Abstract
The objective of this study is to evaluate the average radiation exposure in children with renal stones before SWL treatment. Mean radiation exposure values were evaluated in 110 children before SWL treatment. While some children referred to the emergency department (ED) with colic pain, remaining cases referred to outpatient department (OD). Although low-dose NCCT was performed in ED; KUB and abdominal sonography were first performed in other cases referring to OD where CT has been applied if needed. The type of imaging modality used and the mean radiation exposure were evaluated and comparatively evaluated with respect to the department referred, patient as well as stone related parameters. 49 children referred to ED and 61 children referred to OD. Mean stone size was 7.24 ± 0.29 mm. 62 cases had opaque stones. Mean radiation exposure values were higher in children referring to ED than the other cases. However, there was no significant difference between the two groups regarding the mean number of KUB, IVU and sonographic evaluation performed prior to SWL management. There was a significant correlation between the mean radiation exposure and the stone size as well degree of hydonephrosis in a positive manner. Although a significant correlation was present between the mean radiation exposure and stone opacity in a negative manner; there was no correlation with respect to the other related parameters. Unnecessary use of X-ray based imaging modalities in children could be effectively avoided using KUB and US combination beginning from the diagnostic phase of stone disease.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Although the incidence of pediatric urolithiasis is reported to be 1–5%, the disease is still an important healthcare problem particularly in developing countries [1]. Due to the high recurrence rates associated with metabolic abnormalities and changes in the quality of life, stone disease represents a unique diagnostic and therapeutic challenge in this specific population [2,3,4,5].
Early diagnosis and rational management of urinary stones have a pivotal role particularly in this specific population and as the first but highly important step proper imaging of these cases include a true assessment with maximum sensitivity and specificity associated with minimal risk of radiation exposure. Similar to adult population, a variety of imaging modalities namely sonography, noncontrast computed tomography (NCCT), intravenous urography (IVU) as well as plain kidney-ureter-bladder (KUB) radiographs are being performed in kids with certain benefits and limitations [6].
Unlike the data regarding the incidence and the outcomes of minimally invasive surgical treatment modalities, very limited data focusing on the quantification of the radiation exposure prior to the stone management in these cases could be derived from the literature. Regarding the type as well as the quantity of the imaging modality used children may undergo excessive radiation exposure during both the initial diagnostic and also follow-up evaluation period. When compared with adults, use of medical radiation in pediatric population for any reason is an important consideration due to the relatively longer remaining lifespan and more radiosensitive tissues making them particularly vulnerable to the long-term effects of ionizing radiation [7].
In light of these facts, collaborative efforts of clinicians, radiation physicists, public health officials and industry have promoted the ALARA (As low as reasonably achievable) principle to limit the radiation exposure as much as possible particularly in the pediatric population [8,9,10,11].
Regarding the diagnosis as well as the follow-up of stones in children; although ultrasonography (USG) has been commonly performed as the least non-invasive and safest tool, similar to the adult cases (non-contrast computerized tomography) NCCT has also been increasingly performed particularly for acute evaluation of pediatric urolithiasis. Radiologists tend to perform NCCT based examination more commonly due to its high sensitivity in the quick diagnosis of both renal and ureteral stones particularly in the emergency department (ED) setting.
In this present study, we aimed to evaluate the average radiation exposure values in children during the preparation phase for shock wave lithotripsy (SWL) treatment of renal stones.
Patients and methods
The departmental files of 110 children (63 boys and 47 girls; M/F: 1.34) undergoing SWL for solitary renal stones between April 2014 and April 2016 have been evaluated in a retrospective manner. The mean radiation exposure values during the preparation phase for SWL treatment along with the patient and stone related parameters were derived from these files.
Depending on the department of first referral children were divided into two groups namely cases referring to the pediatric emergency department (ED) with colic pain and/or hematuria (Group 1) and cases referring to outpatient department (OD) with vague symptoms of abdominal pain and recurrent urinary tract infection (UTI) (Group 2).
