Abstract
Purpose
Acute vertebrobasilar occlusion (VBO) has a grave clinical course; however, thrombectomy in VBO patients has rarely been reported. We retrospectively evaluated the clinical and radiological outcomes of thrombectomy in VBO patients.
Methods
From March 2010 to December 2017, 38 patients with 40 acute VBOs underwent thrombectomy at our hospital. Thrombectomy was performed using catheter aspiration (n = 11, 26.8%) or a stent retriever (n = 29, 70.7%).
Results
Good clinical outcomes (3-month modified Rankin scale (mRS) of 2 or lower) were achieved in 9 cases (22.5%), and successful recanalization (thrombolysis in cerebral infarction (TICI) grade of 2b or 3) was achieved in 35 cases (87.5%). Good clinical outcomes were significantly related to aetiologies other than atherosclerosis (p = 0.020) and lower National Institutes of Health Stroke Scale (NIHSS) scores on admission (p = 0.025). The clinical and radiological outcomes did not differ significantly between catheter aspiration and stent retriever thrombectomy (p = 1.000 and p = 0.603, respectively); however, stent retriever thrombectomy had a shorter procedure time than catheter aspiration (59.7 ± 31.2 vs. 84.5 ± 35.1 min, p = 0.037).
Conclusion
In our series, good clinical outcomes were associated with a lower NIHSS score on admission and stroke aetiologies other than atherosclerosis. The two thrombectomy modalities showed similar clinical and radiological outcomes. However, stent retrievers seemed to allow more rapid recanalization than catheter aspiration in VBO.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Vertebrobasilar occlusion (VBO) is an uncommon cause of ischaemic stroke, and in the absence of early reperfusion, it is associated with a high mortality rate of over 80% [1,2,3,4,5,6]. Furthermore, VBO can cause severe neurological disability even if patients survive with the help of intra-arterial (IA) or intravenous (IV) thrombolysis agents [1,2,3,4]. Thrombectomy of a major vessel occlusion of the anterior circulation has become a standard treatment for acute ischaemic stroke in the last decade, and several randomized controlled trials (RCTs) have shown that this procedure provides a benefit [1, 2, 4, 5]. The superiority of thrombectomy over IV thrombolysis for acute VBO is not definitively established because there are no data from RCTs on this topic. However, the current literature suggests that recanalization of VBO after IA thrombolysis is an important prognostic factor for survival and good functional outcomes [2,3,4,5,6,7].
Here, we reported our single-centre experience with thrombectomy for VBO. Furthermore, we evaluated the clinical and radiological outcomes of VBO and the prognostic factors affecting good clinical outcomes of VBO after thrombectomy. We also compared two thrombectomy modalities, catheter aspiration and stent retrievers, in patients with VBO.
Methods
Patient baseline and other characteristics
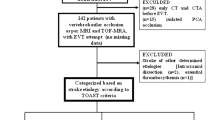
We reviewed patients with acute ischaemic stroke caused by VBO who underwent thrombectomy at our hospital from March 2010 to December 2017. During the study period, 38 patients (31 men, mean age ± standard deviation (SD) = 67.0 ± 12.4 years old) with a total of 40 VBOs were treated with thrombectomy using catheter aspiration or a stent retriever and were included in our study.
Data on baseline characteristics, procedure-related factors, and clinical and radiological outcomes were extracted from medical records. Medical records and imaging data were reviewed with the approval of the Institutional Review Board. Baseline characteristics included age, sex, past medical history, occlusion site, tandem lesion, stroke aetiology, and National Institutes of Health Stroke Scale (NIHSS) score on admission. Procedure-related factors included intravenous (IV) thrombolysis, thrombectomy modality, number of passes, whether the surgeon switched to the secondary modality, whether rescue treatments such as balloon angioplasty or stenting were needed, the time from the last normal time (LNT) to the emergency room (ER), the time from the ER to the intervention clinic (IC), the time from LNT to the IC, the procedure time and whether reocclusion occurred. Clinical and radiological outcomes included 3-month modified Rankin scale (mRS) and thrombolysis in cerebral infarction (TICI) grade.
