Abstract
Introduction
Cerebral punctate and curvilinear gadolinium enhancements (PCGE) correspond to opacification of small vessel lumen or its perivascular areas in case of blood-brain barrier (BBB) disruption. We will discuss the possible causes of intra-parenchymal central nervous system PCGE.
Methods
Our review is based on French database including patients presenting with central nervous system PCGE and literature search using PubMed database with the following keywords: punctate enhancement, linear enhancement, and curvilinear enhancement. Disorders which displayed linear leptomeningeal or periventricular enhancements without intra-parenchymal PCGE are excluded of this review.
Results
Among our 39 patients with PCGE, 16 different diagnoses were established. After combining our PCGE causes with those described in the literature, we propose a practical approach. Besides physiologic post-contrast enhancement of small vessels, three pathologic conditions may exhibit PCGE: (1) small collateral artery network seen in Moyamoya syndrome, (2) small veins congestions related to developmental or acquired venous outflow disturbance, and (3) disorders causing small vessels BBB disruption indicated by T2 and FLAIR hyperintensities in the corresponding areas of PCGE. Disruption of the BBB could be caused by a direct injury of the endothelial cell, as in posterior reversible encephalopathy syndrome, Susac syndrome, and radiochemotherapy-induced injuries, or by an angiocentric cellular infiltrate, as in inflammatory disorders, demyelinating diseases, host immune responses fighting against infections, prelymphoma states, lymphoma, and in CLIPPERS.
Conclusion
PCGE may conceal several causes, including physiological and pathological conditions. Nevertheless, a practical approach could improve its management and limit the indications of brain biopsy to very specific situations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cerebral punctate and curvilinear gadolinium enhancements (PCGE) correspond to opacification of small vessel lumen or its perivascular areas in case of blood-brain barrier (BBB) disruption. In physiological situation, conventional angiography is more suitable than contrast-enhanced T1-weighted images to observe small vessels such as perforating medullary arteries and deep medullary veins. However, conventional angiography cannot provide images of vessels with diameter less than 0.2 mm (i.e. precapillary arterioles, capillaries, and postcapillary venules) [1]. Therefore, in presence of BBB breakdown concerning vessels with diameter less than 200 μm, as displayed on histological findings, magnetic resonance imaging (MRI) can show PCGE in absence of vascular damage on conventional angiography [2].
Punctate enhancement is defined as dotlike enhancement with a diameter less than 3 mm, while round enhancement with a diameter ranging from 3 to 9 mm is considered as nodular enhancement [3]. According to the image section, either perpendicular or parallel to the long axis of the small vessel, contrast enhancement is respectively punctate or curvilinear.
The aim of this review is to describe the main situations that can present cerebral intraaxial PCGE on T1-weighted images (TWI). After rule out physiologic post-contrast enhancement of small vessels, three pathologic conditions may exhibit PCGE: (1) small collateral artery network seen in Moyamoya syndrome, (2) small veins congestions related to developmental or acquired venous outflow disturbance, and (3) disorders causing small vessels BBB disruption. Finally, we propose a diagnostic strategy and indicate the situations where brain biopsy seems crucial.
Materials and methods
Since the publication of the French chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) cohort in 2012 [4], a database was established including patients presenting with CNS parenchymal PCGE. Among 39 patients collected, 16 different diagnoses were identified (Table 1). In the present review, one patient has been selected in each diagnosis category (n = 16). In addition, other causes of PCGE have been documented using PubMed database with the following keywords: “punctate enhancement, linear enhancement, and curvilinear enhancement”. Local ethical committee approved this study.
Disorders that displayed pachymeningeal, leptomeningeal, gyral, nodular, patchy, open- and closed-ring, and periventricular enhancements in absence of intra-parenchymal PCGE will be not discussed. Because this review is based on a retrospective database analysis and a review of the literature, promising sequences such as susceptibility-weighted imaging (SWI), which is able to highlight small veins, and postcontrast FLAIR imaging that could show BBB disruption have not been evaluated.
Results
In our database of patients with CNS parenchymal PCGE (Table 1), 16 cases were selected according to their final diagnosis. In each case, clinical findings, radiological features, and explorations needed to determine the diagnosis are listed in Table 2 (patients 1–8) and in Table 3 (patients 9–16). Based on our database and PubMed research, the CNS PCGE aetiologies are successively addressed.