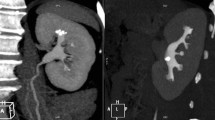
In addition to the detailed patient history, a thorough physical examination and complete blood–urine tests have been performed. Regarding the radiological assessment again although a low-dose NCCT was the preferred imaging modality in children referring in an emergency setting with colic pain, KUB and abdominal sonography were the most commonly performed means in other cases referring to outpatient department where NCCT has been applied if needed. UTI has been treated with appropriate antibiotic regimen in all cases before SWL treatment. All these evaluation and management procedures have been performed within the frame of the algorithm used in our department for kids referring with suspected urinary stones (Fig. 1).
While abdominal sonography evaluation was performed with Mindray DC-7 system (Mindray Medical Technologies, Shenzhen, China), low-dose non-contrast CT examination was performed with GE Hi-Speed Advantage helical scanners (GE Medical Systems, Milwaukee, WI). IVU and KUB roentgenograms were performed using a Siemens Healthcare 960 × 720 X-ray scanner system.
In addition to the stone related factors (location, size and Hounsfield unit (HU)), presence and the degree of hydronephrosis were also assessed in all children. Following the evaluation of the type of imaging modality used and the mean exposure to radiation in each case, mean radiation exposure values were comparatively evaluated with respect to the department referred, patient as well as stone related parameters mentioned above.
Last but not least, as the most important parameter of our study estimated radiation exposure values in children has also been calculated for each imaging modality as follows:
With respect to the protocol applied for CT evaluation included parameters as peak tube voltage of 100 kVp, minimum tube current (mA) of 75 mA, maximum mA of 240 mA, noise index (NI) of 23, exposure time of 0.8 s, volume CT dose index of 2.8 mGy, dose-length product of 115 mGy × cm. The organ doses have been estimated using Monte Carlo methods [12, 13]. The effective dose was calculated by summing organ doses adapted by the tissue-weighting factors provided in the International Commission on Radiological Protection (ICRP) Publication 103 [14]. For IVU evaluation; effective dose was calculated using the patient entrance skin dose, radiation field size, an effective dose conversion factor and a normalized energy-imparted conversion factor for an abdominal radiographic projection [15]. Finally the effective dose for roentgenograms was calculated using the PC-based Monte Carlo program (PCXMC) (version 2.0) (STUK—Radiation and Nuclear Safety Authority, Helsinki, Finland).
Data obtained in our study are presented as mean ± standard error of mean. Using prism 5.0 (GraphPad Software, San Diego, CA); Mann–Whitney test and Spearman tests were used to evaluate both the overall statistical significance and also the correlation between subgroups. A p value of < 0.05 was considered to be significant.
Results
A total of 110 pediatric cases (63 boys and 47 girls; M/F: 1.34) with solitary renal calculi have been evaluated and treated with SWL in our department between April 2014 and April 2016. Of all the children treated while 49 cases referred to ED with colic pain (44.5%), the remaining 61 cases were examined in OD (55.5%) with symptoms of vague abdominal pain, recurrent UTI and hematuria.
Patient age varied between 1 and 16 years with a mean value of 5.84 ± 0.38 years. Mean stone size was 7.24 ± 0.29 mm (4–21 mm) and the mean HU value was 596.3 ± 38.28 (234–1076). 70 Children had dilated renal collecting system and mean degree of dilation was 0.82 (0–2). There was no statistically significant difference with respect to parameters mentioned above between the two groups (Table 1).
Stones were located in right kidney in 44 cases (40%) and in left kidney in 66 cases (60%). Regarding the localization in the kidney 52 stones (47.3%) were in renal pelvis, 31 stones were in lower calyx (28.2%) and the remaining 27 stones were located in upper calyceal position (24.5%). Although 62 cases had opaque stones, the stones were non-opaque in 48 cases.
With respect to the possible radiation exposure values during each X-ray based imaging modality, while the estimated exposure ranged from 1.60 to 1.75 millisievert (mSv) for one CT imaging evaluation, these values were 2.6–2.9 mSv for IVU and 0.012–0.015 mSv for KUB examination, respectively.