The occlusion sites of VBO were divided into three categories: at the top of the basilar artery, at the basilar trunk, and at the vertebral arteries. VBO was classified as a single lesion or tandem lesion, with the latter including dual events, such as intracranial occlusion, and extracranial atherosclerotic stenosis, such as basilar trunk occlusion with atherosclerotic occlusion of the vertebral artery. Stroke aetiology was classified according to the Trial of Org 10172 in Acute Stroke Treatment (TOAST) criteria. Among the stroke aetiologies, atherosclerosis was divided into artery-to-artery embolism and in situ thrombo-occlusion [8, 9]. Patients admitted within 4.5 h of onset of acute ischaemic stroke symptoms were considered suitable candidates for IV t-PA infusion. Each patient’s NIHSS score was assessed on admission. Good clinical outcome was defined as a 3-month mRS score of 2 or lower, and successful recanalization was defined as a TICI grade of 2b or 3. The time from the LNT to the ER was defined as the total time from symptom onset to ER arrival. The time from the ER to the IC was defined as the total time from ER arrival to femoral puncture. The time from the LNT to the IC was defined as the total time from symptom onset to femoral puncture. The procedure time was defined as the total time from femoral puncture to puncture site closure.
Evaluations, including CT angiography, MR angiography, and conventional angiography, were performed to detect post-thrombectomy reocclusion. However, reocclusion was evaluated only when neurological deterioration occurred or reocclusion was strongly suspected in atherosclerotic occlusions with residual stenosis after thrombectomy.
The inclusion criteria were as follows: (1) acute ischaemic stroke with symptoms, (2) VBO confirmed by either CT or MR angiography, (3) less than 24 h from the LNT to treatment, and (4) thrombectomy procedure using catheter aspiration or a stent retriever. The exclusion criteria were as follows: (1) haemorrhagic stroke, (2) NIHSS score of 3 or lower, or (3) nearly all of the brain stem affected on diffusion imaging.
We excluded patients based on the extent to which the brainstem was affected by the occlusion, as indicated by diffusion imaging rather than by perfusion-diffusion mismatching, the latter of which generally serves as an indicator of the penumbra, because the low resolution of perfusion imaging in the brainstem has a limited ability to show the penumbra in the posterior circulation [10].
Procedure and periprocedural management
Procedures were performed under conscious sedation (n = 39) or under general anaesthesia (n = 1) via femoral access. Most procedures were performed under conscious sedation because general anaesthesia was not available for many cases of thrombectomy at our hospital. The primary thrombectomy modality was decided according to the surgeon’s discretion and was performed using catheter aspiration (Penumbra, Alameda, CA, USA) or a stent retriever (Solitaire FR stent (Medtronic, Irvine, CA, USA) or Trevo retrieve (Stryker Neurovascular, Fremont, CA, USA)). When persistent occlusion or incomplete recanalization was observed, the procedure was repeated. However, the first modality was not generally used more than three times. We switched to the second modality when the first modality did not achieve successful recanalization (TICI grade, 0 to 2a). When post-thrombectomy angiography showed residual stenosis in atherosclerotic occlusions and delayed angiography showed a subtle change in the residual stenosis, rescue treatments such as balloon angioplasty alone or balloon angioplasty with stenting were considered. Balloon angioplasty was considered first, with stenting additionally considered when residual stenosis did not improve after balloon angioplasty. Rescue treatments were not considered when delayed angiography showed no subtle change in the residual stenosis. When atherosclerosis was considered the aetiology of the occlusion, antiplatelet agents, including aspirin, clopidogrel, cilostazol, and combinations of these drugs, were administered. Aspirin plus clopidogrel dual antiplatelet therapy was used for patients who had received rescue treatments. Patients who did not receive rescue treatments were given a single antiplatelet therapy, including aspirin alone, clopidogrel alone, or cilostazol alone. When the risk of reocclusion was considered high, such as in the presence of a subtle change in the residual stenosis on delayed angiography, IA tirofiban injection was also used after thrombectomy depending on the patient’s condition.
