pulmonary artery was performed using the parasternal short-axis view, with the sample volume placed at the annulus of the pulmonary valve. The pulsed-wave sample volume was placed at the annulus of the pulmonary valve but not more proximally in the right ventricular outflow tract so as to obtain maximal alignment for blood flow and Doppler interrogation. No correction of angles between the Doppler flow measurements was made.
All the investigations were recorded on Video Home System tape (JVC; Victor Company Ltd., Yokohama, Japan). The pulmonary artery flow velocity curve profile was assessed in two stages: the acceleration phase and the deceleration phase of the flow curve. In the flow curve, the deceleration phase can be assessed in two subphases limited by the inflexion point. The second peak point after the rapid deceleration during the period between the middle and late systoles is the inflexion point [19, 26, 29].
The relevant measurements were performed while the pulmonary artery flow velocity was assessed by the pulsed-wave Doppler. The definitions for the parameters were as follows. The acceleration time (AcT) was the interval from the beginning of the ejection to the peak flow velocity. The inflexion time (InT) was the period between the ejection and the inflexion points. The InT involved parts of the acceleration and deceleration phases. The deceleration time (DT) was the interval between the point at which the peak flow velocity occurred and the end of the ejection. The deceleration index (DI) was obtained by dividing the remainder after subtraction of the flow velocity at the inflexion point from peak flow velocity to the peak flow velocity. The corrected acceleration time (AcTc), corrected inflexion time (InTc), and corrected deceleration time (DecTc) were obtained by correcting the resulting data for heart rate (the data were divided by the square root of the time taken for one cardiac cycle). The measurements were repeated three times.
The TRV was defined as the maximum tricuspid regügitan jet flow on the tricuspid valve with continuous-wave Doppler in an apical four-chamber view of echocardiographic imaging. The interval between the onset of right ventricle ejection and the point of systolic pulmonary arterial flow cessation was defined as right ventricle ejection time (RVET).
All values used for the analysis represented the average of three consecutive cardiac cycles, except for patients with dysrhythmia, for whom five-beat averages were obtained.
Cardiac Catheterization
Cardiac catheterization was performed after sedation with midazolam 0.1 mg/kg. Pressures (PAP, right atrial pressure, left atrial pressure, and pulmonary arterial wedge pressure) were measured with fluid-filled catheters. Pulmonary and systemic blood flows were measured by the Fick method using the measured oxygen consumption and oxygen content derived from oxygen saturation. The PVR was calculated conventionally as the ratio of the difference between mean PAPmean and left atrial pressure or pulmonary arterial capillary wedge pressure to mean cardiac output, and the values were expressed as units per square meter.
Vasoreactivity Test
All the children underwent cardiac catheterization with simultaneous echocardiographic examination before and after the administration of 100 % inspired oxygen. All the pressure recordings and oxygen saturation samplings were performed before and after the administration of 100 % oxygen by mask for 10 min. The pulmonary vascular reactivity test (PVT) was considered positive if the PAPmean and the RpI/RsI ratio exhibited a reduction of more than 20 % [2, 15, 23].
Statistical Analysis
Normality was tested with the Shapiro–Wilks test. To compare each variable between groups, Student’s t tests, including Levene tests for comparison of variances, and Mann–Whitney U tests were used where appropriate. To compare the nominal data, Chi-square tests were used. The repeated measurements were evaluated using the paired t test or the Wilcoxon signed rank test where appropriate.
All the aforementioned tests and correlation tests were performed using Statistical Package for Social Sciences 19.0 (SPSS Inc., Chicago, IL, USA). For calculation and presentation of receiver operating characteristic (ROC) analyses, we used Med Calc 11.0 (Mariakerke, Belgium), and the graphical presentations were prepared using Microsoft Excel 2010 (Microsoft Corporation, Bellevue, USA). All tests were two-sided with a significance level of 0.05.
Results
The demographic, clinical, and baseline Doppler echocardiographic characteristics of 29 patients with PAH and CHD and 40 control subjects are compared in Table 1. The mean age of the patient group was 66.9 ± 77.9 months, and 55.2 % were female, whereas the mean age of control group was 76.3 ± 62.1 months, and 50 % were female.
The patient and control groups did not differ statistically in terms of age or gender. In addition, the patient and control groups did not differ significantly in terms of weight (p = 0.160), height (p = 0.426), body surface area (p = 0.181), or heart rate (p = 0.125) variables.
