Abstract
Impacted stones typically make it difficult to perform ureteroscopic lithotripsy (URSL), so it is useful to preoperatively predict such impaction. We focused on CT attenuation values of the ureter above and below the stone (‘HU above’ and ‘HU below’) and calculated their ratio (HAB ratio; HU above/HU below ratio). The aim was to investigate whether HAB ratio could predict impacted stones preoperatively. Between 2011 and 2019, 171 patients from our hospital that had URSL for ureteral stones with pretreatment non-contrast computed tomography (NCCT) were retrospectively identified. Ureteral wall thickness (UWT), ureteral wall volume (UWV) and HAB ratio (‘HU above’ divided by ‘HU below’) were recorded. Impacted stones were defined as fixed stones that did not move by means of ureteroscopic manipulation or water pressure. Of the 171 procedures, 46 (27%) involved patients with impacted stones. Comparing patient characteristics and stone parameters according to impaction status, factors with significant difference included grade of hydronephrosis, UWT, and HAB ratio (all P < 0.01). Multivariate analysis indicated that significant independent predictors of impacted stones were thicker UWT and lower HAB ratio (all P < 0.01). HAB ratio was a significant preoperative predictor of stone impaction in patients undergoing URSL for ureteral stones. HAB ratio may be informative for selecting the treatment and preoperative preparations.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Impacted ureteral stones are those that stay in the same place for long time, although this definition has not been agreed upon. The presence of impacted stones is extremely important information in ureteral stone treatment. Low rate of shock wave lithotripsy (SWL) success has been shown in patients with impacted ureteral stones because of ureteral epithelial edema and hypertrophy [1,2,3]. SWL should therefore be avoided as much as possible for patients with impacted stones. On the other hand, ureteroscopic lithotripsy (URSL) is often complicated in patients with impacted stones, as clear visualization cannot be maintained and the fixation of ureteral stones need to be removed. Impacted stones may also increase the intraoperative rate of complications (including ureteral perforation and avulsion), and decrease the stone-free rate (SFR) [4,5,6]. For these reasons, a means of predicting stone impaction is urgently required for treatment selection and adequate preoperative preparation.
Many studies have been conducted to predict stone impaction based on preoperative factors obtained from non-contrast computed tomography (NCCT) [4], and more recently, ureteral wall-related factors have attracted attention [7, 8]. Ureteral wall thickness (UWT) assessed by NCCT where there are ureteral stones has been reported as the representative ureteral wall-related factor for predicting stone impaction [8]. Furthermore, CT attenuation of the ureter above and below the ureteral stone was recently reported to be useful for predicting stone impaction [9].
The definition of impacted stones has varied in previous reports, but intraoperative ureteroscopic findings can determine whether ureteral stones are actually impacted. Impacted stones were defined in the current study as those that could not be moved by means of ureteroscopic procedure or irrigation pressure. To our knowledge, no studies have previously defined impacted stones from intraoperative ureteroscopic findings and evaluated whether ureteral wall-related factors, including CT attenuation of the ureter above and below the ureteral stone, can predict impacted stones. We therefore aimed in this study to elucidate what can preoperatively predict stone impaction.
Materials and methods
Patients
We retrospectively reviewed the records of 226 consecutive patients who underwent URSL at Wakayama Medical University for ureteral stones shown on preoperative NCCT between January 2011 and April 2019. Of these 226 patients, 55 were excluded because of multiple ureteral stones, previous treatment, or insufficient data, and the remaining 171 patients were enrolled in this study. Institutional review board approval was received. All participants gave written informed consent prior to this study.