Physiologic post-contrast enhancement of the small vessels
The timing of the MR image after gadolinium injection but also the dosages of gadolinium have been evaluated to detect active lesions in patients with multiple sclerosis [5]. A delay of 5 min after the injection of gadolinium increased the detection of blood-brain barrier permeability related to active lesions. At this time, gadolinium leaves the arterial vessels and goes in the capillaries and veins or in the parenchymal brain when the blood-brain barrier is disrupted. In healthy patients, when the imaging protocol of multiple sclerosis (MS) is used, PCGE are sometimes seen. Physiologic PCGE usually follow the anatomical arrangement of the deep medullary veins that run perpendicular to the long axis of the lateral ventricles and converge toward the fourth ventricle at the level of the brachium pontis [6]. Deep medullary veins are well recognized by SWI that uses desoxyhemoglobin as an intrinsic contrast agent. Physiologic PCGE are not associated with intraparenchymal hyperintensities on T2-weighted images (T2WI) and FLAIR (Fig. 1).
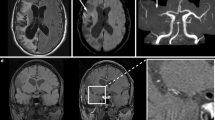
PCGE in absence of BBB breakdown. On axial contrast T1WI, physiologic PCGE follow the deep medullary veins (arrowheads) that run perpendicular to the long axis of the lateral ventricles (a) and converge toward the fourth ventricle (c). At the level of the brachium pontis, anterior transpontine vein is also seen (c, arrow). Axial FLAIR images reveal no abnormality (b, d). Punctate enhancements on axial contrast T1WI represent lenticulostriate collateral vessels in Moyamoya syndrome (arrowheads, e). In the corresponding area, axial FLAIR reveals no hyperintensity (f). Axial T2WI shows curvilinear hypointensities related to collateral moyamoya vessels (arrowheads, g). MRA discloses narrowing of the distal internal carotid arteries (arrowheads, h). Axial contrast T1WI show multiple curvilinear enhancements (i, j) occurring in the setting of straight sinus thrombosis, as seen on sagittal contrast T1WI (k, arrowhead), complicated by bithalamic infarction on axial FLAIR image (l)
Small collateral artery network related to Moyamoya syndrome
Moyamoya syndrome (including Moyamoya disease and secondary Moyamoya) is defined by a narrowing of the distal internal carotid artery accompanied by the development of collateral vessels. This additional network of perforating medullary artery collaterals (i.e. enlarged lenticulostriate, thalamoperforator, anterior and posterior choroidal arteries) may appear as punctate gadolinium enhancements [7]. Since the BBB is not disrupted, there is no parenchymal hyperintensity on T2WI and FLAIR in the vicinity of punctate enhancements (Fig. 1).
Enlarged small vessels related to developmental or acquired venous drainage disturbance
PCGE could correspond to the congestion of the deep medullary veins and/or the brainstem and cerebellum veins secondary to venous outflow disturbances. Acquired venous drainage failure could be caused by extensive dural sinus thrombosis (Fig. 1), arteriovenous malformations, dural arteriovenous fistula, and in the setting of high-grade glioma. Parenchymal hyperintensities on T2WI and FLAIR are only seen if venous congestions are complicated by oedema or ischemia [6].
Vascular malformations without arteriovenous shunt, such as capillary telangiectasia and developmental venous anomaly (where curvilinear enhancements take the form of caput medusa) could also exhibit PCGE. These malformations are particularly well visualized on T2-weighted gradient echo sequences and SWI. Aggressive course is rarely seen but remains possible.
Small vessels blood-brain barrier disruption
PCGE may be seen when the BBB of the small vessels is disrupted either by a direct injury of the endothelial cells or by an angiocentric infiltrates composed of various combinations of T lymphocytes (CD4 or CD8), B lymphocytes, and histiocytes (CD1 or CD68). Because the BBB breakdown, hyperintensities on T2WI and FLAIR are systematically seen in the corresponding areas of PCGE.
In each disease presented here, morphology of characteristic lesions other than PCGE will be described. Since these lesions are usually iso or hypointense on T1WI, and hyperintense on T2WI, FLAIR, and diffusion-weighted images (DWI), with either increased or decreased diffusion (according to their inflammatory or vascular mechanism, respectively), only unusual imaging pattern will be specified (e.g. hyperintensities on nonenhanced T1WI, inflammatory lesions with restricted diffusion, hyposignal on T2 gradient echo-weighted images).
Endotheliopathies
Posterior reversible encephalopathy syndrome, Susac syndrome, and endothelial cell injuries related to radiochemotherapy will be described in this section.