Regarding the possible radiation exposure risk of the children evaluated for renal calculi prior to SWL, our data obtained in both group of cases revealed following findings:
When we evaluated the possible correlation between mean radiation exposure values in both groups on a radiologic imaging method based manner, our data clearly demonstrated that the mean exposure value to radiation was higher in children referring to ED than the other cases referring to OD (p = 0.0307). The main reason for this finding was the higher mean number of CT evaluation sessions performed in these cases when compared with the cases in other group (p = 0.0080). Our data showed that multiple X-ray based radiological evaluation (at least 2 of NCCT, IVU and KUB evaluations) has been performed in a total of 63 children (57.3%). However there was no significant difference between two groups regarding the mean number of KUB, IVU and sonographic evaluation performed prior to SWL management (Table 2).
On the other hand again, there was a significant correlation between the mean radiation exposure values and the stone size as well degree of dilation in a positive manner. In other words, as the size of the stone and the degree of dilation increased the mean value of radiation exposure did also increase in a parallel manner (p < 0.0001) (Table 3).
Last but not least, evaluation of the correlation for patient and stone related parameters (gender, laterality, stone location and opacity) on this aspect clearly showed that although a significant correlation was present between the mean radiation exposure of the children with the opacity of the stones treated (p < 0.0001) in a negative manner; we were not able to show any further correlation with respect to the other related parameters. As the opacity of the stone decreased mean radiation dosage increased in an inversely correlated manner (Table 4).
Discussion
With an overall incidence of 1–2%, pediatric urinary stone disease is often associated with high recurrence rates due to metabolic abnormalities, genitourinary anomalies and other certain factors requiring a close follow-up of each child on an individual basis [16,17,18,19,20]. Early assessment of the disease particularly in younger children is the most crucial part of the evaluation where radiologic imaging remains an integral part of the diagnosis as well as the management of symptomatic stones. Proper imaging using the appropriate means under required cautions is extremely important to limit the risk of radiation exposure particularly in this specific population. Like in adult cases, sonography, NCCT or IVU and plain KUB radiographs are the modalities used in the evaluation and follow-up of stones in children and depending on the type and also the number of the imaging modality used kids may receive excessive doses of radiation during the diagnostic evaluation of urinary calculi [8, 11].
Regarding the above-mentioned radiation exposure risk, highly limited data could be derived from the published literature focusing on the quantification of this exposure prior to the stone removal procedures in these cases. Unlike the adult cases, studies have clearly demonstrated that the radiation exposure in these cases for any reason is an important issue due to the relatively longer lifespan and more radiosensitive tissues making them particularly vulnerable to the long-term effects of ionizing radiation [21]. The National council on Radiation Protection and Measurements Report of 2009 estimates that approximately 8–10% of CT examinations in the USA were performed on children and concerns had been raised about the risks of increased radiation exposure in these patients [22].
In the light of these facts, collaborative efforts between clinicians, radiation physicists, public health officials and industry representatives have led the use of ALARA principle to limit the exposure as much as possible (particularly in pediatric population) and there is a widespread agreement that reducing radiation exposure should be a public health priority particularly in specific groups of patients like, pregnant women and children [8,9,10,11, 23]. To limit the risk of radiation exposure to a certain extent particularly in emergency conditions, despite their relatively bad image qualities low-dose radiation CT protocols have been used with high sensitivity and specificity in pediatric patients with an estimated effective dose of as low as 0.5 mSv [11, 21]. However, higher risk of radiation hazard and the necessity of anesthesia in the majority of these cases for a reliable CT imaging constitute the main disadvantages of this technique in children.
