Abstract
Purpose
To recommend a new simple and explicit index termed the anteroposterior diameter of the lateral ventricle index (ALVI) for assessing brain ventricular size in neuroimaging and to compare Evans index (EI) between idiopathic normal pressure hydrocephalus (iNPH) patients and age-matched healthy elderly subjects.
Methods
Retrospective measurements of ventricular volume (VV), relative VV (RVV), the EI, and the ALVI were taken from thin-section CT scans for 23 pre-shunt-insertion iNPH patients and 62 age-matched healthy elderly volunteers. The area under the receiver operating characteristic (ROC) curve (AUC), net reclassification improvement (NRI), and integrated discrimination improvement (IDI) were calculated to assess the effectiveness of ALVI scores for predicting VV.
Results
The correlations between VV or RVV and ALVI scores (VV, r = 0.957; RVV, r = 0.983) were significantly stronger than the corresponding correlations with EI scores (VV, r = 0.843; RVV, r = 0.840). The AUC for ALVI scores was significantly greater than the AUC for EI scores. Furthermore, with the inclusion of the ALVI, the NRI value was 0.14 and the IDI value was 0.14; these improvements were also statistically significant.
Conclusion
The ALVI is a more accurate and more explicitly defined marker of VV than the EI and assesses ventricular enlargement effectively. We suggest that ventricular enlargement of the healthy elderly be defined by ALVI > 0.50.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Normal-pressure hydrocephalus (NPH) was first described in 1965 [1] and is characterized by gait disturbance, urinary incontinence, mental deterioration, and the presence of normal cerebrospinal fluid (CSF) pressure on lumbar puncture (LP), the radiologic finding of communicating hydrocephalus, and improvements after implantation of a CSF shunt [2,3,4]. Ventricular enlargement is a key diagnostic criterion for NPH, but direct measurements of ventricular volume (VV) can be time consuming and was not easy. Linear indices are an alternative, faster method of assessing ventricular dilation.
The Evans’ index (EI) is the ratio of the transverse diameter of the anterior horns of the lateral ventricles to the greatest internal diameter of the skull [5]. The EI is currently the most commonly used index of ventricular size in neurosurgery and is recommended in NPH guidelines for the assessment of idiopathic NPH (iNPH) [5].
However, EI can vary significantly in iNPH patients, depending on different the levels of the brain CT scan image [6]. This issue is compounded by the fact that guidelines for iNPH describe the EI in just a simple sentence without detailed measurement level of the brain imaging [2, 3]; these simple definitions lack an explicit description of a standard measurement method for the EI. Therefore, a more reliable index could improve assessments of ventricular volume and diagnosis of iNPH. We designed a new, simple, and explicitly described index termed the anteroposterior diameter of the lateral ventricle index (ALVI), and sought to use this new index to reliably assess ventricular volume (VV). The aims of this study were to investigate the relationship between ALVI scores and VV and to compare the effectiveness of the ALVI and EI in assessing VV in iNPH patients and age-matched healthy controls.
Methods
Patients and volunteers
We retrospectively reviewed thin-section CT scans of the brains of 23 patients with definite iNPH (age 73 ± 7 years; range 60–89 years; 13 men and 10 women) at our hospital. All patients met the diagnostic criteria of the Japanese and international iNPH guidelines and exhibited objective improvements in gait, urinary symptoms, and cognition after CSF shunting between 2015 and 2017. All brains CT scans of the patients were acquired before CSF shunting.
An advertisement was placed in the local several community bulletin board asking elderly persons (60–90 years) to apply for participation in the study if they considered themselves healthy. After telephone interviews by two authors, the healthy control was selected. The control group comprised 75 age-matched healthy participants who underwent thin-section CT scanning during the same time period as the iNPH patients. Six persons were excluded because of suspected cognitive disorders, three because of unexplained gait disturbances over nearly 2 years, two because of a previous history of intradural hematomas, and two because of urinary urgency. Atrophy, lacunar strokes, transient dizziness, and headache were not used as exclusion criteria. Sixty-two age-matched healthy persons were recruited in the control group. The mean age was 75 ± 8 years (range 60–86 years; 41men and 21women). The protocol was approved by the Hospital Bioethics Committee (approval no.2017K057).
