Abstract
Exercise creates a physiologic burden with recovery from such effort crucial to adaptation. Excess postexercise oxygen consumption (EPOC) refers to the body’s increased metabolic need after work. This investigation was designed to determine the role of near infrared spectroscopy (NIRS) in the description of exercise recovery in healthy controls (NL) and children with congenital heart disease (CHD). Subjects were recruited with exercise testing performed to exhaustion. Exercise time (EXT), heart rate (HR), and oxygen consumption (VO2) were measured. Four-site NIRS (brain, kidney, deltoid, and vastus lateralis) were measured during exercise and into recovery to establish trends. Fifty individuals were recruited for each group (NL = 26 boys and 24 girls; CHD = 33 boys and 17 girls). Significant differences existed between EXT, VO2, and peak HR (P < 0.01). NIRS values were examined at four distinct intervals: rest, peak work, and 2 and 5 min after exercise. Significant cerebral hyperemia was seen in children with CHD post exercise when compared to normal individuals in whom redistribution patterns were directed to somatic muscles. These identified trends support an immediate compensation of organ systems to re-establish homeostasis in peripheral beds through enhanced perfusion. Noninvasive NIRS monitoring helps delineate patterns of redistribution associated with EPOC in healthy adolescents and children with CHD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Exercise induces a physiologic burden resulting in the individual initially meeting demands followed by exhaustion leading to termination. Cardiopulmonary exercise testing (CPET) provides assessment of the integrative responses during this progression that are not adequately evaluated through the measurement of global or individual organ system function during resting conditions. This evaluation of a response to physiologic stress is clinically important because if failure of the system is to occur, it typically occurs while the system is under stress [27, 35].
The stress of exercise is not limited to just the duration of activity. Recovery from exercise-induced burden is equally important to the overall performance of the system. Excess postexercise oxygen consumption (EPOC) is the body’s increased metabolic need after exercise and refers to a physiologic payback of an oxygen debt at the tissue level. This debt reflects both the anaerobic metabolism of exercise and the respiratory, circulatory, hormonal, ionic, and thermal adjustments that occur in recovery [19]. There is an absence of a noninvasive real-time method of measuring regional tissue oxygenation to study this phenomenon in health and disease states.
Near-infrared spectroscopy (NIRS) techniques rely on application of the Beer–Lambert law for measurement of the concentration of a substance according to its absorption of light [25]. NIRS provides a noninvasive, continuous method to monitor regional tissue oxygenation (rSO2). NIRS is a venous-weighted oxyhemoglobin saturation that provides a window into regional oxygen supply–demand relations. We hypothesized that NIRS monitoring during ramping exercise will track the oxygen dynamics of exercise recovery in real time in both healthy children (NL) and children with congenital heart disease who had previously undergone palliation of single-ventricle anatomy (CHD).
Materials and Methods
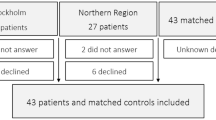
This study was initiated with funding assistance from the Children’s Research Institute, a division of Children’s Hospital and Health System, and the Medical College of Wisconsin, Milwaukee, WI, in addition to a Mend-a-Heart Foundation Grant and was approved by the Institutional Review Board of Children’s Hospital of Wisconsin. Patients were consented (IRB 07198 GC 708) for their participation. Fifty healthy subjects were recruited from individuals referred to the Exercise Physiology Laboratory at Children’s Hospital of Wisconsin for complaints of chest pain, palpitations, or shortness of breath. Resting echocardiogram (Siemens, Acuson, Mountain View, CA) and electrocardiogram (EKG) (GE Medical Systems, Milwaukee, WI) were performed before CPET to ensure there were no cardiac abnormalities, prolongation of the QT interval, pre-excitation, or frequent premature ectopic complexes. Fifty children with cyanotic congenital heart disease who had previously undergone palliation of single-ventricle anatomy were also recruited. Single-ventricle palliation included a three-stage approach consistent with our center’s protocol progressing from a Norwood procedure with creation of a neoaorta, Glenn anastomosis, and completion Fontan to establish cavopulmonary flow. In total, 23 single left ventricle and 27 single right ventricles were included for analysis. Diagnoses of the single-ventricle group are listed in Table 1. All patients were tested during an outpatient visit. No activity restrictions were given before testing, and standard pretest instructions were given.