In terms of disorders, 14 patients had ventricular septal defects, 4 had atrioventricular canal defects, 3 had ventricular septal defects and atrial septal defects, 3 had patent ductus arteriosus, 3 had atrial septal defects, and 2 had an aorticopulmonary window. The patient and control groups showed a statistically significant difference in terms of Doppler echocardiographic parameters including AcT/RVET, AcTc, InTc, DecTc, DI, TRV, and AcTc/TRV except for the RVET (p < 0.005 for DI; p < 0.001 for AcT/RVET, AcTc, InTc, DecTc, DI, TRV, and AcTc/TRV).
All the patients underwent the vasoreactivity test by administration of 100 % oxygen with a simple face mask. The pretest values were as follows: PAPmean (57.1 ± 22.2 mmHg) and RpI (9.97 ± 8.28 Wood U/m²). The baseline cardiac catheterization findings in the patient group and the decrease in PAPmean, increase in pulmonary flow (Qp), and reduction in RpI and RpI/RsI were found to be statistically significant (p < 0.001) (Table 2). As shown in Table 3, 12 of the patients gave a positive response to the vasoreactivity test. In the responder group, the mean age (14.67 ± 24.42 months), weight (7.62 ± 3.13 kg), height (69.61 ± 11.21 cm), and body surface area (0.36 ± 0.11 m²) parameters were lower than those of the nonresponder group (p < 0.05).
The invasive hemodynamic findings and the Doppler parameters obtained from noninvasive TTE also were compared before and after pulmonary vasoreactivity testing between the responder and nonresponder groups (Table 4). The InTc and DI parameters were found to be significantly higher in the responder group than in the nonresponder group (311.7 ± 76.8 vs 267.5 ± 52.6, p < 0.05; 0.65 ± 0.10 vs 0.52 ± 0.19, p < 0.05, respectively).
The AcT/RVET and AcTc parameters differed significantly in the assessments performed before and after vasoreactivity testing in the responder group (0.27 ± 0.09 vs 0.35 ± 0.09, p < 0.01; 120.56 ± 18.77 vs 155.48 ± 27.75, p < 0.01). The AcT/RVET and DecTc parameters differed significantly between the before and after PVT assessments in the nonresponder group (0.27 ± 0.08 vs 0.32 ± 0.10, p < 0.05; 301.34 ± 78.42 vs 259.24 ± 60.73, p < 0.05) (Tables 5 and 6).
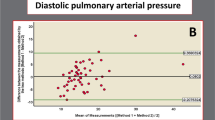
When the correlation between the parameters obtained invasively and the Doppler parameters obtained from noninvasive TTE before pulmonary vasoreactivity testing was determined, a moderate negative correlation was found between AcTc and PAPsystolic, PAPdiastolic, PAPmean, and RpI (AcTc and PAPsystolic: r = −0.478, p = 0.009, 95 % CI = −0.719 to −0.135; AcTc and PAPmean: r = −0.559, p = 0.002, 95 % CI = −0.768 to −0.242; AcTc and RpI: r = −0.481, p = 0.008, 95 % CI = −0.720 to −0.139). The findings showed TRV to have a moderate positive correlation only with PAPsystolic and RpI (TRV and PAPsystolic: r = 0.394, p = 0.035, 95 % CI = 0032–0665; TRV and RpI: r = 0.526, p = 0.003, 95 % CI = 0.198–0.748). According to the findings, InTc had a moderate negative correlation with PAPsystolic, PAPdiastolic and PAPmean. (PAPsystolic: r = −0.419, p = 0.024, 95 % CI = −0.681 to −0.062; PAPdiastolic: r = −0.387, p = 0.038, 95 % CI = −0.660 to −0.024; PAPmean: r = −0.376, p = 0.044, 95 % CI = −0.653 to −0.011).
The negative correlation between AcTc and parameters PAPsystolic, PAPmean, PAPdiastolic and RpI and the positive correlation between TRV and parameters PAPsystolic and RpI remained after pulmonary vasoreactivity testing, whereas a moderate negative correlation existed between DI and parameters PAPsystolic, PAPmean, PAPdiastolic, and RpI, which was not determined before the test (DI and PAPsystolic: r = −0.507, p = 0.005, 95 % CI = −0.737 to −0.173; DI and PAPmean: r = −0,467, p = 0.011, 95 % CI = −0.712 to −0.121; DI and RpI: r = −0.504, p = 0.005, 95 % CI = −0.735 to −0.169).