On the other hand, USG is an excellent tool of diagnosis for urinary stones particularly in children presenting in an acute setting. Moreover, wide availability of the system, quick application, noninvasiveness, lack of ionizing radiation and ability to define the anatomical changes in the urinary tract are the additional advantages of this modality. In addition to its non-invasive manner associated with no risk of radiation; sonographic evaluation of urinary calculi in children may also offer some further advantages which may ease the diagnosis of the stones and the associated obstruction as well. Related to this subject, published data have clearly demonstrated that as a valuable parameter “the twinkling artifact” evaluated and noted during this examination may be useful for the early detection of the mid ureteric (as well as some smaller stones) that represent the most difficult location in sonographic stone detection. Moreover, twinkling sign may also be helpful in the diagnosis of ureteral stones in patients presenting with renal colic in the emergency setting [24]. Related with this issue again, colour doppler sonography (CDU) in patients with renal colic and/or pelvicaliceal dilation was found to provide the advantage of improving the diagnostic accuracy of sonography in distinguishing obstructive from non-obstructive dilatation. Ureteral jet dynamics can be measured with CDU and this examination may provide information about ureteral peristaltism and as a useful adjunct to gray-scale ultrasound, Doppler ultrasound examination could ease differential diagnosis of ureteral obstruction from that of non-obstructive dilation. Moreover, due to the absence of contraindications and side-effects, CDU has been used for the follow-up of patients after ESWL, pregnant women and children [25, 26]. Last but not least, by providing size measurement KUB is useful in follow-up of patients with nephrolithiasis. Studies using a combination of USG and KUB have revealed a high sensitivity (79%) for direct detection of calculi and 100% sensitivity for indirect signs [21, 22].
Among the possible causes of higher radiation exposure before any planned definitive stone management, evaluation of these cases by different physicians during the same interval seems to be the most important one. Due to the lack of a well established correspondence between these physicians children may undergo the same imaging modality for several times mostly in different but sometimes in the same hospital. Moreover, children referring to the emergency departments with pain complaints undergo a CT evaluation due to the common tendency of the physicians to accept them as “acute abdomen” cases and evaluate them from a general perspective (not to miss any particular underlying pathology in this specific population). Thus, considering the facts mentioned above, ultimate diagnosis of stone disease in children (particularly in cases with obscure complaints) may take a long time period during which inconclusive KUB evaluations may also be performed to a certain extent.
Regarding the use of NCCT evaluation in our group, based on the risk of high radiation exposure we do not perform this evaluation particularly in pediatric cases in a routine manner. However, as mentioned above although 31 children out of 49 (63%) in our group referring directly to the ED with colic pain and abdominal distress symptoms required this evaluation in the differential diagnosis of stone disease¸ a couple of cases also presented with this evaluation performed in other centers. Finally in a limited number of outpatient cases (23 cases out of 61 children (38%)) a NCCT evaluation was performed due to the suspicious accompanying small ureteric stone(s).
In accordance to the facts mentioned above, data obtained in our current study also demonstrated a mean 2.72 ± 0.52 mSv dosage of radiation exposure in the children during the evaluation period before SWL management. Additionally our results showed that children in our group do undergo a mean 0.88 ± 0.10 number of CT evaluation, 4.10 ± 0.27 KUB and 0.30 ± 0.05 IVP evaluations prior to SWL treatment. When we evaluated the risk of radiation exposure in our group from different aspects our findings demonstrated well that the mean exposure value to radiation was higher in children referring to ED than the other cases referring to OD. The main reason for this finding was the higher mean number of CT evaluation sessions performed possibly due to the established attitude of the physicians to outline the cause of colic pain in a quick and reliable manner. This observation has been further supported by our observation with no significant difference regarding the use of other modalities (KUB, IVU) performed prior to SWL management. On the other hand again, stone size as well as the degree of upper tract dilatation have been found to be important factors on this aspect with a significant positive correlation between the mean radiation exposure values and the mean values of these factors. As the size of the stone and the degree of dilation increased the mean value of radiation exposure did also increase in a parallel manner. This might be again well explained by the need of multiple radiological evaluation sessions required for the detection of the exact stone configuration located in different parts of the kidney and also for the assessment of best treatment modality to remove such large calculi. Additionally, dilated systems do often require integrated radiologic evaluation in an attempt to outline the cause and degree of this dilation during both diagnosis and also follow-up of such cases. Dilation of upper tract demonstrated on sonography requires a contrast based imaging in majority of the cases to outline and evaluate the collecting system. Finally, a negative significant correlation was present between the mean radiation exposure values and the opacity of the stones treated. As the opacity of the stone decreased mean radiation dosage increased in an inversely correlated manner. This might be well explained with the need of multiple X-ray based radiological evaluations (including non-contrast CT) to outline the exact location of the stone along with the actual status of the upper tract collecting system in children with semi-opaque or non-opaque stones for a proper diagnosis of these stones.