Image collection
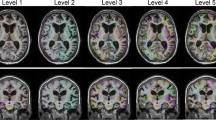
Brain CT imaging (from the apex to the base of the skull) was performed with a 64-detector CT system (GE Light Speed VCT or GE Discovery CT750 HD, GE Healthcare, Milwaukee, WI, USA) using the following protocol parameters: 1.25-mm section width with a 1.25-mm reconstruction interval, 120 kV, 360 mA. All DICOM database of CT were transmitted to GE Advantage Workstation 4.4 software (VolumeShare 2, GE Healthcare, Milwaukee, WI, USA) through Picture Archiving and Communication Systems (PACS) for image post-processing. Axial images parallel to the anterior commissure–posterior commissure (AC-PC) plane were acquired with the multiplanar reformer function in GE Advantage Workstation 4.4 software, with a slice thickness of 1 mm and a spacing of 1 mm between images (Fig. 1a).
a Standard axial plane used for calculating the ALVI (anteroposterior diameter of the lateral ventricle index). The CT slice is in the plane of body of lateral ventricle where the cella media first appears unobscured by other regions (thalamus). ALVI is the length of the dashed line/length of the solid line. The dashed line denotes the anteroposterior diameter of the lateral ventricle. The solid line denotes the maximal width of the anteroposterior inner diameter of the skull (along the cerebral falx). b Axial plane in which the lateral ventricle is partially obscured by thalamus (arrow)
Image analysis
The VV and the total intracranial volume (ICV) were measured on all scans using the segment and display functions in GE Advantage Workstation VolumeShare 2 software. All the segmentation results were visually tested. Manual corrections were performed in those cases in which the semiautomatic segmentation did not meet the desired level of accuracy.
EI was measured as the ratio of the maximal transverse diameter of the frontal horns of the lateral ventricles to the greatest internal diameter of the skull [2,3,4,5]; the former was determined by measuring several consecutive axial slices chosen by the operator and selecting the slice with the largest diameter, and the latter was determined from the same slice used for the maximal width of the frontal horns.
To compute the ALVI, we first identified the axial slice in the plane of body of lateral ventricle where the cella media (central part of lateral ventricle) first appears unobscured by other regions (thalamus) from skull base to skull roof (Fig. 1). Next, we measured the anteroposterior diameter of the left and right lateral ventricles in this axial slice. Occasionally, the anteroposterior diameters were markedly different for the left and right ventricles (such as in Fig. 4c, e), with the magnitude of the difference varying from 1 to 3 cm. When the difference between the anteroposterior diameters of the left and right ventricles was greater than 1 cm, the diameter measurement was defined as the mean of the diameters of the left and right lateral ventricles. When the difference between the anteroposterior diameters of the left and right ventricles was equal to or less than 1 cm, the diameter measurement was defined as the larger of the two measured ventricle diameters. The ALVI was defined as the ratio of this lateral ventricle diameter measurement to the maximal width of the anteroposterior inner diameter of the skull (along the cerebral falx) in the same plane (Fig. 1).
Measurements of all linear indices (ALVI and EI) and volumes (VV and ICV) were performed in a double-blind manner. Two independent operators measured the ALVI and the EI, and two other operators measured the ventricular volumes; each pair of operators comprised a radiologist and a neurosurgeon. The intraclass correlation coefficients were 0.99, 0.96, 0.98, and 0.99 for ALVI, EI, VV, and ICV, respectively.
Diagnostic criteria
There is currently no accurate threshold for ventricular dilation [2, 3], and cerebral ventricular size can vary with ethnicity, sex, and age [7,8,9,10]. As described in previous criteria [11], ventricular dilation was defined as a VV value above the 95th percentile in the healthy elderly control participants.