Figures 1 and 2 show the moderate negative correlation between AcTc and parameters PAPmean and PAPsystolic, and Fig. 3 shows the moderate positive correlation between TRV and parameter PAPsystolic. A moderate negative correlation was found between TRV and AcTc before the test (r = −0.383, p = 0.001, 95 % CI = −0.657 to −0.019) and after the test (r = −0.492, p = 0.007, 95 % CI = −0.153 to −0.727).
Figure 4 shows the correlation between AcTc and TRV. As shown in Fig. 5, based on the cutoff criterion of 124 ms for AcTc, sensitivity was found to be 79.3 % and specificity to be 77.5 % in distinguishing between the PAH patients and the healthy control group (ROC area under the curve [AUC] = 0.804, 95 % CI = 0.691–0.890, p < 0.0001). The sensitivity and specificity of TRV were found to be 69 and 95 %, respectively, in distinguishing between the PAH patients and the healthy control group depending on the criterion of more than 2.2 m/s (ROC AUC = 0.793, 95 % CI = 0.679–0.881, p < 0.0001) (Fig. 6). The findings showed TRV to be lower than 2.2 m/s in 9 (31 %) of 29 patients. Furthermore, AcTc was lower than 124 ms for six (66.6 %) of nine patients with a TRV lower than 2.2 m/s. The concomitant use of AcTc and TRV were found to have a sensitivity of 90 % and a specificity of 73 % in distinguishing between the PAH patients and the healthy control group.
Discussion
Currently, TTE is the main noninvasive diagnostic method used for the diagnosis and follow-up evaluation of children with CHD and pulmonary hypertension [7, 17]. The estimation of PAPsystolic with the measurement of TRV by TTE is widely accepted and clinically used [9]. However, PAPmean and PVR values are more important in the diagnosis of PAH, and patients with normal or immeasurably low levels of TRV may have higher PAP levels.
Early diagnosis PAH allows treatment of the disease before irreversible changes occur. The close monitoring of the high-risk patients, particularly those with CHDs, by noninvasive methods such as TTE is a decisive factor for the early diagnosis and prognosis of these patients [25].
The literature consists of studies that investigated the correlation of the time intervals obtained from the pulmonary flow velocity profile by Doppler echocardiography in the presence of PAH. In 1975, Hirschfeld et al. [13] established a correlation of pulmonary hypertension and the right ventricle preejection period with RVET on M-mode echocardiography after defining the right ventricular systolic time intervals. Tahara et al. [28] described the abnormal pulmonary artery velocity changes and flow profiles resulting from the abnormal pulmonary valve movements on experimental models of pulmonary hypertension.
On the other hand, Kitabatake et al. [19] were the first to investigate the AcT and the RVET time intervals on Doppler echocardiography in patients with pulmonary hypertension. In this study involving 33 adult patients, the results showed that this method could detect pulmonary hypertension at a rate of 90 %. It was shown that AcT and AcT/RVET values were inversely and highly correlated with mean PAP. Thus, AcT and AcT/RVET values were shown to be significant in the noninvasive evaluation of patients with PAH.
Cooper et al. [5] were the first to investigate the time intervals obtained from the pulmonary artery flow velocity curves by Doppler echocardiography in children with pulmonary hypertension. This study included 21 children with VSD and atrioventricular canal defect, whereas no healthy subjects were recruited.
In our study, time intervals were studied in healthy subjects and patients with PAH using the pulmonary artery flow velocity curve obtained by pulse-wave Doppler in sample volumes from distal right ventricular outflow tract, and significant differences were found in patients with PAH.
To date, the largest group of patients reviewed for pediatric pulmonary hypertension with noninvasive assessments belongs to those published by Nakahata et al. [26] and Ebeid et al. [8]. Nakahata et al. [26] included only patients 3 months to 8 years of age with left-to-right shunting, whereas Ebeid et al. [8] included patients without even specifying the PCWP or the lesions involving the left heart.
In the study by Ebeid et al. [8], the patients were categorized as having normal PVR, mild PVR, or high PVR. Whereas all the patients underwent catheter angiography, no concurrent TTE was performed. In addition to patients with intracardiac defects, those with left cardiac pathology also were included in this study. The results showed that AcT and AcT/RVET values were poor determinants of the PAP or PVR and that any alteration in these parameters was unable to indicate the increase in either PVR or pulmonary flow. On the other hand, AcTc was found to be significantly correlated with PVR as well as with PAPmean and PAPsystolic. These results were consistent with the results of the current study.