Posterior reversible encephalopathy syndrome
Posterior reversible encephalopathy syndrome (PRES) may occur in the setting of acute hypertension (including preeclampsia/eclampsia) and in many other conditions such as thrombotic microangiopathy, bone marrow and solid organ transplantations, sepsis, autoimmune diseases, and after immunosuppressive drugs or chemotherapy administration. Since the description of normotensive PRES cases, the hyperperfusion theory related to severe hypertension overwhelming the limits of autoregulation resulting in vasogenic oedema is challenging. Recent studies suggest that the damage of the endothelial cells could be the first event, resulting in the following pathophysiological cascade: release of endothelin, vasoconstriction, cerebral hypoperfusion, and eventually subsequent release of vascularendothelial growth factor leading to vasogenic oedema [8]. PRES is characterized by symptoms including headache, seizure, visual disturbances, and consciousness impairment, together with a typical cortical and subcortical vasogenic oedema involving the watershed areas of the brain (including mainly parietooccipital areas, superior frontal sulcus, inferior temporal regions, and cerebellum). Vasospams may be seen on MRA and concern usually distal second- and third-order branches of the posterior and anterior cerebral circulations. Once the underlying cause is removed, clinical and radiological signs are usually reversible. Diffusion restriction, haemorrhage, and gadolinium enhancements may occur and are associated with poorer outcome. Enhancing lesions are usually punctate (Fig. 2) and/or patchy and indicate a BBB disruption related to endothelial cell injuries.
PCGE with BBB breakdown related to endotheliopathies. Punctate enhancements in the setting of PRES are seen on axial contrast T1WI (a). In the corresponding areas, confluent hyperintensities are present on axial FLAIR (b) together with vasogenic oedema on ADC map (c). In a patient with Susac syndrome, axial contrast T1WI shows cerebellar punctate enhancements (d) matching with small foci hyperintensities on axial FLAIR (e). Sagittal T2WI discloses multiple punctate hyperintensities involving the corpus callosum (f). Sagittal (g) and axial (h) contrast T1WI reveal PCGE related to neovessels in the setting of glioblastoma progressing under antiangiogenic agents. On axial FLAIR, confluent hyperintensities in the vicinity of PCGE suggest that these neovessels have a weak BBB (i), as seen on brain biopsy (data not shown)
Susac syndrome
Besides PRES, punctate enhancing lesions could be observed in Susac syndrome.
Susac syndrome is characterized by a microangiopathy involving the precapillary arterioles. This syndrome is considered as an autoimmune endotheliopathy rather than a vasculitis, since histological findings show arteriolar occlusion without necrotizing vasculitis and absence of (or minimal) perivascular lymphocytic infiltrates. The brain, inner ear, and retina could be affected leading to encephalopathy, sensorineuronal hearing loss, and branch retinal artery occlusion, respectively. On MRI, lesions are usually small (3 to 7 mm), multiple, sometimes confluents (termed “snowball”), and involve the white and the grey matters of both the supratentorial and infratentorial areas. Corpus callosum is systematically involved, especially the central fibers suggesting an arteriolar distribution of the lesions. After gadolinium injection, up to 70 % of the parenchymal lesions enhance, with most often a miliary punctate aspect (Fig. 2) [9]. Less frequently, leptomeningeal enhancement could be also observed. Since the diameter of the involved arterioles is under 0.1 mm, conventional angiography is almost always normal.
Endothelial cell injuries related to radiochemotherapy
At last, PCGE could be seen in the setting of radiochemotherapy. Radiotherapy can induce acute and delayed injuries of the meningothelial, glial, and endothelial cells. Cryptic vascular malformations (e.g. capillary telangiectasias), vasculitis, and Moyamoya could account for the presence of PCGE in the setting of radiotherapy. As described above, chemotherapy could be complicated by a PRES and subsequent PCGE. Finally, punctate contrast enhancements have been described in patients with glioblastoma progressing under antiangiogenic agents (Fig. 2). Punctate enhancing lesions in this subset of glioblastoma patients may indicate neovascularization and/or endothelial cell injuries related to radiochemotherapy.
Disorders associated with angiocentric infiltrates
In this section, inflammatory diseases (including connective tissue diseases, sarcoidosis, hystiocytosis, and vasculitis), primary demyelinating diseases (i.e. acute demyelinating encephalomyelitis, multiple sclerosis, and neuromyelitis optica spectrum disorders), host immune responses, lymphoma, and CLIPPERS will be discussed successively.