Statistical analysis
Baseline characteristics, procedure-related factors, and clinical and radiological outcomes were compared according to clinical outcomes (good vs. poor) and thrombectomy modalities (catheter aspiration vs. stent retriever). The chi-squared test or Fisher’s exact test was used to analyse categorical variables, while Student’s t test or the Mann-Whitney U test was used for continuous variables. Multivariable analysis was used to evaluate factors affecting good clinical outcome. Variables for which p < 0.2 in the univariate analysis were selected for the logistic regression model. All analyses were performed with SPSS version 22 (SPSS, Chicago, IL, USA), and a value of p < 0.05 was considered indicative of statistical significance.
Results
In our study of 38 patients with 40 VBOs who were treated with thrombectomy, two patients initially had occlusion at the top of the basilar artery, followed by vertebral artery occlusion several days later. These two patients had atherosclerotic stenosis of the vertebral artery at the time of the first event; however, we decided not to treat the atherosclerotic stenosis in the vertebral artery at the first event, because the stenosis was not severe (approximately 20% in both patients) and showed no change during the procedure. However, the pre-existing stenosis in the vertebral artery showed occlusion several days later, and repeated thrombectomies were performed. Therefore, we report 40 VBOs in 38 patients.
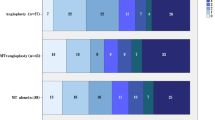
A good clinical outcome was achieved in 9 patients (23.7%), and successful recanalization was achieved in 35 cases (87.5%). The mRS values were distributed as follows: mRS 0, 3 patients; mRS 1, 4 patients; mRS 2, 2 patients; mRS 3, 6 patients; mRS 4, 7 patients; mRS 5, 12 patients; and mRS 6, 6 patients. Table 1 shows a comparison between patients with good clinical outcomes and those with poor clinical outcomes. Past medical history, such as diabetes, hypertension, hyperlipidaemia, and coronary disease, was not significantly associated with clinical outcomes.
The sites of VBO were as follows: 29 single-lesion VBOs, including 21 occlusions at the top of the basilar artery and 8 occlusions in the basilar trunk, and 11 tandem VBO lesions, including 3 occlusions at the top of the basilar artery with stenosis of the vertebral artery and 8 occlusions in the basilar trunk with stenosis of the vertebral artery. The occlusion site was not significantly associated with clinical outcome (p = 0.658), and the tandem lesions also had no such association (p = 0.399).
The aetiology of VBO included cardioembolism (n = 10, 25.0%), large-artery atherosclerosis (n = 20, 50.0%), unknown (n = 9, 22.5%), and dissection (n = 1, 2.5%). When stroke aetiology was divided into atherosclerosis and non-atherosclerosis, atherosclerosis was significantly associated with poor clinical outcome (19 out of 31 vs. 1 out of 9, p = 0.020). Among the atherosclerotic occlusions (n = 20), artery-to-artery embolisms were observed in 4 cases (20%), and in situ thrombo-occlusion was observed in 16 cases (80%). Rescue treatments were needed in 7 cases (none of which was artery-to-artery embolism), and all rescue treatments were needed for the in situ thrombo-occlusion. Reocclusion after thrombectomy occurred in 3 cases (18.8%), all of which were in situ thrombo-occlusions. Among the 3 patients with reocclusion, 1 patient underwent balloon angioplasty with stenting at the first event, and further treatment was not available after reocclusion. The other 2 patients did not receive rescue treatment (e.g. balloon angioplasty or stenting) at the first event, because they did not require rescue treatment owing to the lack of an interval change in contrast filling based on serial control angiography. However, reocclusion occurred in these 2 patients due to the pre-existing stenosis of the vertebral artery. Repeated thrombectomy achieved successful recanalization in the 2 patients without rescue treatment. Neither the rate of good clinical outcome nor successful recanalization differed significantly between artery-to-artery embolism and in situ thrombo-occlusion (0 out of 4 vs. 1 out of 16, p = 1.000, 3 out of 4 vs. 12 out of 16, p = 1.000, respectively).