As a result, it is essential that urologists should collaborate with radiologists, emergency room physicians and other relevant departments to balance the theoretical risks and practical benefits of ionizing radiation in the diagnosis of stone disease in an appropriate manner. However, despite all these concerns and careful approaches, it is clear that children with renal stones may expose to a varying doses of radiation beginning with the diagnostic evaluation phase prior to stone removal procedures for some certain reasons. Among the main underlying reasons for this condition, the evaluation of the cases with the same imaging modalities performed in different but sometimes in the same hospitals by the physicians without a well correspondence with each other. Additionally, children referring to emergency departments with obscure and vague symptoms are usually evaluated from a general perspective during which radiologic evaluation may cause unnecessary radiation exposure until final diagnosis of urinary stones is done. Taking all these facts into account, the risk of radiation and related problems could be minimized by performing sonography as the first and safest imaging modality particulary in these cases. When we include the additional risk of radiation exposure during the management as well as the follow-up of these cases the importance of sonographic evaluation gains further importance. If the aim is maximum safety and minimum risk of radiation exposure, the unnecessary use of NCCT evaluation (as well as IVU) should be avoided and performed only in cases where a final diagnosis could not be made with KUB and sonographic examinations. Any physician dealing with a child with stone(s) should obtain a detailed history particularly focusing on the previously performed radiologic evaluations in an attempt not to repeat them and increase the radiation exposure. Additionally, when necessary, they should get in touch with the previous responsible physician to obtain detailed information both about the course of the disease as well as the imaging modalities used so far. Last but not least, we believe that this problem could be best solved by evaluating, treating and also following these children in a center where all relevant experienced physicians are working together with a well established cooperation. Unnecessary performance of such radiological evaluations carrying high radiation risk could be avoided and the work load of the responsible physicians could be lowered with this approach.
Conclusions
In light of the increased awareness for the potential risks of ionizing radiation in pediatric patients, unnecessary use of X-ray based imaging modalities should be avoided in children with stones beginning from the diagnostic phase before any stone treatment modality. However, as the conventional NCCT is still over utilized even during the evaluation period in pediatric cases with stones, the risk of radiation exposure could be limited with the common use of KUB and USG combination particularly in children with recurrent stone disease.
Abbreviations
- ALARA:
-
As low as reasonably achievable
- CT:
-
Computed tomography
- ED:
-
Emergency department
- HU:
-
Hounsfield unit
- IVU:
-
Intravenous urography
- ICRP:
-
International Commission on Radiological Protection
- KUB:
-
Kidney-ureter-bladder
- mSv:
-
millisievert
- NCCT:
-
Noncontrast computed tomography
- OD:
-
Outpatient department
- SWL:
-
Shock wave lithotripsy
- UTI:
-
Urinary tract infection
- USG:
-
Ultrasonography
References
Sarica K (2008) Medical aspect and minimal invasive treatment of urinary stones in children. Arch Ital Urol Androl 80:43–49
Kroovand RL (1997) Pediatric urolithiasis. Urol Clin North Am 24:173–184
Minevich E (2001) Pediatric urolithiasis. Pediatr Clin North Am 48:1571–1585
Erbagcı A, Erbagcı BA, Yılmaz M et al (2003) Pediatric urolithiasis. Scand J Urol Nephrol 37:127–133