Connective tissue diseases
Among the connective tissue diseases, neurological involvement has been mainly described in systemic lupus erythematosus (SLE). SLE could involve almost all parts of the central and peripheral nervous system with a prevalence of 25–70 %. CNS involvement in SLE could be due to neuronal dysfunction and/or direct parenchymal injuries. In neuronal dysfunction, brain MRI is often normal (up to 42 % of cases) or reveals diffuse cortical grey matter lesions suggesting postseizure changes or specific antineuronal antibody-mediated encephalitis. Direct parenchymal injuries may be due to (1) immune-mediated endothelial cell proliferation leading to occlusive vasculopathy, (2) immune complex-mediated perivascular lymphocytic infiltrates and less likely necrotizing vasculitis involving the small-sized (rather than the medium-sized) vessels, (3) aquaporin-4 antibodies complicated by neuromyelitis optica disease (refer to demyelinating diseases section), (4) arterial and/or venous thrombosis related to antiphospholipid antibodies, (5) thrombotic microangiopathy complicated by microvascular thrombosis and sometimes PRES, (6) embolism from Libman-Sacks endocarditis, (7) accelerated atherosclerosis due to the SLE itself, (8) comorbidities such as migraine and hypertension, and eventually (9) iatrogenic complications of steroid therapy and immunosuppressive drugs (e.g. PRES, progressive multifocal leukoencephalopathy, CNS lymphoma). Among these several mechanisms of parenchymal lesions, noninflammatory small-vessel vasculopathy but also vasculitis extending from small- to medium-sized vessels (with rarely Moyamoya imaging patterns), PRES, and finally dural venous thrombosis may account for PCGE in SLE (Fig. 3) [10]. In the other connective tissue diseases (e.g. Sjögren’s syndrome), PCGE are mainly caused by secondary vasculitis (refer to vasculitis section).
PCGE with BBB breakdown related to angiocentric cellular infiltrates (set 1). In SLE patient, a punctate enhancement is seen on axial contrast T1WI (a, arrowhead). Hyperintensity in the corresponding area is indicated by arrowhead on axial FLAIR image (b) and sagittal T2WI (c). In neurosarcoidosis patient, sagittal (d) and axial (e) contrast T1WI show disease extension along the leptomenigeal spaces where multiple punctate, patchy, and nodular enhancements are found. Cortical punctate enhancement (e, arrowhead) is associated with hyperintensity on axial FLAIR (f, arrowhead). In the setting of Hand-Schüller-Christian disease, axial contrast T1WI discloses brainstem punctate enhancement (arrow, g) matching with hyperintensity on axial FALIR (arrow, h). Sagittal contrast T1WI reveals thickened enhancing pituitary stalk (i)
Sarcoidosis
Sarcoidosis is a systemic inflammatory granulomatous disease of unknown origin. In the setting of systemic sarcoidosis, clinical neurologic involvement occurs in about 5 % of cases, while only 1 % of cases have isolated neurosarcoidosis. Therefore, histologic evidence of non-caseating granulomas is usually made in extra-neurologic organs. Neurosarcoidosis could involve all parts of the central and peripheral nervous systems. MRI could reveal (1) extra-axial changes (including epidural and subdural meninges), (2) lesions of structures without BBB (i.e. ependyma, choroid plexuses, pineal gland, pituitary stalk, optic chiasm, cranial nerves, and nerve roots), and (3) parenchymal involvement. Parenchymal lesions could result from disease extension along the cerebrospinal fluid pathways (i.e. through leptomenigeal and/or subependymal spaces) or related to haematogenous dissemination after blood-brain barrier disruption. Spectrum of the brain, hindbrain, and spinal cord lesions is very wide, including small lesions, vasculatic infarct, and tumour-like lesions. Small lesions may involve the whole-brain white matter, the cortex, and the deep grey matter. After gadolinium administration, some of these lesions could have patchy, nodular, or punctate enhancements (Fig. 3). Punctate enhancements may correspond to lymphohistiocytic perivascular infiltrates associated with non-caseating granulomas involving small arteries and/or small veins, as seen on brain biopsy [11].
Histiocytosis
Hitiocytosis defined by histiocytic proliferation is classified as either Langerhans cell histiocytosis (LCH) when immunostaining reveal the presence of CD1a-positive cells on biopsy, or non-Langerhans cell histiocytosis (NLCH) with or without hemophagocytosis when only CD68-positive cells are seen. Almost any organs could be affected by histiocytosis. We exposed herein histiocytosis among which PCGE have been described. Hand-Schüller-Christian disease is a LCH that usually occurs in childhood, while Erdheim-Chester disease is a NLCH without hemophagocytosis that starts in adulthood. Besides bones involvement (including paranasal sinus and orbital lesions), these two sporadic diseases could affect the same neurological compartments and share some radiological features with sarcoidosis. MRI findings could reveal (1) extra-axial changes (including epidural and subdural meninges), (2) hypothalamic-pituitary region and circumventricular organs (e.g. pineal gland and area postrema), and (3) parenchymal changes involving not only the white matter of the brainstem, the cerebellum, and the periventricular areas but also the grey matter such as dentate nucleus, and basal ganglia. PCGE are related to BBB disruption by perivascular histiocytosis infiltrates (Fig. 3) [12, 13].