NIHSS scores on admission ranged from 3 to 28 (13.70 ± 6.56). The mean ± SD NIHSS score on admission was 10.0 ± 4.64 in the group with good clinical outcomes and 14.8 ± 13.2 in the group with poor clinical outcomes. The difference between the two groups was significant (p = 0.025).
Although the statistical significance of some variables was not sufficient, our results have some numerical tendencies. The patients with good clinical outcomes had fewer passes (1.56 ± 1.01 vs. 2.16 ± 1.37 times, p = 0.227) and shorter procedure times (55.2 ± 30.7 vs. 69.8 ± 34.4 min, p = 0.259) than those with poor clinical outcomes. In our study, there was no significant relationship between good clinical outcome and either successful recanalization (p = 0.570) or reocclusion (p = 0.557). However, none of the patients with unsuccessful recanalization or reocclusion showed good clinical outcomes.
In a multivariable logistic regression analysis of good clinical outcomes, atherosclerosis as a stroke aetiology (adjusted odds ratio (OR); 0.055, confidence interval (CI); 0.005–0.574, p = 0.015) and NIHSS score on admission (adjusted OR; 0.839, CI; 0.710–0.991, p = 0.040) were significant predictors of a good clinical outcome.
Among the 40 thrombectomies performed at our hospital, 11 used catheter aspiration, and 29 used a stent retriever. A comparison between catheter aspiration and stent retriever thrombectomy is shown in Table 2. Catheter aspiration produced good clinical outcomes in 2 out of 11 cases (18.2%), and stent retriever thrombectomy produced good clinical outcomes in 7 out of 29 cases (24.1%); the difference between these two procedures was not significant (p = 1.000). Catheter aspiration achieved successful recanalization in 9 out of 11 cases (81.8%), and the stent retriever achieved successful recanalization in 26 out of 29 cases (89.7%). Therefore, the thrombectomy modality was not significantly associated with successful recanalization (p = 0.603).
Catheter aspiration was associated with a longer procedure time than the stent retriever (84.5 ± 35.1 vs. 59.7 ± 31.2 min, p = 0.037). In terms of the number of passes, catheter aspiration required 3.4 ± 2.2 passes per VBO, while stent retrievers required 2.1 ± 1.3 passes per VBO; this difference was not statistically significant (p = 0.085). Regarding the occlusion site, the stent retriever was used more frequently than catheter aspiration with occlusions at the top of the basilar artery (p = 0.002).
After failing to recanalize VBO with the first modality in 12 lesions (30%), we switched to the second modality. Switching from catheter aspiration to the stent retriever occurred in 3 cases out of 11 in which catheter aspiration was tried first (27.3%), and switching from the stent retriever to catheter aspiration occurred in 9 cases out of 29 cases in which the stent retriever was tried first (31.3%). In terms of the frequency of switching to a second modality, there were no statistically significant differences between catheter aspiration and stent retrievers (p = 1.000).
Significant stenosis after thrombectomy for VBO was observed in 7 patients, all of whom were treated by rescue treatment comprising balloon angioplasty either alone (n = 4) or with stenting (n = 3). Among the 35 successful recanalizations, 3 cases showed reocclusion after thrombectomy as observed on CT angiography or MR angiography within 1 day to several days after thrombectomy. The degree of residual stenosis in these 3 patients with reocclusion was 50%, 70%, and 80%. One of the three reocclusions is shown in Fig. 1. The aetiology of reocclusion was large-artery atherosclerosis in all 3 cases, and all three patients showed poor clinical outcomes (mRS 5).