The response provoked by the PVT indicates the prognosis after surgical treatment or transplantation in CHD cases and the efficacy of response to chronic calcium canal blocker treatment in PAH patients. The research performed in adults more frequently has defined quantitative analysis of the AcT, RVET, the right ventricle preejection period (RPEP) by using the pulmonary flow velocity profile, and findings have shown the acceleration time to be inversely related to the mean and systolic PAP [4, 6]. Lanzarini et al. [21] reported that 64.7 % of the patients with PAH could be detected by an AcT shorter than 93 ms and that when combined with the other indices, this variable could be even more discriminative.
The current study detected a significant difference in AcTc, InTc, DI, and DecTc between the control subjects in accordance with the literature data. The normal values for AcT were given as 137 ± 24 ms by Kitabatake et al. [19] and as 150 ± 30 ms by Kosturakis et al. [20].
Dabestani et al. [6], in their study of 23 patients with PAH and 16 healthy adults, assessed PVR and PAP by Doppler echocardiography and found that AcT significantly correlated with PAP and PVR. If AcT was shorter than 100 ms, the sensitivity was 78 % and the specificity was 100 %. In this study, it was reported that Doppler echocardiography cannot be used for the numeric estimation of PAP but can be useful in differentiating the groups with normal and high PAP values.
To date, no studies reporting cutoff values for the time intervals of the pulmonary artery flow velocity measurements in children with PAH have been conducted. Although there was moderate correlation between invasive and noninvasive parameters, the values were not sufficient independently for cutoff values in our study. The cutoff values in the current study could be used to differentiate the children with and those without PAH. As the findings show, AcTc (<124.6 ms) would be beneficial for detecting PAH, with a sensitivity of 79.3 % and a specifity of 77.5 %.
In a study conducted by Nakahata et al. [26] including 45 children with a higher PAP and left-to-right shunting, PVR was intended to be identified by TTE, and the pulmonary vasoreactivity test was applied. The patients were divided into two subgroups: those with a PVR of 4.5 WU/m² or less and those with a PVR of 4.6 WU/m² or more. The patients, ranging in age from 0.25 to 8 years (mean, 1.4 years), were compared with 23 healthy control subjects. In contrast to the current study, patients with right-to-left shunting and older patients were not included in the study. For vasoreactivity testing, 100 % oxygen was used with a face mask.
Concurrent cardiac catheterization and TTE was performed for 11 of the 45 patients, whereas the remaining 34 patients were subjected to an investigation during a period of 6–24 h. The assessment of the pulmonary artery flow velocity indices showed that InTc significantly correlated with high PVR (sensitivity, 92 %; specificity, 90 %). Moreover, 22 patients underwent PVT, and among those with a positive response, AcTc, InTc, and peak flow rate increased, whereas DI decreased.
The comparison of the groups with positive and negative PVT showed significant changes for all four Doppler indices. Among these, InTc was the best in discriminating those with positive and negative PVT responses, with a sensitivity of 93 % and a specificity of 100 %. This study revealed that InTc is inversely correlated with PVR and more distinctive than other indices in identifying patients with low and high PVR values, and that InTc is prolonged, with a better pulmonary artery reactivity. Although InTc was inversely correlated with PVR, the low-PVR patients and control subjects were indifferent in the aspect of InTc. The authors concluded that InTc could be used to screen high and low PVR. However, the current study results show statistically significant differences between before and after PVT, AcTc, and AcT/RVET measurements for responders, while results show statistically significant differences between before and after PVT, InTc and DI measurements for nonresponders.
These findings suggest that pulmonary artery flow velocity measurements can be used to distinguish between responders and nonresponders, as well as between healthy individuals and children with CHD and PAH. The correlation detected between InTc and the PAPmean value before the vasoreactivity test, between DI and the PAPmean after the vasoreactivity test, and PVR values for estimation of the pulmonary vasoreactivity response is consistent with the literature data. The TTE indices that might be used to specify the PVT responses of patients with PAH include DI and InTc.
Fisher et al. [10], in a recent study conducted with 63 patients to determine the accuracy of PAPsystolic measurement with TRV by Doppler echocardiography found that 48 % of patients had a different PAPsystolic value (±10 mmHg) than that measured with catheter angiography and a more significant underestimation. Measurable TRV ranged between 39 and 86 % in all patients with PAH, although it could not be detected in all the patients [18].
McQuillan et al. [24] found a PAPsystolic value of 28.3 ± 4.9 mmHg (range, 15–57 mmHg) with the measurements in healthy children by using TRV and the modified Bernoulli equation and considering a right atrial pressure of 10 mmHg. The upper limit of PAPsystolic was considered to be 37.2 mmHg (TRV, 2.7 m/s) using this method when there was no pulmonary stenosis.