Another NLCH with hemophagocytic syndrome, a life-threatening disease, could occur in conditions resulting in secretion of inflammatory cytokines including macrophage colony stimulating factor. Leptomeningeal enhancements and intraparenchymal PCGE associated with diffuse white matters changes throughout the brain and the spinal cord could be seen. PCGE likely reflect the presence of perivascular infiltration by lymphocytes and hemophagocytic histiocytes, while white matter lesions presumed to be caused by secondary demyelination [14].
Vasculitis
Arteritis of the CNS could result from secondary vasculitis (triggered by numerous causes), systemic primary vasculitis, and primary arteritis of the CNS (PACNS). According to the second International Chapel Hill Consensus Conference, PACNS is ranged into the single-organ vasculitis [15]. Diagnosis of PACNS is certain when brain biopsy shows vascular and perivascular inflammatory infiltrates together with fibrinoid necrosis of the medium (diameter between 0.08 and 0.25 mm) and/or the small (diameter <0.08 mm) vessels. However, since vasculitis lesions are segmental and focal, brain biopsy is most often either normal or displays non-specific inflammatory infiltrates. Although conventional angiography is considered as the gold standard, numerous differential diagnoses involving the vessel wall and/or the vessel lumen could mimic vasculitis-imaging patterns and exhibit multiple stenosis and dilations. In addition, a subset of medium-vessel vasculitis and all small-vessel vasculitis are not detected by conventional angiography because its resolution cannot reach vessels of diameter less than 0.2 mm. Therefore, the diagnosis of PACNS with certainty is rarely achieved. According to the size and the nature (i.e. artery or vein) of the involved vessels, MRI could display one pattern or different combinations including territorial infarctions, watershed ischemia, lacunar infarcts, tumour-like lesions, intraparenchymal haematoma, microbleeds, venous thrombosis, and spinal cord lesions. After gadolinium administration, pachymeningeal, leptomeningeal, gyral, patchy, nodular and punctate, and curvilinear enhancements may be observed. In the setting of secondary vasculitis and systemic primary vasculitis, PCGE could result from BBB disruption caused by small vessel inflammatory infiltrates or PRES. In addition, PCGE could be due to secondary Moyamoya (e.g. periarteritis nodosa) or venous thrombosis (e.g. Behçet disease) [16]. In PACNS, PCGE are mainly due to small vessel BBB disruption (Fig. 4). Interestingly, in cerebral amyloid angiopathy-related inflammation, a subset of PACNS, PCGE are not usually seen. MRI shows more likely large confluent cortical and subcortical lesions, spreading beyond the vascular boundaries, together with microbleeds and leptomeningeal enhancements [17].
PCGE with BBB breakdown related to angiocentric cellular infiltrates (set 2). In PACNS patient, axial contrast T1WI of the brain (a) and sagittal contrast T1WI of the spinal cord (c) show multiple punctate enhancements matching with hyperintensities in the corresponding areas on axial FLAIR (b) and sagittal T2WI (d), respectively. On axial contrast T1WI, in addition to nodular enhancing lesions, some punctate enhancements (e) are seen in ADEM patient. On axial T2WI, hyperintensities match with all enhancing lesions (f). Sagittal T2WI of the spinal cord shows concomitant longitudinally extensive transverse myelitis (g). In MS patient, punctate lesions are seen on axial contrast T1WI (h) but not on axial non-contrast T1WI (i). These enhancing lesions match with hyperintensities on axial FLAIR (j)
Demyelinating diseases
CNS demyelination is related to oligodendrocyte damages with relative axonal preservation. Mechanisms of oligodendrocyte dysfunction or destruction are numerous and could be inherited or acquired. Here, we discuss autoimmune demyelinating diseases including acute demyelinating encephalomyelitis (ADEM), MS, and neuromyelitis optica spectrum disorders (NMOSD).
ADEM is a usually monophasic and multifocal disease, triggered by viral infection or vaccination. Lesions could involve the brain, brainstem, cerebellum, optic nerve, and spinal cord. Morphologies vary from small punctate lesions to large tumour-like lesions, which have less mass effect than expected for their size. The white matter, except the callososeptal interface, is typically affected, and the basal ganglia, thalamus, and even cortical grey matter may be involved. Rarely, haemorrhagic lesions could be seen and are related to necrotizing vasculitis of venules. After gadolinium administration, all (or almost all) lesions are enhanced. Not only closed or open ring enhancements but also PCGE could be seen (Fig. 4). Enhancing lesions are related to BBB disruption and correspond to perivenous lymphocytic infiltrates accompanied by demyelinating lesions [18].