Pulmonary Function Testing
Spirometry (Care Fusion, Yorba Linda, CA) was performed according to American Thoracic Society standards. Forced vital capacity (FVC), forced expiratory volume in 1 s (FEV1), peak expiratory flow rate, and maximal mid-expiratory flow (FEF25–75) were obtained. Values were expressed as a percent predicted for stature, body mass, and age [30].
NIRS
NIRS probes (Somanetics Invos Oximeter, Troy, MI) were placed on the forehead, para vertebral space, vastus lateralis, and deltoid muscle (rSO2C [brain], rSO2R [kidney], rSO2L [leg], and rSO2A [arm]), and rSO2 was recorded at 6-s intervals at rest, exercise, and throughout a 5-min recovery period to establish subacute trends associated with EPOC.
Exercise Testing
Exercise studies were performed using a standard Bruce protocol on a treadmill ergometer (GE Medical Systems, Milwaukee, WI) with incremental increases in speed and grade to voluntary exhaustion [6]. Heart rates (HRs) were obtained every minute with a 12-lead EKG, and blood pressure (BP) was obtained every 3 min or at times of arrhythmia or symptoms. Oxygen consumption (VO2) was determined (Care Fusion, Yorba Linda, CA) and computer recorded on a breath-by-breath basis. Maximal VO2 was recorded. A test was considered maximal if the peak HR exceeded 90% of predicted maximum, a plateau occurred in oxygen consumption that did not increase with increasing work, or the respiratory quotient (RQ) exceeded 1.10.
Postexercise Monitoring
Twelve-lead EKG and BP was recorded throughout 5 min of recovery or longer if an exaggeration in HR was observed or if patient symptoms required further evaluation. Spirometry was performed at 5 min after exercise and compared with baseline values. Postexercise decrease >15% in FEV1 or >20% in lower airway function was considered significant. Bronchodilator therapy (albuterol, 2 puffs metered dose inhaler by way of AeroChamber) was administered in those considered to have a significant postexercise decrease, and these patients were eliminated from further analysis.
Data Management
Descriptive statistics (mean, SD) were calculated for all physiologic parameters. Trends were plotted for regional oxygenation data, and polynomial smoothing of regional data was created for graphical representation. The mean percent change in rSO2 from baseline to time points peak, 2 min after exercise, and 5 min after exercise were computed for each individual. The mean change in rSO2 at these three time points for the NL and CHD groups were then compared using Student t test. Statistical analysis was performed using SPSS 11.5 statistical program (SPSS, Chicago, IL). All significant changes were reported at P < 0.05.
Results
Fifty NL (N = 26 boys and 24 girls age 7–21 years [average 15.4]) and 50 CHD (N = 33 boys and 17 girls age 7–23 years [average 11.5]) subjects were recruited. Resting pulmonary function studies were defined as normal in all healthy subjects with values >80% predicted in FVC, FEV1, and mid-expiratory flow (MEF25–75). The CHD group showed significant decreases in all indices of airway function when compared to the NL group. Most noticeable was the difference in FVC represented as a percent predicted (100.9 ± 18.4% vs. 69.7 ± 14.2%). Significant decreases in exercise (13.2 ± 2.5 vs. 9.3 ± 1.8 min; 120.2 ± 24.1% vs. 86.7 ± 18.3%), peak oxygen consumption (42.8 ± 9.7 vs. 34.3 ± 7.8 ml/kg/min), as well HR response (193.9 ± 9.8 vs. 163.7 ± 24.1 beats/min) were seen with the CHD compared with the NL group. Because a significant difference was noted in age between the CHD and NL groups (P < 0.01), reporting of data to age-related normative values maintained significance in the physiologic parameters as noted previously. Comparative data for all physiologic parameters are listed in Table 2.
Regional saturations at each site during exercise were plotted over time. In the NL group, trends in all somatic sites, as expected, showed progressive desaturation with an accelerated slope beginning after anaerobic threshold and continuing until exhaustion [31]. During recovery, patterns of regional saturations varied for exercising versus nonexercising muscle. Oxygenation in exercising muscle was associated with marked hyperemia during recovery to values well above baseline. The regional oxygenation trends in nonexercising somatic sites showed progressive desaturation, with an accelerated slope during the anaerobic phase, followed by rapid recovery with minimal or no postexercise hyperemia. In contrast, the CHD group had lower regional saturations in all somatic sites at rest with early and more progressive desaturation noted in response to maximal exercise (Figs. 1, 2, 3, 4). During recovery, patterns of regional saturations varied for exercising versus nonexercising muscles. In the CHD group, the significantly lower cerebral saturation at rest became exacerbated with exercise followed by a period of postexercise hyperemia directed toward re-establishment of cerebral saturations (Fig. 2). Despite significant desaturation in the exercise leg, there was sluggish recovery without marked hyperemia as noted in the NL group (Fig. 3).