In our study, a statistically significant difference was found in TRV between the patient and control groups. The findings showed TRV to be 1.44 ± 0.81 m/s in the healthy control group and 2.91 ± 1.54 m/s in the patient group. The maximum TRV obtained from the healthy children was 2.2 m/s, and the minimum jet flow obtained from the children with PAH was 1.9 m/s. Considering the cutoff value for TRV to be 2.2 m/s, the sensitivity and specificity of TRV in distinguishing PAH patients were found to be 69, and 95 %, respectively. Our results are consistent with those of a recent study indicating that a strong correlation exists between TRV and AcTc and that PAPsystolic can be determined with AcTc independently of TRV [29]. Our study found a moderate negative correlation between TRV and AcTc before the pulmonary vasoreactivity test (r = −0.383, p = 0.001, 95 % CI = −0.657 to −0.019) and after the pulmonary vasoreactivity test (r = −0.492, p = 0.007, 95 % CI = −0.727 to −0.153).
Our study is the first study to demonstrate the correlation between AcTc and TRV in patients with CHD and PAH. Our results show that information on pulmonary hemodynamics can be provided for a greater proportion of patients with PAH by AcTc and other measurements of the pulmonary artery flow velocity curve unless TRV can be detected.
Study Limitations
The most important limitation of our study was the small number of patients. This limitation resulted from the need to include patients with PAH and intracardiac shunts, to exclude patients who underwent medical treatment and intubation during cardiac catheterization, and to require concurrent catheterization and TTE. Another limitation was the absence of information about invasive pulmonary hemodynamics for the healthy control group. This limitation was because catheterization cannot be performed in these cases. Because it is not possible to obtain data about patients for whom cardiac catheterization is indicated but who have normal pulmonary hemodynamics, this limitation is considered to be an expected outcome of this study.
In conclusion, the measurement of pulmonary arterial flow velocity curve by means of TTE would be appropriate for assessing PAPmean, PAPsystolic, PVR, and pulmonary vasoreactivity in patients with CHD and PAH in the absence of a measurable TRV. We recommend the use of conventionally measured TRV, estimated PAPsystolic measurement, and AcTc, especially for patients with immeasurable TRV in clinical practice. The sensitivity and specificity associated with the concomitant use of AcTc and TRV to distinguish between PAH patients and healthy subjects were found to be 90 and 73 %, respectively. Therefore, this approach can be appropriate for determining the priority or urgency of cardiac catheterization when the implementation of invasive cardiac catheterization is not possible.
References
Badesch DB, Champion HC, Sanchez MA et al (2009) Diagnosis and assessment of pulmonary arterial hypertension. J Am Coll Cardiol 54:55–66
Barst RJ, Agnoletti G, Fraisse A et al (2010) Vasodilator testing with nitric oxide and/or oxygen in pediatric pulmonary hypertension. Pediatr Cardiol 31:598–606
Borgeson DD, Seward JB, Miller FA et al (1996) Frequency of Doppler measurable pulmonary artery pressures. J Am Soc Echocardiogr 9:832–837
Celermajer DS, Marwick T (2008) Echocardiographic and right heart catheterization techniques in patients with pulmonary arterial hypertension. Int J Cardiol 125:294–303
Cooper MJ, Tyndall M, Silverman NH (1988) Evaluation of the responsiveness of elevated pulmonary vascular resistance in children by Doppler echocardiography. J Am Coll Cardiol 12:470–475
Dabestani A, Mahan G, Gardin JM et al (1987) Evaluation of pulmonary artery pressure and resistance by pulsed Doppler echocardiography. Am J Cardiol 59:662–668
Donti A, Formigari R, Ragni L et al (2007) Pulmonary arterial hypertension in the pediatric age. J Cardiovasc Med 8:72–77
Ebeid MR, Ferrer PL, Robinson B et al (1996) Doppler echocardiographic evaluation of pulmonary vascular resistance in children with congenital heart disease. J Am Soc Echocardiogr 9:822–831
Feigenbaum H, Armstrong WF, Ryan T (2005) Feigenbaum’s echocardiography, 6th edn. Lippincott Williams & Wilkins, Philadelphia