Koyuncu H, Yencilek F, Erturhan S et al (2011) Clinical course of pediatric urolithiasis: follow-up data in a long-term basis. Int Urol Nephrol 43:7–13
Thalgott M, Kurtz F, Gschwend JE et al (2015) Diagnostic imaging of urolithiais. Current recommendations and new developments. Urologe Ausg A 54:948–955
Preston DL, Cullings H, Suyama A et al (2008) Solid cancer incidence in atomic bomb survivors exposed in utero or as young children. J Natl Cancer Inst 100:428
Katz DS, Scheer M, Lumerman JH et al (2000) Alternative or additional diagnoses on unenhanced helical computed tomography for suspected renal colic: experience with 1000 consecutive examinations. Urology 56:53–57
Hernanz-Schulman M, Goske MJ, Bercha IH et al (2011) Pause and pulse: ten steps that help manage radiation dose during pediatric fluoroscopy. AJR Am J Roentgenol 197:475
Strauss KJ, Kaste SC (2006) The ALARA (as low as reasonably achievable) concept in pediatric interventional and fluoroscopic imaging: striving to keep radiation doses as low as possible during fluoroscopy of pediatric patients—a white paper executive summary. Radiology 240:621
Hyams ES, Shah O (2010) Evaluation and follow-up of patients with urinary lithiasis: minimizing radiation exposure. Curr Urol Rep 11:80–86
Johnson PB, Bahadori AA, Eckerman KF et al (2011) Response functions for computing absorbed dose to skeletal tissues from photon irradiation—an update. Phys Med Biol 56:2347–2365
Lee C, Lodwick D, Hurtado J et al (2010) The UF family of reference hybrid phantoms for computational radiation dosimetry. Phys Med Biol 55:339–363
Recommendations of the international commission on radiological protection 2007 (2007) ICRP publication 103. Ann ICRP 37:1–332
Gkanatsios NA, Huda W (1997) Computation of energy imparted in diagnostic radiology. Med Phys 24:571–579
Faerber GJ (2001) Pediatric urolithiasis. Urology 11:385–389
Spivacow FR, Negri AL, del Valle EE et al (2008) Metabolic risk factors in children with kidney stone disease. Pediatr Nephrol 23:1129–1133
Pietrow PK, Pope JC, Adams MC et al (2002) Clinical outcome of pediatric stone disease. J Urol 167:670–673
Milliner DS, Murphy ME (1993) Urolithiasis in pediatric patients. Mayo Clin Proc 68:241–244
Noe HN (2000) Hypercalciuria and pediatric stone recurrences with and without structural abnormalities. J Urol 164:1094–1096
Kluner C, Hein PA, Gralla O et al (2006) Does ultra-low-dose CT with a radiation dose equivalent to that of KUB suffice to detect renal and ureteral calculi? J Comput Assist Tomogr 30:44–50
Ripolles T, Agramunt M, Errando J et al (2004) Suspected ureteral colic: plain film and sonography vs unenhanced helical CT. A prospective study in 66 patients. Eur Radiol 14:129–136
Strauss KJ, Goske MJ (2011) Estimated pediatric radiation dose during CT. Pediatr Radiol 41:472–482
Ripolles T, Martinez-Perez MJ, Vizuete J et al (2013) Sonographic diagnosis of symptomatic ureteral calculi: usefulness of the twinkling artifact. Abdom Imaging 38:863–869
Pepe P, Motta L, Pennisi M et al (2005) Functional evaluation of the urinary tract by color-Doppler ultrasonography (CDU) in 100 patients with renal colic. Eur J Radiol 53:131–135
Jandaghi AB, Falahatkar S, Alizadeh A et al (2013) Assessment of ureterovesical jet dynamics in obstructed ureter by urinary stone with color Doppler and duplex Doppler examinations. Urolithiasis 41:159–163
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was not funded by any institution.
Conflict of interest
Bilal Eryildirim, Ozlem Turkoglu, Cemal Goktas, Ovunc Kavukoglu, Rasim Guzel and Kemal Sarica declares that he has no conflict of interest.
Ethical approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed.
Rights and permissions
About this article
Cite this article
Eryildirim, B., Turkoglu, O., Goktas, C. et al. Radiologic evaluation of children prior to SWL: to what extent they are exposed to radiation?. Urolithiasis 46, 485–491 (2018). https://doi.org/10.1007/s00240-017-1008-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00240-017-1008-8