Repeated thrombectomy using balloon angioplasty and stenting in a case of reocclusion after recanalization. A 71-year-old woman was admitted due to dizziness and global aphasia (NIHSS score 14). a CT angiography showed occlusion of the basilar artery. b We tried thrombectomy using a stent retriever. c Recanalization was achieved and several stenotic lesions were observed in the basilar artery. However, we decided to end this procedure because there was no interval change in delayed control angiography. d After 5 days, the patient showed mental deterioration and CT angiography showed reocclusion of the basilar artery. Repeated thrombectomy showed reocclusion. e The stent retriever was tried again, and recanalization was achieved. f Because this lesion was a reoccluded lesion, we decided to perform balloon angioplasty. g However, residual stenosis, indicating a high possibility of reocclusion, was still observed. h We decided to perform stenting for residual stenosis. i Final angiography showed successful recanalization with improved residual stenosis
There were no procedural complications, such as intracranial haemorrhage. The mortality rate was 15% (n = 6). Decompressive suboccipital craniectomy was performed in 2 patients, who both showed successful recanalization after thrombectomy; however, brain swelling progressed and was refractory to medical treatment. The two patients retained moderate neurological deficits after craniectomy (mRS 4).
Discussion
The prognosis of acute ischaemic stroke of the posterior circulation is very poor [1, 2]. In particular, if VBO is left untreated, the mortality rate will rise to 85%. However, there are few data on the proportion of VBOs among ischaemic strokes of the posterior circulation or on how to treat VBO. Thrombectomy has become an important treatment modality for large-artery occlusion of the anterior circulation [1, 2]; however, the efficacy and safety of thrombectomy in the posterior circulation are unclear.
During the thrombectomy procedure, it is important to identify the underlying cause of occlusion, especially distinguishing cardioembolism and large-artery atherosclerosis, and to set an optimal strategy to achieve better clinical outcomes. The posterior circulation has different characteristics from the anterior circulation, including the cause of the occlusion, details of the procedure (lack of availability of a balloon occlusion catheter), and the clinical course. Therefore, different strategies should be considered when performing thrombectomy for VBO, such as atherosclerotic aetiology, preparation of rescue treatment, and possibility of reocclusion.
The most common cause of ischaemic stroke is cardioembolism, accounting for 60% of all cases [11]. However, our study showed that the most common cause of VBO was large-artery atherosclerosis (n = 20, 50%). The anterior circulation is directly derived from the aortic arch, and the diameter of the common carotid artery is much larger than that of the vertebral artery. We believe that these anatomic differences between the anterior circulation and the posterior circulation may be related to a lower incidence of cardioembolic occlusion in the posterior circulation than in the anterior circulation [12].
It is known that large-artery atherosclerosis consists of artery-to-artery embolism or in situ thrombo-occlusion [8, 9, 13, 14]. In our study, the in situ thrombo-occlusion group was the only group in which rescue treatments were needed and occlusion occurred. Our study suggests that in situ thrombo-occlusion may have a greater association with rescue treatments and reocclusion than artery-to-artery embolism.
Our study showed that reocclusion occurred in 3 cases (n = 3, 7.5%) after thrombectomy for VBO, with all 3 cases resulting in poor clinical outcomes (mRS 5). When thrombectomy was performed for posterior circulation occlusion, the possibility of reocclusion should always be considered, because the procedure can lead to endothelial damage and in situ platelet aggregation [15]. The following considerations are important because of the possibility of reocclusion. First, if residual stenosis is observed after thrombectomy for VBOs, treatment should not be finished immediately after recanalization of the occlusion. Delayed control angiography should be performed, and any subtle change in residual stenosis should be carefully inspected [13]. If there is a suggestion of residual stenosis after thrombectomy, repeated control angiography every 5 min for 15 min was recently implemented at our hospital to mitigate reocclusion. Second, if delayed control angiography shows a subtle change in the residual stenosis, rescue treatments rather than repeated thrombectomy should be considered [13,14,15], especially in elderly patients with no evidence of cardioembolism, because large-artery atherosclerosis affects more elderly patients than younger patients [16]. Third, to prevent in situ platelet aggregation, which may occur after thrombectomy, IA tirofiban may be administered to prevent reocclusion of the residual stenosis after thrombectomy [17, 18]. Recently, it has been reported that the use of tirofiban showed a better recanalization rate and a lower incidence of intracranial haemorrhage, even when coadministered with IV tissue plasminogen activators [17, 19].