Fisher MR, Forfia PR, Chamera E et al (2009) Accuracy of Doppler echocardiography in the hemodynamic assessment of pulmonary hypertension. Am J Respir Crit Care Med 179:615–621
Galie N, Hoeper MM, Humbert M et al (2009) Guidelines for the diagnosis and treatment of pulmonary hypertension. The Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS), endorsed by the International Society of Heart and Lung Transplantation (ISHLT). Eur Heart J 30:2493–2537
Gardin JM, Yoganathan A, McMillon S (1986) Pitfalls in Doppler pulmonary artery measurements: documentation in a flow model. Circulation 74:179
Hirschfeld S, Meyer R, Schwartz DC et al (1975) The echocardiographic assessment of pulmonary artery pressure and pulmonary vascular resistance. Circulation 52:642–650
Hoeper MM, Lee SH, Voswinckel R et al (2006) Complications of right heart catheterization procedures in patients with pulmonary hypertension in experienced centers. J Am Coll Cardiol 48:2546–2552
Houde C, Bohn DJ, Freedom RM (1993) Profile of paediatric patients with pulmonary hypertension judged by responsiveness to vasodilators. Br Heart J 70:461–468
Humpl T, Ingram SN (2010) Pulmonary vascular disease. In: Anderson R, Baker EJ, Penny D et al (eds) Pediatric cardiology, 3rd edn. Churchill Livingstone, Philadelphia, pp 1147–1161
Ivy D (2001) Diagnosis and treatment of severe pediatric pulmonary hypertension. Cardiol Rev 9:227–230
Jeon DS, Luo H, Iwami T et al (2002) The usefulness of a 10 % air-10 % blood-80 %saline mixture for contrast echocardiography: Doppler measurement of pulmonary artery systolic pressure. J Am Coll Cardiol 39:124–129
Kitabatake A, Inoue M, Asao M et al (1983) Noninvasive evaluation of pulmonary hypertension by a pulsed Doppler technique. Circulation 68:302–309
Kosturakis D, Goldberg SJ, Allen HD et al (1984) Doppler echocardiographic prediction of pulmonary arterial hypertension in congenital heart disease. Am J Cardiol 53:1110–1115
Lanzarini L, Fontana A, Campana C et al (2005) Two simple echo-Doppler measurements can accurately identify pulmonary hypertension in the large majority of patients with chronic heart failure. J Heart Lung Transplant 24:745–754
Limsuwan A, Khowsathit P (2009) Assessment of pulmonary vasoreactivity in children with pulmonary hypertension. Curr Opin Pediatr 21:594–599
Marshall HW, Swan HJ, Burchell HB et al (1961) Effect of breathing oxygen on pulmonary artery pressure and pulmonary vascular resistance in patients with ventricular septal defect. Circulation 23:241–252
McQuillan BM, Picard MH, Leavitt M et al (2001) Clinical correlates and reference intervals for pulmonary artery systolic pressure among echocardiographically normal subjects. Circulation 104:2797–2802
Milan A, Magnino C, Veglio F (2010) Echocardiographic indexes for the noninvasive evaluation of pulmonary hemodynamics. J Am Soc Echocardiogr 23:225–239
Nakahata Y, Hiraishi S, Oowada N et al (2009) Quantitative assessment of pulmonary vascular resistance and reactivity in children with pulmonary hypertension due to congenital heart disease using a noninvasive method: new Doppler-derived indexes. Pediatr Cardiol 30:232–239
Panidis IP, Russ I, Pliers GS (1986) Effect of sampling site: an.-overt of pulmonary artery blood flow by Doppler echocardiography. Am J Cardiol 5:1145–1147
Tahara M, Tanaka H, Nakao S et al (1981) Hemodynamic determinants of pulmonary valve motion during systole in experimental pulmonary hypertension. Circulation 64:1249
Yared K, Noseworthy P, Weyman AE et al (2011) Pulmonary artery acceleration time provides an accurate estimate of systolic pulmonary arterial pressure during transthoracic echocardiography. J Am Soc Echocardiogr 24:687–692
Yock PG, Popp RL (1984) Noninvasive estimation of right ventricular systolic pressure by Doppler ultrasound in patients with tricuspid regurgitation. Circulation 70:657–662
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cevik, A., Kula, S., Olgunturk, R. et al. Assessment of Pulmonary Arterial Hypertension and Vascular Resistance by Measurements of the Pulmonary Arterial Flow Velocity Curve in the Absence of a Measurable Tricuspid Regurgitant Velocity in Childhood Congenital Heart Disease. Pediatr Cardiol 34, 646–655 (2013). https://doi.org/10.1007/s00246-012-0520-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-012-0520-4