Statistical methods
The statistical analyses were performed in the statistical software programs SAS (version 9.0; SAS Institute Inc., Cary, NC) and MedCalc (version 15.2.2; MedCalc Software BVBA, Ostend, Belgium; http://www.medcalc.org; 2015). Statistical significance was set at P < 0.05. Scatterplots, Spearman’s rank correlations, and linear regressions were used to compare the relationships between the linear indices (ALVI and EI) and the VV and relative VV (RVV). The area under the receiver operating characteristic (ROC) curve (AUC) was used to evaluate the predictive abilities of ALVI and EI. The discriminative value of ALVI relative to EI was examined by calculating the net reclassification improvement (NRI) and the integrated discrimination improvement (IDI) [12].
Results
The ALVI, EI, VV, and RVV measurements for all subjects are presented in Table 1. In the healthy control, VV and RVV were normally distributed. Figure 2 presents the relationship between the linear indices (ALVI and EI) and VV. There were significant correlations between the linear indices (ALVI and EI) and VV and RVV (ALVI, RVV = 0.957 and RRVV = 0.983; EI, RVV = 0.843 and RRVV = 0.840, P < 0.001 for all correlations), and the ALVI correlation coefficients were significantly greater than the EI correlation coefficients (P < 0.001).
Using the 95th percentile of the VV of the healthy age-matched control subjects as the threshold for ventricular enlargement, the AUC values for the sensitivity/specificity ROC curves were 0.991 (95% confidence interval (CI)0.942–1.0) for ALVI and 0.949 (95% CI: 0.879–0.985) for EI, and the incremental AUC was statistically significant (0.0421, 95% CI 0.0024–0.0819, P = 0.038), suggesting that the ALVI is more effective than the EI. For a cut-off ALVI value of 0.501 as the threshold for ventricular enlargement, ALVI specificity was 100% and sensitivity was 98.3%.
Next, we introduced two statistical methods—NRI and IDI—to evaluate the added predictive ability of the ALVI [12]. We examined the NRI and IDI for the ALVI and EI across all individuals, using an ALVI value of 0.50 and an EI value of 0.30 as the thresholds for ventricular enlargement (Table 2). With ALVI, the NRI increased by 0.14 (95% CI 0.024–0.261) and the IDI increased by 0.14 (95% CI 0.022–0.263); these increases were statistically significant (NRI, P = 0.023; IDI, P = 0.020). Our results indicate that ALVI provides significant increases in discrimination and net reclassification for ventricular enlargement and is more effective than EI for evaluating ventricular size.
Discussion
The present study main result has shown that ALVI is a more accurate and more explicitly defined marker of brain ventricular size than the EI and assesses ventricular enlargement effectively.
In 1942, William Evans developed the EI to assess ventricular size from sagittal-view pneumoencephalograms in children; at that time, he set the criterion for definite ventricular enlargement as EI > 0.30. However, EI measurements from axial CT and MR images do not resemble the measurements from sagittal pneumoencephalograms, in which it is easy to measure the greatest frontal horn diameter and the maximum internal diameter of the skull in a single image [5]. Moreover, the EI > 0.30 threshold for lateral ventricle expansion has been challenged, with some studies suggesting that this threshold does not reliably differentiate between normal and enlarged ventricles [13, 14]. Despite this, EI measurements are now widely derived from axial-view CT and MR images, and the original threshold value of 0.30 for ventricular enlargement is still used today, especially in elderly. Additionally, definitive descriptions of a standard measurement level for the EI based on CT and MR images are rare in the authoritative guidelines for iNPH [2,3,4].
The selection of different scan baselines, the selection of different planes, and differences in posture (especially for iNPH patients with consciousness disorders) all affect the axial ventricle shape and thus linear measurements [6]. Because of the potential for measurement bias with the EI, we developed the ALVI for assessing ventricular size. We defined an easy-to-access standard level in axial CT or MR images, in the plane of body of lateral ventricle at the point where the cella media first appears unobscured by other regions (thalamus). The linear measurement values and standard level used to calculate the ALVI are singular: unlike the EI, there is no requirement for the operators to take measurements from several consecutive axial slices to identify the largest diameter. The measurement method for the ALVI is therefore simpler and more explicit than that for EI, reducing measurement bias.