Values were delineated for each somatic site at rest, peak exercise (ΔP), 2 min after exercise (Δ2), and 5 min after exercise (Δ5) for each group. Significant desaturation was noted at each somatic site at peak work compared with resting values with the greatest deviation from baseline being appreciated in the deltoid (−29%, −31%) and kidney (−31%, −35%) for both groups, respectively, suggesting global redistribution of flow away from these sites at peak work. Variations in saturation patterns were seen between the CHD and NL groups with regard to the vastus lateralis (exercising leg) and the cerebral bed (P < 0.01). These trends are listed in Table 3.
Discussion
The literature demonstrating the importance of this relatively new clinical tool, NIRS monitoring, continues to grow. The concept of multisite NIRS monitoring to characterize changes in integrative circulatory physiology has been previously described and has been extensively evaluated in the cerebral [13, 14, 22, 37, 39, 40], splanchnic [11, 29], and quasi-global circulations [20, 31, 34, 38]. NIRS can also be used to monitor cerebral and somatic oxygenation in various clinical situations and has been helpful in the detection of cerebrovascular dysfunction [21, 36]. This use of NIRS monitoring has also been employed in cardiac patients, demonstrating altered cardiovascular function in correlation with decreased cerebral saturation [16, 17, 26], as well as in both cerebral and somatic beds in patients with univentricle anatomy [33], cardiomyopathy [8], and neurocardiogenic instability [32].
CPET is used increasingly in children and adolescents in a wide spectrum of clinical applications for evaluation of undiagnosed exercise intolerance and for objective determination of functional capacity and impairment [1]. EPOC is the body’s increased metabolic need after physical work and refers to the physiologic payback of an oxygen debt. The use of NIRS during exercise to evaluate tissue oxygen economy has been validated. To date, the majority of these studies have measured regional oximetry in muscles, particularly in the vastus lateralis [7, 9] Progressive desaturation in somatic beds has also been described during incremental exercise on a bicycle ergometer [3]. Finally, anaerobic threshold has been shown to be accurately predicted through NIRS monitoring both at muscular and cerebral tissue beds [4, 31]. Despite considerable growth in NIRS-related exercise data, its utility as a descriptor of EPOC has not been previously explored, especially in patients with impaired cardiac status.
Performance of moderate to intense exertion results in stored carbohydrate depletion. Because oxygen demands exceed supply, the resultant acidosis results in marked physiologic changes. Recovery from such stress is measured by a return to homeostasis by the affected organs. This data highlights the distinct advantage of multisite NIRS monitoring in CPET because it provides real-time data of flow-to-demand coupling dynamics in different vascular beds with differing physiological control mechanisms. Although many measures have been used to describe single contributors to these exercise dynamics, such as endothelial function, cardiac output, etc., this single noninvasive tool now allows quantification of the complex interplay of these many factors. Multisite NIRS monitoring appears to enhance our understanding of EPOC through exaggeration of flow dynamics after exercise in specific somatic beds versus immediate return of homeostasis in others. The identified trends support an immediate compensation of organ systems to re-establish homeostasis through enhanced perfusion. Moreover, noninvasive NIRS monitoring helps delineate patterns of redistribution associated with EPOC, most notably in the super-compensation recognized in the muscle beds specifically involved in exercise. Specific representative variations in regional patterns of blood flow during incremental exercise are likely to emerge under different pathophysiologic conditions. The collection of data after exercise for this investigation was originally designed to allow for a return to baseline without expectation of significant hyperemia in the vastus lateralis. This overcompensation significantly correlated with the dramatic decrease in oxygen consumption measured using accepted gas analyzing techniques and supports the concept of a rapid lactacid payback as described in 1933 by Margaria–Hill [18]. Continuation of measurements to true baseline beyond our traditional 5-min recovery period would have allowed for assessment of the lactacid period of recovery and may have represented full recovery from exhaustive exertion with assumption of liver resynthesis of glycogen stores.