In our study, good clinical outcomes were related to NIHSS scores on admission (10.0 ± 4.64 vs. 14.8 ± 13.2, p = 0.025). The baseline NIHSS score is known as the best early predictor of functional outcomes in patients with acute cerebral infarction [3, 20, 21]. However, other studies [4, 19, 21,22,23] have suggested that with regard to disease assessment, the NIHSS score has relatively poor sensitivity in patients with posterior circulation stroke. Our study provides a basis for the relationship between NIHSS scores and clinical prognostic factors in posterior circulation stroke [3].
A prolonged procedure time and multiple device passes may cause endothelial injury, and these factors are associated with worse neurological recovery. Our results showed that patients with good clinical outcomes had a tendency to undergo fewer passes and have shorter procedure times than patients with poor clinical outcomes, which is consistent with previous reports [24]. The clinical outcome after thrombectomy for acute ischaemic stroke has been reported to be associated with the time interval from symptom onset to reperfusion; however, our results showed that good clinical outcomes had no relationship with the time from LNT to IC (p = 0.547), which is probably due to the small size of the study population. In our study, the time from ER to IC was 197.1 ± 99.3 min for patients with good clinical outcomes and 211.1 ± 130.2 min for patients with poor clinical outcomes, both of which may exceed the acceptable range. The reason for this long in-hospital delay time from ER to IC was because the prerequisite MRI for thrombectomy was not always available in our hospital, resulting in an unexpected time delay. Accordingly, to reduce the time delay from ER to IC, we revised the thrombectomy protocol of image evaluation based on CT angiography and CT perfusion.
In our study, good clinical outcomes (mRS 2 or less) were achieved at a relatively low rate (22.5%), despite the relatively high recanalization rate (87.5%). Our results also showed that there was no significant relationship between good clinical outcomes and successful recanalization (p = 0.570). The clinical course and prognosis of VBO are worse than those of ischaemic stroke in the anterior circulation. Therefore, especially for posterior circulation occlusions, VBO may have different definitions of clinical outcomes in our study, such as good clinical outcome (mRS 0 to 3) or the 90-day mortality rate. Comparing our results with the Basilar Artery International Cooperation Study (BASICS) registry [7], our results showed a lower number of cases with mRS 0 to 3 than did the BASICS registry (15 out of 40 (37.5%) vs. 19 out of 38 (50%)); however, our results showed a better 90-day mortality rate than the BASICS registry (6 out of 40 (15%) vs. 15 out of 38 (39.5%)).
Recently, it has been reported that successful recanalization and favourable clinical outcomes can be achieved with catheter aspiration for VBO [25, 26], whereas other reports stated that successful recanalization of the VBO can be achieved with a stent retriever [5, 15, 27]. However, few reports have compared catheter aspiration and stent retrievers in thrombectomy for VBO. Although our study was not an RCT, our results showed that there was no significant difference between catheter aspiration and stent retrievers in clinical (p = 1.000) or radiological (p = 0.603) outcomes. However, our study showed that the stent retriever was superior to catheter aspiration in terms of procedure time (84.5 ± 35.1 vs. 59.7 ± 31.2 min, p = 0.037) and the number of passes (3.4 ± 2.2 vs. 2.1 ± 1.3 times, p = 0.085).