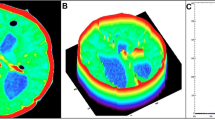
Although statistical analyses indicate that EI can accurately evaluate VV, we found that EI demonstrated some bias in its predictions (Fig. 4a–c) whereas ALVI provided a more explicit assessment of VV. In our study, five healthy elderly individuals with normal VVs had EI values above 0.30; however, the ALVI values for these individuals were below 0.50 (e.g., Fig. 4d). Several studies have demonstrated that a cut-off value of 0.3 for EI cannot be used to differentiate between normal and enlarged ventricles in individual cases, and it has been suggested that the EI cut-off value should be adjusted, e.g., to 0.33 [13, 14]. However, increasing the cut-off value of EI could exclude more individuals who do have enlarged ventricles. Among our control subjects, two elderly individuals had EI values lower than 0.30 but were deemed to have ventricular dilation, as determined by a VV greater than the 95th percentile (e.g., Fig. 4e). In these cases, the ALVI values were greater than 0.50 and thus accurately reflected the ventricular dilation (Fig. 4e). In terms of performance, the ALVI scores reflected VV and RVV more closely than the EI scores.
a–c CT images from three idiopathic normal-pressure hydrocephalus (iNPH) patients with similar ventricular volumes of approximately 140 mL (138 mL, 136 mL, and 135 mL, in panels a, b and c, respectively). The ALVI (anteroposterior diameter of the lateral ventricle index) values were similar for all three patients (0.601, 0.583, and 0.603), but the Evans’ index (EI) values differed substantially (0.370, 0.307, and 0.434). d CT image from a healthy elderly individual. In this individual, the EI was 0.312 but the VV (44 mL) was below the 95th percentile for healthy elderly subjects. The ALVI value was 0.446. e, CT image from a healthy elderly individual. In this individual, the VV (96 mL) was above the 95th percentile for the healthy elderly subjects, but the EI was 0.291. The ALVI was 0.517
Ventricular dilation is a characteristic feature of iNPH patients that distinguishes them from healthy control [1,2,3, 15]. Direct measurement of the VV is undisputedly the best method to identify ventricular dilation. VV can be measured by advanced imaging postprocessing technology in approximately 10 min, and sometimes even as quickly as a few minutes [16], especially if specialized brain tools are used. We spent an average of 15 min per subject measuring both VV and ICV using a manual tool. However, existing studies have failed to find a positive correlation between the clinical prognosis and changes in ventricle size [17, 18]. For current research and clinical needs, all we need to know is whether the VV of suspected patients indicates dilation; we do not need the exact VV values. Thus, linear indices continue to have great clinical value. ALVI is therefore a simpler and more accurate linear index than EI and should be granted attention and use (Table 3).
Study limitations
All of the individuals were from a single center. This study was a retrospective study and lacks prospective analysis. We did not validate different methods of measuring VV. Because most healthy elderly people had only CT scans available and no further medical information, we did not examine correlations between the clinical prognoses and ALVI values or the connection between ALVI values and the results of clinical trials for iNPH.
Conclusion
ALVI is a simpler, more explicit, and more accurate marker of VV than EI and can assess ventricular enlargement more effectively. We suggest that the threshold for ventricular enlargement of the healthy elderly be defined as ALVI > 0.50.