Surgical procedures
All URSL procedures were performed in lithotomy position using a 7.5 Fr semi-rigid ureteroscope (Karl Strorz, Tuttlingen, Germany), and/or flexible ureteroscopy (URF-P6 or P7, OLYMPUS, Tokyo, Japan) under general anesthesia. First, to observe the inside of the ureter, a semi-rigid ureteroscope was inserted from the ureteral orifice to the stone. Subsequently, a ureteral access sheath (Cook Medical, Bloomington, IN, size; 9.5/11.5 Fr, 12/14 Fr and Boston Scientific, Marlborough, MA, size; 11/13 Fr) was placed under fluoroscopic guidance in patients with proximal or middle ureteral stones that could not be disintegrated using the semi-rigid ureteroscope. A safety guidewire was placed under fluoroscopic guidance in the case of impacted stones based on intraoperative endoscopic findings. A 270 µm Medilas H Solvo holmium laser (Dornier, Lindau, Germany) with short/long pulse width setting and an energy level of 0.6–1.2 J and a rate of 8–10 Hz was used to disintegrate the target stone. A 1.5 Fr N-Circle nitinol tip-less basket (Cook Medical) was used for stone removal. Finally, an indwelling ureteral stent was placed under fluoroscopic guidance in most patients, with the exception of those that did not use ureteral access sheath, for 1–2 weeks and removed as an outpatient after hospital discharge. Procedures were all performed by or observed by expert surgeons.
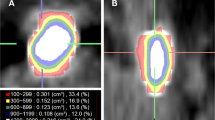
Data collection
Patient demographics, clinical data and surgical outcomes were retrospectively collected from patient medical records, and impacted stone presence was evaluated from operative videos. Patient demographics included patient age, sex, body mass index (BMI) and Eastern Cooperative Oncology Group performance status. Clinical data included stone size, stone volume, mean stone density (MSD), UWT, ureteral wall volume (UWV), stone location (proximal, middle or distal ureter), grade of hydronephrosis, CT attenuation of the ureter above and below the stone (‘HU above’ and ‘HU below’) and presence of preoperative stenting. All patients underwent preoperative non-contrast computed tomography (NCCT) before placement of a ureteral stent with a 5–10 mm thickness slice (LightSpeed 64-slice multidetector helical CT scanner, GE Healthcare Technologies, Waukesha, WI). The following settings were adopted: peak voltage 120kVp, tube current automatic exposure control setting (noise index 12), detector coverage 40 mm, gantry rotation time 0.5 s, beam pitch 0.984. All CT images were reconstructed with filtered back projection. UWT was defined as the maximum thickness of the ureteral wall in the maximum stone diameter on axial NCCT image. UWV was defined as the volume of the ureteral wall from the upper edge to the lower edge of the stone [10]. UWV was evaluated using Aquarius iNtuition Viewer (TeraRecon Inc., Durham, NC) as well as stone volume and MSD. Stones were defined as lesions ≥ 100 Hounsfield unit (HU), as previously described [11]. ‘HU above’ and ‘HU below’ were measured by visually placing ROI at the center of the ureter of the one slice proximal and distal to the stone on axial NCCT image, respectively (the size of ROI was 0.005 cm2) (Fig. 1) [9]. HAB ratio, the ratio of ‘HU above’ and ‘HU below’, was calculated as ‘HU above’ divided by ‘HU below’ (Fig. 2). All NCCT measurements were via the abdominal window by experienced urologists blinded to the outcome of this study and the presence of impacted stones. Surgical outcomes included operation time, intraoperative complication rate (ureteral injury), and SFR. Our definition of stone-free status was the absence of residual stones ≥ 4 mm based on NCCT or kidney-ureter-bladder X-ray films within three months after the operation. Impacted stones were defined as fixed stones that did not move by means of ureteroscopic manipulation or irrigation pressure.
The measurement method of ‘HU above’ and ‘HU below’ from NCCT image. A The CT slice locations where ‘HU above’ and ‘HU below’ were measured were shown in coronal NCCT image. ‘HU above’ and ‘HU below’ were measured from the first slice proximal and distal to the stone. B ‘HU above’ was measured at the center of the ureter on axial image (the size of ROI: 0.005cm2). C ‘HU below’ was measured at the center of the ureter on axial image (the size of ROI: 0.005 cm2)
Statistical analysis
Patient demographics, clinical data and surgical outcomes were compared with Chi square tests or Mann–Whitney U tests according to impaction status. We performed univariate and multivariate logistic regression analyses to identify predictive factors associated with the presence of impacted stones. In logistic regression analyses, UWT and HAB ratio were analyzed as continuous variables. Statistical analyses were all performed using JMP Pro 13 (SAS Institute, Cary, NC) and P < 0.05 was considered statistically significant.