Our result that catheter aspiration had a longer procedure time is not consistent with previous reports [11]. This finding may be explained by the higher incidence of atherosclerotic occlusion in our case series. The reasons why atherosclerosis was more common in our cases are as follows. First, unlike Western populations in which the causes of ischaemic stroke are primarily cardioembolism (60%) followed by large-artery atherosclerosis (15%) [11], atherosclerosis is more common in Asian populations [15, 28]. Second, atherosclerosis is more common in the posterior circulation than in the anterior circulation. Kang DH et al. reported that stent retrievers are more effective than catheter aspiration for acute large vessel occlusions with underlying intracranial atherosclerosis, which is consistent with our results [29].
Our study has several limitations. The study design is retrospective in nature, and we therefore cannot rule out selection bias. Additionally, there was no control group, and the cohort comprised a small number of subjects from a single centre. The comparison between catheter aspiration and stent retriever thrombectomy could have also limited the interpretation of the results, because there were 12 cases (30%) in which there was switching between the two methods. More evidence is required to obtain a definitive conclusion.
Conclusion
In our series, a good clinical outcome was related to a lower NIHSS score on admission and stroke aetiologies other than atherosclerosis. Our results suggest that stent retrievers are more appropriate than catheter aspiration as a first-line modality for thrombectomy in VBO. When atherosclerotic occlusion is suspected, repeated delayed control angiography is necessary to prevent reocclusion after the procedure, and maximal treatment, including balloon angioplasty or balloon angioplasty with stenting, should be considered.
References
Fahed R, Di Maria F, Rosso C et al (2017) A leap forward in the endovascular management of acute basilar artery occlusion since the appearance of stent retrievers: a single-center comparative study. J Neurosurg 126:1578–1584
Yang H, Ma N, Zhang S, Huo X, Gao F, Sun X, Mo D, Miao Z (2018) Endovascular revascularisation of acute tandem vertebrobasilar artery occlusion: seven case series with literature reviews. Stroke Vasc Neurol 3:17–21
Uno J, Kameda K, Otsuji R, Ren N, Nagaoka S, Maeda K, Ikai Y, Gi H (2017) Mechanical thrombectomy for acute basilar artery occlusion in early therapeutic time window. Cerebrovasc Dis 44:217–224
Mak CH-K, Ho JW-K, Chan K-Y et al (2016) Intra-arterial revascularization therapy for basilar artery occlusion—a systematic review and analysis. Neurosurg Rev 39:575–580
Long J, Qin H, Zhang H (2017) Evaluation of recanalisation treatment on posterior circulation ischemic stroke by Solitaire device—a multicenter retrospective study. Neurol Neurochir Pol 51:208–213
Luo G, Mo D, Tong X, Liebeskind DS, Song L, Ma N, Gao F, Sun X, Zhang X, Wang B, Jia B, Fernandez-Escobar A, Miao Z (2018) Factors associated with 90-day outcomes of patients with acute posterior circulation stroke treated by mechanical thrombectomy. World Neurosurg 109:e318–e328
van Houwelingen RC, Luijckx G-J, Mazuri A et al (2016) Safety and outcome of intra-arterial treatment for basilar artery occlusion. JAMA Neurol 73:1225
Qureshi AI, Caplan LR (2014) Intracranial atherosclerosis. Lancet 383:984–998
Banerjee C, Chimowitz MI (2017) Stroke caused by atherosclerosis of the major intracranial arteries. Circ Res 120:502–513
Kim SJ, Ryoo S, Bang OY, Chung CS, Lee KH, Kim GM (2010) Perfusion-weighted MRI as a predictor of clinical outcomes following medullary infarctions. Cerebrovasc Dis 29:382–388
Kistler JP, Furie KL (2000) Carotid endarterectomy revisited. N Engl J Med 342:1743–1745
Labropoulos N, Nandivada P, Bekelis K (2011) Stroke of the posterior cerebral circulation. Int Angiol 30:105–114