MS is the most common CNS autoimmune disorder. According to its patterns of progression, four main phenotypes have been described including relapsing-remitting, secondary progressive, primary progressive, and progressive relapsing. Lesions have usually a linear or ovoid appearance and involve predominantly the juxtacortical and periventricular white matter, the callososeptal interface along the deep medullary veins (“Dawson fingers”), the middle cerebellar peduncles, the optic nerve, and the ascending and descending tracts of the spinal cord. In the acute stage, some lesions could have restricted diffusion. After gadolinium administration, only the recent lesions (less than 6 months) enhanced. Characteristic open ring, but also closed ring, nodular, and rarely punctate enhancements (Fig. 4) have been described [19]. Enhancing lesions are related to BBB breakdown and active demyelination. Active plaques are characterized by perivenous inflammatory infiltrates, with predominantly T cells, together with confluent demyelinating lesions, foamy macrophages, and subsequent glial scar tissue. Hyperintense lesions on nonenhanced T1WI could also be observed in MS. Since the size of these lesions ranges between 2 and 20 mm in diameter, these hyperintensities could be misdiagnosed with PCGE. The underlying pathophysiology of these lesions remains undetermined.
Neuromyelitis optica (NMO, or Devic disease) is usually a relapsing remitting disease characterized by severe attacks of optic neuritis, longitudinally extensive transverse myelitis (i.e. lesion extending over 3 or more vertebral segments), and presence of NMO-IgG in serum. NMO-IgG targets the water channel aquaporin-4 (AQP4). AQP4 is localized on astrocyte feet along the endothelial tight junctions at BBB of small vessels. AQP4 is found throughout in the brain, with highly expression in the optic nerves, spinal cord, and along the periependymal regions. Histological findings suggest that interaction between NMO-IgG and aquaporin-4 induces complement-dependent astrocyte cytotoxicity leading to leukocytes infiltrations, BBB disruption, and eventually destruction of the oligodendrocytes and neurons. Neurological phenotypes (e.g. encephalopathy, diencephalic syndrome, or brainstem symptoms) associated with NMO-IgG that do not meet NMO criteria are designed NMOSD. All parts of the CNS except the cortex could be affected and some of NMOSD patients fulfil the Barkhof criteria for dissemination in space. Three NMOSD characteristic imaging patterns have been described: (1) linear periependymal lesions, which could progress variably to adjacent structures; (2) contiguous lesions following the corticospinal tracts; and (3) extensive and confluent hemispheric white matter lesions (“spilled ink pattern”) with vasogenic oedema. After gadolinium administration, pencil-thin enhancement could be seen along the linear periependymal lesions, and cloud-like enhancement (patchy enhancement) is usually associated with extensive lesions. Leptomeningeal enhancement is less likely seen, and PCGE has been reported in only one NMO patient [20]. As described above, NMOSD could coexist with connective tissue diseases.
After review of the literature, PCGE have not been described as characteristic imaging pattern in the other demyelinating disorders including solitary sclerosis, atypical idiopathic inflammatory demyelinating lesions (i.e. ring-like, Balo-like, megacystic, infiltrative, and unclassified lesions), and combined central and peripheral demyelination. The strict delimitation between all these demyelinating disorders is not well defined. In addition, their correlation with specific autoantibodies targeting CNS autoantigens (e.g. myelin-oligodendrocyte glycoprotein, neurofascin, and glycine receptor alpha1 subunit) remains to be determined.
Host immune responses
PCGE could be seen when host immune response is fighting against infectious disease or against the emergence of lymphoma.
Host immune response in the setting of infectious disease
Immune reconstitution inflammatory syndrome (IRIS) is characterized by a prompt immune restoration leading to an exaggerated inflammatory response against active or latent opportunistic infections. Mainly described in the setting of HIV immunosuppression after anti-retroviral therapy initiation, IRIS could also occur after removal of required immunosuppressive drugs (e.g. natalizumab in MS) or when treatment of haematologic malignancies allowed to an immune restoration. IRIS can affect any organ of the body, including the CNS (CNS-IRIS). Among opportunistic infections, PCGE are mainly described when CNS-IRIS occurred in the setting of progressive multifocal leukoencephalopathy (PML) and cryptococcal meningitis [21, 22].
PML lesions are related to progressive demyelination due to JC virus. Brain MRI shows white matter lesions that predominantly involve the supratentorial areas. Initially focal and often subcortical (with U-fiber involvement), these lesions progress along the whole-brain white matter and become rapidly confluent. Diffusion restriction in the outer rim of the lesion indicates the active site of demyelination. By contrast to typical PML, PML-IRIS is characterised by the presence of enhancing lesions and oedema with mass effect. Enhancement may be punctuate, linear, or rim like (Fig. 5). PCGE are related to perivascular infiltration by CD8-positive T cells, which is considered as the pathological hallmark of IRIS.