Multiple studies have identified exercise limitations in patients with single-ventricle anatomy, citing decreased exercise tolerance, including decreases in HR response, oxygen consumption, and exercise time [2, 5, 10, 12, 15, 23, 24, 28]. Moreover, age and pubertal status have been shown to magnify exercise abnormalities, especially in male patients in whom increased muscle associated with this period of growth results in even greater impairment with regard to oxygen delivery and use [28].
Fewer studies have examined the recovery of these patients from maximal exhaustive work. Ohuchi et al. in 2005 [23] noticed that there was delayed regression in HR, oxygen consumption, and systolic BP after exercise compared with individuals with normal cardiac anatomy. Lack of a pulmonary pump in patient with Fontan repair may limit venous return and result in alteration in venous compliance and tissue perfusion characteristics after exhaustive work. The use of cerebral saturation in patients with cardiac disease has been explored. There was a high correlation between left-ventricular systolic/diastolic function and baseline cerebral saturations with a magnified response in patients with exercise [26]. These findings correspond nicely with recent findings demonstrating a disproportionate decrease in cerebral saturations in response to exercise in single-ventricle patients compared with healthy controls [33]. However, this abnormal response to exercise was not translated into potential abnormalities in recovery. The postexercise cerebral hyperemia noted in our single-ventricle patients may further delineate these recovery abnormalities. Unlike normal subjects, in whom postexercise flow distribution is directed in a disproportionate way to the recovery muscles, single-ventricle patients showed redirection of postexercise blood flow to cerebral beds, resulting in comparatively decreased flow to the somatic regions of greatest need. This flow distribution pattern may delay overall recovery and prolong the regression of physiologic variables discussed previously.
Limitations of this investigation include a population that comprised of pediatric and adolescent patients. This may eliminate broader generalization to older populations in whom decreased muscle mass, altered metabolic process, and decreasing cardiopulmonary factors have been recognized as potentially affecting recovery from high-intensity endurance. Furthermore, in hindsight, continuation of measurements to true baseline beyond our traditional 5-min recovery period would have allowed for assessment of the lactacid period of recovery and may have represented full recovery from exhaustive exertion with assumption of liver resynthesis of glycogen stores. Finally, despite the variations in trends that were established, it is difficult to know the true clinical significance of these trends as they relates to the long-term prognosis of CHD patients. The absolute values presented for regional saturations, at any specific time point, have decreased value compared with the magnitude of change any value has in relation to a given stressor. In this investigation, we observed unique saturation trends that were represented as changes from baseline. These changes were distinctly different between the NL and CHD groups and provide valuable insight into the mechanism of recovery in individuals with single-ventricle physiology.
Conclusion
The use of multisite NIRS monitoring in assessing regional saturation patterns in healthy individuals as well as patients with repair of single-ventricle anatomy provides noninvasive, real-time assessment of perfusion trends associated with the response both during and after exhaustive exercise. Further application in individuals with various forms of physiology should provide additional insight to pathophysiologic mechanisms of exercise recovery in disease states.
References
Albouaini K, Egred M, Alahmar A, Wright DJ (2007) Cardiopulmonary exercise testing and its application. Postgrad Med J 83:675–682
Anderson PAW, Sleeper LA, Mahony L, Colan SD, Atz AM, Breitbart RE et al (2008) Contemporary outcomes after the Fontan procedure. A pediatric heart network multicenter study. J Am Coll Cardiol 52:85–98
Belardinelli R, Barstow TJ, Porszasz J, Wasserman K (1995) Changes in skeletal muscle oxygenation during incremental exercise measured with near infrared spectroscopy. Eur J Appl Physiol Occup Physiol 70:487–492