Kang D-H, Kim Y-W, Hwang Y-H et al (2014) Instant reocclusion following mechanical thrombectomy of in situ thromboocclusion and the role of low-dose intra-arterial tirofiban. Cerebrovasc Dis 37:350–355
Mordasini P, Brekenfeld C, Byrne JV et al (2013) Technical feasibility and application of mechanical thrombectomy with the Solitaire FR revascularization device in acute basilar artery occlusion. Am J Neuroradiol 34:159–163
Tian C, Cao X, Wang J (2017) Recanalisation therapy in patients with acute ischaemic stroke caused by large artery occlusion: choice of therapeutic strategy according to underlying aetiological mechanism? Stroke Vasc Neurol 2:244–250
Fromm A, Waje-Andreassen U, Thomassen L et al (2011) Comparison between ischemic stroke patients <50 years and ≥50 years admitted to a single centre: the Bergen stroke study. Stroke Res Treat 20:183256
Niu J, Ding Y, Zhai T et al (2019) The efficacy and safety of tirofiban for patients with acute ischemic stroke: a protocol for systematic review and a meta-analysis. Medicine (Baltimore) 98:e14673
Yu T, Lin Y, Jin A, Zhang P, Zhou X, Fang M, Liu X (2018) Safety and efficiency of low dose intra-arterial tirofiban in mechanical thrombectomy during acute ischemic stroke. Curr Neurovasc Res 15:145–150
Xianxian Z, Chengsong Y, Qiang M et al (2017) The efficiency analysis of thrombolytic rt-PA combined with intravascular interventional therapy in patients with acute basilar artery occlusion. Int J Biol Sci 13:57–64
Young FB, Weir CJ, Lees KR (2005) Comparison of the National Institutes of Health Stroke Scale with disability outcome measures in acute stroke trials. Stroke 36:2187–2192
Gory B, Mazighi M, Labreuche J, Blanc R, Piotin M, Turjman F, Lapergue B, ETIS (Endovascular Treatment in Ischemic Stroke) Investigators (2018) Predictors for mortality after mechanical thrombectomy of acute basilar artery occlusion. Cerebrovasc Dis 45:61–67
Linfante I, Llinas RH, Schlaug G et al (2001) Diffusion-weighted imaging and National Institutes of Health Stroke Scale in the acute phase of posterior-circulation stroke. Arch Neurol 58:621–628
Tsao JW, Hemphill JC, Johnston SC et al (2005) Initial Glasgow Coma Scale score predicts outcome following thrombolysis for posterior circulation stroke. Arch Neurol 62:1126
Neuberger U, Kickingereder P, Schönenberger S, Schieber S, Ringleb PA, Bendszus M, Pfaff J, Möhlenbruch MA (2019) Risk factors of intracranial hemorrhage after mechanical thrombectomy of anterior circulation ischemic stroke. Neuroradiology 61:461–469
Kwon J-H, Shin SH, Weon YC et al (2011) Intra-arterial adjuvant tirofiban after unsuccessful intra-arterial thrombolysis of acute ischemic stroke: preliminary experience in 16 patients. Neuroradiology 53:779–785
Son S, Choi DS, Oh MK, Hong J, Kim SK, Kang H, Park KJ, Choi NC, Kwon OY, Lim BH (2016) Comparison of Solitaire thrombectomy and Penumbra suction thrombectomy in patients with acute ischemic stroke caused by basilar artery occlusion. J Neurointerv Surg 8:13–18
Li W, Lin L, Zhang M et al (2016) Safety and preliminary efficacy of early tirofiban treatment after alteplase in acute ischemic stroke patients. Stroke 47:2649–2651
Kim BJ, Kim JS (2014) Ischemic stroke subtype classification: an asian viewpoint. J Stroke 16:8–17
Kang DH, Yoon W, Baek BH et al (2019) Front-line thrombectomy for acute large-vessel occlusion with underlying severe intracranial stenosis: stent retriever versus contact aspiration. J Neurosurg 29:1–7
Funding
This study was not funded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We declare that we have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were conducted in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, D.H., Kim, S.H., Lee, H. et al. Thrombectomy in acute vertebrobasilar occlusion: a single-centre experience. Neuroradiology 62, 723–731 (2020). https://doi.org/10.1007/s00234-020-02376-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-020-02376-1