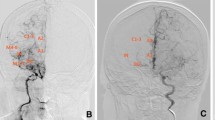
PCGE with BBB breakdown related to angiocentric cellular infiltrates (set 3). In MS patient after natalizumab withdrawal, axial contrast T1WI disclose multiple punctate enhancing lesions (a, c) matching with confluent hyperintensities on axial T2WI (b, d) that are characteristics of PML-IRIS. In HIV patient presenting with CD8 encephalitis, PCGE on axial (a) and coronal (c) contrast T1WI are associated with diffuse white matter lesions on axial and coronal FLAIR images, respectively (b, d). In a LYG, multiple PCGE on axial contrast T1WI involve the hindbrain (i) and the supratentorial areas (k), and match with hyperintensties on axial T2WI (j, l). By contrast to CLIPPERS, epicentre is localized in the genu of the corpus callosum and not in the brainstem
Cryptococcus neoformans mostly affects the lung and the CNS. After leptomeninges, the fungus spreads along the perivascular spaces (adjacent to the small perforating arteries) into the brain parenchyma. In absence of immune restoration, brain MRI could be normal or shows dilated perivascular spaces with basal ganglia pseudocyts (hyperintense on T2WI and hypointense in FLAIR). Less likely, intraparenchymal cryptococcomas (hyperintense on T2WI and FLAIR) could be seen. After immune restoration, enhancement of perivascular spaces with punctate appearance and enhancement of leptomeninges appear almost systematically. Hydrocephalus and brain infarctions could also be observed.
In HIV-infected patients, host immune response mediated by CD8-positive T cells may also affect the CNS in absence of opportunistic infections. Coined CD8 encephalitis, this HIV-driven complication may occur in the setting of immune restoration following combined antiretroviral therapy introduction or after transient HIV replication triggered by minor infection or antiretroviral therapy interruption. MRI indicates bilateral and diffuse lesions involving the white and grey matter in the supratentorial area. After gadolinium administration, PCGE are seen (Fig. 5). CSF analysis shows pleiocytosis with predominance of CD8-positive T cells and transient HIV replication. Massive perivascular infiltration by polyclonal CD8-positive T cells, astrocytic and microglial activation, and sometimes demyelinating features are present on brain biopsy [23]. Weak expression of HIV proteins together with the absence of multinucleated giant cells distinguishes this particular form of CD8 encephalitis from other HIV encephalitis. The precise mechanism of this steroid-responsive disorder remains to be determined.
Finally, schistosomiasis may involve occasionally the CNS in immunocompetent patients. Host granulomatous response around ectopic eggs (localized into the CNS) may lead to encephalitis and transverse myelitis. Central linear enhancement surrounded by multiple punctate nodules, which give an “arborized” appearance, together with vasogenic oedema has been described in the brain and the spinal cord. This unique imaging pattern constitutes a pathognomonic sign of CNS schistosomiasis [24]. Enhancing lesions may represent venous congestion and/or BBB disruption related to granuloma formation.
Host immune response fighting against lymphoma (prelymphoma states)
Pre-lymphoma states such as sentinel lesions of primary CNS lymphoma (PCNSL) and grade I lymphomatoid granulomatosis (LYG) may exhibit PCGE.
Sentinel lesions of PCNSL are symptomatic contrast enhancing mass lesions involving the CNS. Brain biopsy reveals perivascular infiltrates of CD4-positive lymphocytes with sometimes demyelinating features. These lesions recede spontaneously or after steroid therapy and precede the emergence of PCNSL by 1 year or less. It is suggested that sentinel lesions of PCNSL are host immune responses fighting against the lymphoma. Besides tumour-like appearance, MRI may also reveal PCGE and hyperintense lesions on T2WI and FLAIR in the corresponding areas. These gadolinium enhancements predominantly affect the brainstem and are related to perivascular infiltrates by polyclonal CD4-positive lymphocytes [25]. By contrast with its sentinel lesions, PCNSL is characterized by single or multiple mass-like lesion(s), involving mainly the periventricular white matter or the basal ganglia, and spreading along ependymal surfaces and/or the corpus callosum. Because of the high nuclear to cytoplasmic ratio and the high cellular density, lesions are iso-hypointense on T1WI and T2WI with restricted diffusion. Lesions have homogeneous enhancement in immunocompetent patients and peripheral enhancement with central necrosis in immunocompromised individuals.