Results
Overall, included in this study were 171 patients (59 female, 112 male). Of the 171 procedures, 46 (27%) involved patients with impacted stones. Table 1 compares patient characteristics, surgical outcomes and stone parameters between the impacted and non-impacted groups. UWT was significantly thicker in the impacted than in the non-impacted group (4.3 mm vs 3.3 mm, P < 0.01), and UWV was also significantly larger in the impacted group (975 mm3 vs 819 mm3, P = 0.04). Regarding grade of hydronephrosis, the rate of high grade was significantly higher in the impacted group than in the non-impacted group (P < 0.01). Furthermore, ‘HU above’ was significantly lower (12 HU vs 16 HU, P = 0.01) and HAB ratio was significantly lower (0.45 vs 0.68, P < 0.01) in the impacted group than in the non-impacted group. Similarly, operation time was found to be significantly longer (84 min vs 64 min, P < 0.01) and the rate of ureteral injury was significantly higher (17.4% vs 2.4%, P < 0.01) in the impacted group than in the non-impacted group.
The results of univariate and multivariate logistic regression analyses of various preoperative factors that predict the presence of impacted stone are shown in Table 2. On univariate analysis, thicker UWT, grade of hydronephrosis ≥ 3, and lower HAB ratio were associated with the presence of impacted stone (all P < 0.01). On multivariate analysis, thicker UWT, grade of hydronephrosis ≥ 3, and lower HAB ratio were the significant independent predictors for the presence of impacted stone (all P < 0.01).
The association between the rate of the patients with impacted stones and the number of predictive factors is shown in Fig. 3; UWT ≥ 4.0 mm, grade of hydronephrosis ≥ 3 and HAB ratio ≤ 0.3. The optimal cutoff values of these risk factors were determined by ROC curve analyses. The rate of patients with impacted stones when the number of risk factors were 0, 1, 2, 3 were 6.5%, 23.3%, 41.5%, and 81.8%, respectively. As the number of risk factors increased, the rate of patients with impacted stones also increased significantly (P < 0.01).
Discussion
We investigated preoperative factors to predict stone impaction that was defined by intraoperative uteroscopic findings. High UWT, high grade of hydronephrosis and low HAB ratio were each independent preoperative factors that predicted stone impaction. Additionally, the higher the number of these factors, the greater the risk of impacted stones.
In the case of impacted stones, the stone remains in the same position in the ureter, causing chronic inflammation of the mucosa, fibrosis of the interstitium, and thickening of the uroepithelium, resulting in mucosal edema, polyps, and stone adherence [1, 12]. When URSL is performed, these changes in the ureteral wall often make the operative procedures difficult because of the inability to maintain clear visualization and the need to remove stones from ureteral mucosa. In a previous study, operation time was longer, SFR was lower, and intraoperative complications rate was higher in the patients with impacted stones than in those without impacted stones (all P < 0.001) [4]. Similarly, in this study, operation time was found to be longer and the rate of ureteral injury was higher in the impacted group than in the non-impacted group (all P < 0.01).
Several definitions of impacted stones have been reported, but no single definition has yet been established. One definition is the failed initial attempt to pass a guidewire or catheter through the stone [8]. Although this definition has been the most cited, it is difficult to evaluate whether a guidewire or catheter could be passed through the stone retrospectively, and it cannot be assessed in patients undergoing SWL without ureteroscopic procedures. A second definition is when stones stagnate without moving in the ureter for more than two months [5, 13]. In a previous study, the period from first diagnosis or onset of symptoms to the date of treatment was calculated, but it is difficult to assess the exact start date. A third definition is when the ureter distal to the stone is not contrasted on computed tomographic urography (CTU) or intravenous urography (IVU) [6]. However, CTU and IVU may not be possible in all patients because of renal dysfunction or allergies [14]. Previous definitions thus have issues and do not always accurately reflect the actual impacted stones that are difficult to treat. In the present study, we defined impacted stones based on ureteroscopic findings to accurately extract ureteral stones that are difficult to treat with URSL.