Bhambhani Y, Malik R, Mookerjee S (2007) Cerebral oxygenation decreases at exercise intensities above the respiratory compensation threshold. Respir Physiol Neurobiol 156:196–202
Brassard P, Bedard E, Jobin J, Rodes-Cabau J, Poirier P (2006) Exercise capacity and impact of exercise testing in patients after a Fontan procedure: a review. Can J Cardiol 22(6):489–495
Bruce RA (1971) Exercise testing of patients with coronary heart disease. Principles and normal standards for evaluation. Ann Clin Res 3:323–332
Costes F, Denis C, Roche F, Prieur F, Enjolras F, Barthelemy JC (1999) Age associated alteration of muscle oxygenation measured by near infrared spectroscopy during exercise. Arch Physiol Biochem 107:159–167
Danduran MJ, Rao RP, Frommelt PC, Ghanayem NS, Hoffman GM (2009) Near infrared spectroscopy monitoring during cardiopulmonary exercise testing in children with and without heart disease: Emerging new tool for investigation cardiovascular physiology in pediatric cardiology [abstr]. Cardiology, 12th annual update on pediatric and congenital cardiovascular disease: strategies to improve care through a multidisciplinary approach. Cardiol Young 19(Suppl S2):122–162
DeLorey DS, Kowalchuck JM, Paterson DH (2003) Relationship between pulmonary O2 uptake kinetics and muscle deoxygenation during moderate intensity exercise. J Appl Physiol 95:113–120
Durongpisitkul K, Driscoll DJ, Mahoney DW, Wollen PC, Mottram CD, Puga FJ et al (1997) Cardiorespiratory response to exercise after modified Fontan operation: determinants of performance. J Am Coll Cardiol 29(4):785–790
Fortune PM, Wagstaff M, Petros AJ (2001) Cerebro-splanchnic oxygenation ration (CSOR) using near infrared spectroscopy may be able to predict splanchnic ischemia in neonates. Intensive Care Med 27:1401–1407
Golstein BH, Connor CE, Gooding L, Rocchini AP (2010) Relation of systemic venous return, pulmonary vascular resistance, and diastolic dysfunction to exercise capacity in patients with single ventricle receiving Fontan palliation. Am J Cardiol 105:1169–1175
Hayashida M, Kin N, Tomioka T, Orii R, Sekiyama H, Usui H et al (2004) Cerebral ischemia during cardiac surgery in children detected by combined monitoring of BIS and near infrared spectroscopy. Br J Anaesth 92:662–669
Hoffman GM, Stuth EA, Jaquiss RD, Vanderwal PL, Staudt SR, Troshynski TJ et al (2004) Changes in cerebral and somatic oxygenation during stage 1 palliation of hypoplastic left heart syndrome using continuous regional cerebral perfusion. J Thorac Cardiovasc Surg 127:223–233
Khairy P, Poirier N, Mercier LA (2007) Univentricular heart. Circulation 115:800–812
Koike A, Nagayama O, Hoshimoto-Iwamoto M, Suzuki T, Tajima A, Uejima T et al (2008) Clinical significance of cerebral oxygenation during exercise in patients with coronary artery disease. Circ J 72(11):1852–1858
Madsen PL, Nielsen HB, Christiansen P (2000) Well being and cerebral oxygen saturation during acute heart failure in humans. Clin Physiol 20(2):158–164
Margaria R, Edwards HT, Hill DB (1933) The possible mechanism of contracting and paying the oxygen debt and the role of lactic acid in muscular contraction. Am J Physiol 106:687–714
McArdle WD, Katch FL, Katch VL (1991) Energy transfer in exercise. In: Exercise physiology: energy, nutrition and human performance, 3rd edn. Lea and Febiger, Philadelphia, pp 133–139
Nagdyman N, Fleck T, Barth S, Abdul-Khaliq H, Stiller B, Ewert P et al (2004) Relation of cerebral tissue oxygenation index to central venous oxygen saturation in children. Intensive Care Med 30:468–471
Nollert G, Mohnle P, Tassani-Prell P, Uttner I, Borasio GD, Schmoeckel M et al (1995) Postoperative neuropsychological dysfunction and cerebral oxygenation during cardiac surgery. Thorac Cardiovasc Surg 43:260–264
Nollert G, Jonas RA, Reichart B (2000) Optimizing cerebral oxygenation during cardiac surgery: a review of experimental and clinical investigations with near infrared spectrophotometry. Thorac Cardiovasc Surg 48:247–253
Ohuchi H, Hamamichi Y, Hayashi T, Watanabe T, Yamada O, Yagihara T et al (2005) Post exercise heart rate, blood pressure and oxygen uptake dynamics in pediatric patients with Fontan circulation. Comparison with patients after right ventricular outflow tract reconstruction. Int J Cardiol 101:129–136