References
Adams R, Fisher C, Hakim S, Ojemann R, Sweet W (1965) Symptomatic occult hydrocephalus with normal cerebrospinal-fluid pressure — a treatable syndrome. N Engl J Med 273:117–126
Relkin N, Marmarou A, Klinge P, Bergsneider M, Black PM (2005) Diagnosing idiopathic normal-pressure hydrocephalus. Neurosurgery 57:S4–S16
Mori E, Ishikawa M, Kato T, Kazui H, Miyake H, Miyajima M, Nakajima M, Hashimoto M, Kuriyama N, Tokuda T, Ishii K, Kaijima M, Hirata Y, Saito M, Arai H (2012) Guidelines for management of idiopathic normal pressure hydrocephalus: second edition. Neurol Med Chir (Tokyo) 52:775–809
Williams MA, Relkin NR (2013) Diagnosis and management of idiopathic normal-pressure hydrocephalus. Neurol Clin Pract 3:375–385
Jr EW (1942) An encephalographic ratio for estimating the size of the cerebral ventricles - further experience with serial observations. Am J Dis Child 64:820–830
Toma AK, Holl E, Kitchen ND, Watkins LD (2011) Evans' index revisited: the need for an alternative in normal pressure hydrocephalus. Neurosurgery 68:939–944
Skullerud K (1985) Variations in the size of the human brain. Influence of age, sex, body length, body mass index, alcoholism, Alzheimer changes, and cerebral atherosclerosis. Acta Neurol Scand Suppl 102:1–94
Agartz I, Marions O, Saaf J, Wahlund LO, Wetterberg L (1992) Visual rating of magnetic resonance images of human cerebrospinal fluid spaces and white brain matter: relation to sex and age in healthy volunteers. Magn Reson Imaging 10:135–142
Giedd JN, Castellanos FX, Rajapakse JC, Vaituzis AC, Rapoport JL (1997) Sexual dimorphism of the developing human brain. Prog Neuro-Psychopharmacol Biol Psychiatry 21:1185–1201
Coffey CE, Lucke JF, Saxton JA, Ratcliff G, Unitas LJ, Billig B, Bryan RN (1998) Sex differences in brain aging: a quantitative magnetic resonance imaging study. Arch Neurol 55:169–179
Ambarki K, Israelsson H, Wahlin A, Birgander R, Eklund A, Malm J (2010) Brain ventricular size in healthy elderly: comparison between Evans index and volume measurement. Neurosurgery 67(94–99):99
Pencina MJ, D'Agostino RS, D'Agostino RJ, Vasan RS (2008) Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med 27(157–172):207–212
Brix MK, Westman E, Simmons A, Ringstad GA, Eide PK, Wagner-Larsen K, Page CM, Vitelli V, Beyer MK (2017) The Evans’ index revisited: new cut-off levels for use in radiological assessment of ventricular enlargement in the elderly. Eur J Radiol 95:28–32
Jaraj D, Rabiei K, Marlow T, Jensen C, Skoog I, Wikkelso C (2017) Estimated ventricle size using Evans index: reference values from a population-based sample. Eur J Neurol 24:468–474
Jaraj D, Rabiei K, Marlow T, Jensen C, Skoog I, Wikkelso C (2014) Prevalence of idiopathic normal-pressure hydrocephalus. Neurology 82:1449–1454
Nestor SM, Rupsingh R, Borrie M, Smith M, Accomazzi V, Wells JL, Fogarty J, Bartha R (2008) Ventricular enlargement as a possible measure of Alzheimer’s disease progression validated using the Alzheimer’s disease neuroimaging initiative database. Brain 131:2443–2454
Palm WM, Walchenbach R, Bruinsma B, Admiraal-Behloul F, Middelkoop HA, Launer LJ, van der Grond J, van Buchem MA (2006) Intracranial compartment volumes in normal pressure hydrocephalus: volumetric assessment versus outcome. AJNR Am J Neuroradiol 27:76–79
Palm WM, Saczynski JS, van der Grond J, Sigurdsson S, Kjartansson O, Jonsson PV, Eiriksdottir G, Gudnason V, Admiraal-Behloul F, Launer LJ, van Buchem MA (2009) Ventricular dilation: association with gait and cognition. Ann Neurol 66:485–493
Funding
This study was funded by the Project of Shenzhen International Cooperation Foundation (GJHZ20180926165402083).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
He, W., Fang, X., Wang, X. et al. A new index for assessing cerebral ventricular volume in idiopathic normal-pressure hydrocephalus: a comparison with Evans’ index. Neuroradiology 62, 661–667 (2020). https://doi.org/10.1007/s00234-020-02361-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-020-02361-8