UWT, ureteral wall thickness at the stone site, was first reported as a predictive factor of SWL success [7]. It was hypothesized that UWT would be increased in impacted stones because of the formation of mucosal edema and polyps at the stone site, and they reported that high UWT was an independent factor predicting stone impaction (odds ratio [OR]: 5.43, P < 0.01, optimal cut off value: 3.49 mm) [8]. Similarly, in the present study, UWT was an independent predictor of stone impaction, and the optimal cut off value was also close (OR: 1.20, P < 0.01, optimal cut off value: 4.0 mm). UWV (volume of the ureteral wall at the stone site) was previously reported to be a better predictive factor of treatment success for SWL than UWT [10], but no previous reports have evaluated UWV in URSL. In the present study, UWV was not a significant factor in predicting stone impaction (OR: 1.00, P = 0.06).
CT attenuation of the ureter above and below ureteral stones, was shown in another recent study to be a novel predictor of stone impaction (‘HU above’; OR: 0.92, P = 0.000, ‘HU below’; OR: 1.13, P = 0.000) [9]. ‘HU below’ (CT attenuation of the ureter below ureteral stones) was reported to be significantly higher, while ‘HU above’ (CT attenuation of the ureter above ureteral stones) was reported to be lower in impacted stones. The cause of these results has been unclear. However, ‘HU above’ tended to have liquid density (lower density) because of hydronephrosis, while ‘HU below’ tended to have tissue density (high density) because of ureteral mucosal edema and inflammatory changes. HAB ratio, which was calculated as ‘HU above’ divided by ‘HU below’, was thus expected to be lower in patients with impacted stones because of hydronephrosis, ureteral mucosal edema and inflammatory changes, so we therefore focused on HAB ratio. Ozbir et al. reported that the area under curve (AUC) of the ratio of ‘HU above’ and ‘HU below’ was equivalent to that of UWT in terms of predicting stone impaction [9]. In the present study, HAB ratio was an independent predictor of stone impaction (OR: 0.26, P < 0.01, optimal cut off value: 0.3).
The grade of hydronephrosis is expected to be high in patients with impacted stones because of poor urinary passage. Hydronephrosis was previously reported to be an independent predictor of stone impaction [9], which was consistent with the results of this study.
Figure 3 shows the association between the rate of the patients with impacted stones and the number of predictors (UWT ≥ 4.0 mm, grade of hydronephrosis ≥ 3 and HAB ratio ≤ 0.3). When the number of risk factors was 0, 1, 2, and 3, the rate of the patients with impacted stones was 6.5%, 23.3%, 41.5%, and 81.8%, respectively. These results suggest that preoperative factors might be used to predict stone impaction.
This study has a small number of limitations. First, it was retrospective and used a comparatively small cohort. Second, CT slice thickness was not unified. Consequently, there might be some small errors in HAB ratio because ‘HU above’ and ‘HU below’ were measured in the one slice proximal and distal to the stone. An additional problem with this measurement method was that slight shift in the location of ROI might cause errors in CT attenuation. Demonstration of the reproducibility of this measurement method is therefore necessary. Third, the duration between the date of symptom and the date of treatment could not be collected. Despite these limitations, UWT, HAB ratio and grade of hydronephrosis were shown to be novel preoperative predictors of stone impaction in which definition was based on ureteroscopic findings. We believe that this information will aid the selection of the treatment of impacted stones.
Conclusion
HAB ratio is a novel predictor of stone impaction in patients with ureteral stones undergoing URSL. It may be useful for selecting the treatment and preoperative preparations.