Ohuchi H, Hayashi T, Yamada O, Echigo S (2006) Change in plasma volume during peak exercise in patients with cyanotic congenital heart disease after definitive operation. Int J Cardiol 108:216–223
Owen-Reece H, Smith M, Elwell CE, Goldstone JC (1990) Near infrared spectroscopy. Br J Anaesth 82:418–426
Paquet C, Deschamps A, Denault AY, Couture P, Carrier M, Babin D et al (2008) Baseline regional cerebral oxygen saturation correlates with left ventricular systolic and diastolic function. J Cardiothorac Vasc Anesth 22(6):840–846
Paridon SM, Alpert BS, Boas SR, Cabrera ME, Caldarera LL, Daniels SR et al (2007) American Heart Association Council on Cardiovascular Disease in the Young. Committee on Atherosclerosis, Hypertension, and Obesity in Youth. Clinical stress testing in the pediatric age group: a statement from the American Heart Association Council on Cardiovascular Disease in the Young. Committee on Atherosclerosis, Hypertension, and Obesity in Youth. Circulation 113:1905–1920
Paridon AM, Mitchell PD, Colan SD, Williams RV, Blaufox A, Li JS et al (2008) A cross sectional study of exercise performance during the first two decades of life after the Fontan operation. J Am Coll Cardiol 52:99–107
Petros AJ, Heys R, Tasker RC, Fortune PM, Roberts I, Kiely E (1999) Near infrared spectroscopy can detect changes in splanchnic oxygen delivery in neonates during apnoeic episodes. Eur J Pediatr 158:173–174
Polgar G, Promadhat V (1971) Standards in pulmonary function tests. In: Polgar G (ed) Pulmonary function testing in children; techniques and standard. Saunders, Philadelphia, pp 254–260
Rao RP, Danduran MJ, Frommelt PC, Ghanayem NS, Berger S, Simpson PM et al (2009) Measurement of regional tissue bed venous weighted oximetric trends during exercise by near infrared spectroscopy. Pediatr Cardiol 30:465–471
Rao RP, Danduran MJ, Dixon JE, Frommelt PC, Berger S, Zangwill SD (2010) Near infrared spectroscopy: guided tilt table testing for syncope. Pediatr Cardiol 31(5):674–679
Rao RP, Danduran MJ, Hoffman GM, Ghanayem NS, Berger S, Frommelt PC (2010) Cerebral hemodynamics in the presence of decreased systemic venous compliance in patients with Fontan physiology may limit anaerobic exercise capacity. Pediatr Cardiol 31(2):208–214
Schulz G, Weiss M, Bauersfeld U, Teller J, Haensse D, Bucher HU et al (2002) Liver tissue oxygenation as measured by near-infrared spectroscopy in the critically ill child in correlation with central venous oxygen saturation. Intensive Care Med 28:184–189
Task ERS, Palange FP, Ward SA, Carlsen KH, Casaburi R, Gallagher CG et al (2007) Recommendations on the use of exercise testing in clinical practice. Eur Respir J 29:185–209
Tsuji M, Saul JP, du Plessis A, Eichenwald E, Sobh J, Crocker R et al (2000) Cerebral intravascular oxygenation correlates with mean arterial pressure in critically ill premature infants. Pediatrics 106:625–632
Watzman HM, Kurth CD, Montenegro LM, Rome J, Steven JM, Nicolson SC (2000) Arterial and venous contributions to near-infrared cerebral oximetry. Anesthesiology 93:947–953
Weiss M, Dullenkopf A, Kolarova A, Schulz G, Frey B, Baenziger O (2005) Near-infrared spectroscopic cerebral oxygenation reading in neonates and infants is associated with central venous oxygen saturation. Paediatr Anaesth 15:102–109
Wyatt JS, Cope M, Delpy DT, Wray S, Reynolds EO (1986) Quantification of cerebral oxygenation and haemodynamics in sick newborn infants by near infrared spectrophotometry. Lancet 2(8515):1063–1066
Yoshitani K, Kawaguchi M, Iwata M, Sasaoka N, Inoue S, Kurumatani N et al (2005) Comparison of changes in jugular venous bulb oxygen saturation and cerebral oxygen saturation during variations of haemoglobin concentration under propofol and sevoflurane anaesthesia. Br J Anaesth 94:341–346
Acknowledgments
This research was funded by a Pilot Innovative Research Award, Children’s Research Institute, Children’s Health System, Milwaukee, WI, and The Mend-a-Heart Foundation, Clarendon Hills, IL.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Danduran, M.J., Dixon, J.E. & Rao, R.P. Near Infrared Spectroscopy Describes Physiologic Payback Associated With Excess Postexercise Oxygen Consumption in Healthy Controls and Children With Complex Congenital Heart Disease. Pediatr Cardiol 33, 95–102 (2012). https://doi.org/10.1007/s00246-011-0097-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-011-0097-3