Abbreviations
- AUC:
-
Area under curve
- BMI:
-
Body mass index
- CTU:
-
Computed tomographic urography
- HAB ratio:
-
HU above/HU below ratio
- HU:
-
Hounsfield unit
- IVU:
-
Intravenous urography
- MSD:
-
Mean stone density
- NCCT:
-
Non-contrast computed tomography
- OR:
-
Odds ratio
- SFR:
-
Stone-free rate
- SWL:
-
Shock wave lithotripsy
- URSL:
-
Ureteroscopic lithotripsy
- UWT:
-
Ureteral wall thickness
- UWV:
-
Ureteral wall volume
References
Morgentaler A, Bridge SS, Dretler SP (1990) Management of the impacted ureteral calculus. J Urol 143:263–266
Mueller SC, Wilbert D, Thueroff JW, Alken P (1986) Extracorporeal shock wave lithotripsy of ureteral stones: clinical experience and experimental findings. J Urol 135:831–834
Chaussy CG, Fuchs GJ (1989) Current state and future developments of noninvasive treatment of human urinary stones with extracorporeal shock wave lithotripsy. J Urol 141:782–789
Legemate JD, Wijnstok NJ, Matsuda T, Strijbos W, Erdogru T, Roth B, Kinoshita H, Palacios-Ramos J, Scarpa RM, de la Rosette JJ (2017) Characteristics and outcomes of ureteroscopic treatment in 2650 patients with impacted ureteral stones. World J Urol 35:1497–1506
Roberts WW, Cadeddu JA, Micali S, Kavoussi LR, Moore RG (1998) Ureteral stricture formation after removal of impacted calculi. J Urol 159:723–726
Degirmenci T, Gunlusoy B, Kozacioglu Z, Arslan M, Kara C, Koras O, Minareci S (2012) Outcomes of ureteroscopy for the management of impacted ureteral calculi with different localizations. Urology 80:811–815
Sarica K, Kafkasli A, Yazici O, Cetinel AC, Demirkol MK, Tuncer M, Sahin C, Eryildrim B (2015) Ureteral wall thickness at the impacted ureteral stone site: a critical predictor for success rates after SWL. Urolithiasis 43:83–88
Yoshida T, Inoue T, Omura N, Okada S, Hamamoto S, Kinoshita H, Matsuda T (2017) Ureteral wall thickness as a preoperative indicator of impacted stones in patients with ureteral stones undergoing ureteroscopic lithotripsy. Urology 106:45–49
Ozbir S, Can O, Atalay HA, Canat HL, Cakir SS, Otunctemur A (2019) Formula for predicting the impaction of ureteral stones. Urolithiasis 48(4):353–360. https://doi.org/10.1007/s00240-019-01152-y
Yamashita S, Kohjimoto Y, Iguchi T, Nishizawa S, Kikkawa K, Hara I (2020) Ureteral wall volume at ureteral stone site is a critical predictor for shock wave lithotripsy outcomes: comparison with ureteral wall thickness and area. Urolithiasis 48(4):361–368. https://doi.org/10.1007/s00240-019-01154-w
Yamashita S, Kohjimoto Y, Iwahashi Y, Iguchi T, Iba A, Nishizawa S, Hara I (2019) Three-dimensional mean stone density measurement is superior for predicting extracorporeal shock wave lithotripsy success. Int J Urol 26:185–191
Dretler SP, Young RH (1993) Stone granuloma: a cause of ureteral stricture. J Urol 150:1800–1802
Deliveliotis C, Chrisofos M, Albanis S, Serafetinides E, Varkarakis J, Protogerou V (2003) Management and follow-up of impacted ureteral stones. Urol Int 70:269–272
Baerlocher MO, Asch M, Myers A (2010) Allergic-type reactions to radiographic contrast media. CMAJ 182:1328
Acknowledgements
This document was proof-read and edited by Benjamin Phillis at the Clinical Study Support Center, Wakayama Medical University. The authors are grateful to Takashi Nishiyama, Radiological technologist at Wakayama Medical University, for his help in manuscript writing.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
RD wrote the main manuscript text and prepared figures 1-3 and table 1-2. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures were carried out in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration. This study was approved by Wakayama Medical University Ethics Committee (No.3487).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Deguchi, R., Yamashita, S., Iwahashi, Y. et al. The ratio of CT attenuation values of the ureter above/below ureteral stones is a useful preoperative factor for predicting impacted ureteral stones. Urolithiasis 50, 643–649 (2022). https://doi.org/10.1007/s00240-022-01354-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00240-022-01354-x