LYG is an EBV-associated B cell lymphoproliferative disorder involving usually the lung, skin, and CNS. However, non-systemic form of LYG is described, and only one of these three organs could be affected. LYG is defined by an angiocentric infiltrate composed by polyclonal CD4-positive lymphocytes together with scattered B cells. In about half of patients, this benign entity (grade I LYG) may progress to a B cell lymphoma (grade II and III LYG), which is defined by the presence of large amount of EBV-positive atypical B cells and angiodestructive changes. Five MR imaging patterns are described: (1) infra and/or supratentorial PCGE involving the white and grey matter with punctate hyperintense lesions on T2WI and FLAIR; (2) brain masses with ring-like enhancement; (3) lacunar cerebral infarcts; (4) gadolinium enhancements along the CSF pathways including leptomeninges, cranial nerves, choroid plexus, and pituitary stalk; and (5) focal thickening and enhancement of the dura mater [26]. Finally, multiple arterial narrowing and aneurysm are demonstrated by using conventional angiography. In grade I LYG, hindbrain PCGE seems to be the mostly imaging pattern (Fig. 5) [27]. As sentinel lesions of PCNSL, grade I LYG could recede spontaneously or after steroid therapy.
Lymphoma
CNS involvement in the setting of systemic lymphoma may be due to parenchymal invasion either along the CSF pathways or after crossing the BBB, or related to nonmetastatic systemic effects (e.g. hemophagocytic syndrome, thrombotic microangiopathy with or without PRES, paraneoplastic syndromes, opportunistic infections). Non-Hodgkin’s systemic lymphoma can be revealed by multiple CNS PCGE, as reported in a case of marginal zone B cell lymphoma and more recently in a case of mantle cell lymphoma [28, 29]. Beside systemic lymphoma, PCNSL, LYG, and intravascular lymphoma (IVL) are the three main lymphomas involving exclusively or having a relative predilection for the CNS. As in sentinel lesions of the PCNSL, and grade I LYG (described above), PCGE could be seen in IVL.
IVL is a non-Hodgkin’s lymphoma, usually of B cell lineage, in which the malignant lymphocyte clone invades the lumen of small vessels (i.e. arterioles, capillaries, postcapillary venules) rather than medium vessels. Although a systemic disease, IVL involves predominantly the nervous system and the skin. Untreated IVL follows usually a relapsing-progressive clinical course with systematically a fatal outcome. Encephalopathy, focal neurological deficits, seizure, dementia, and less frequently myelopathy and cauda equina syndrome could be seen. Characteristic imaging patterns on MRI include the following: multiple infarct-like lesions throughout the brain with possible haemorrhagic transformations, white matter lesions involving periventricular areas and the pons, and mass-like lesions. Correlation between brain MRI features and pathological findings suggest that infarct-like lesions are related to small artery occlusions, whereas white matter abnormalities result from small vein occlusions. Mass-like lesions seem to be due to extravascular spread of lymphoma cells [30]. Rarely, spinal infarcts and extensive spinal cord lesions reveal IVL. Multiple arterial stenosis and dural sinus thrombosis are infrequently reported. In addition to extra-axial enhancements, involving the dura matter, leptomeninges, and roots, intra-parenchymal punctate, linear, nodular, and ring-like enhancing lesions are described [31]. PCGE in the setting of IVL could be due to small vein congestions, sluggish flow in small vessels, or BBB disruption resulting from vascular wall infiltrations by lymphoma cells.
Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids
Described in 2010, CLIPPERS is a steroid-sensitive and steroid-dependent relapsing-remitting brainstem disorder of unknown origin [2]. Core features of CLIPPERS include six criteria: (1) brainstem signs and symptoms; (2) PCGE predominantly involving the pons and the middle cerebellar peduncles; (3) a steroid sensitivity with possible clinical and radiological sequelae; (4) absence evidence of an alternative diagnosis; (5) a relapsing-remitting course in absence of immunosuppressive therapy with relapses matching with the four first criteria; and (6) a lymphohistiocytic infiltrate around and sometimes in the vessel walls on brainstem biopsy. Biopsy is not recommended (criterion 6) when the first four criteria are present at the first attack and when the fifth criterion exists during relapse(s). During attacks, cerebellar ataxia and diplopia are the most common signs. Besides brainstem, cerebellar, and cranial nerve symptoms/signs, spinal cord syndrome and cognitive dysfunction may be observed. Characteristic imaging features of CLIPPERS are defined by brainstem PCGE matching with hyperintensities in T2WI and FLAIR without mass effect. Although the epicentre is localized in the pons and in the middle cerebellar peduncles, these lesions may extend posteriorly to the cerebellum, rostrally to the supratentorial regions, and caudally to the spinal cord. In supratentorial area, deep grey matter (i.e. basal ganglia, thalami, hippocampus) and the whole-brain white matter (i.e. periventricular, deep, and juxtacortical white matter, and corpus callosum) could be involved. In the spinal cord, lesions could extend from the upper cervical levels to the conus (Fig. 6). The cerebral and cerebellar cortex, hypothalamic-pituitary axis, leptomeninges, and dura mater are not affected. In addition to classical punctate and curvilinear appearance, enhancements could be nodular and even rarely ring-like. Complete or marked clinical and radiological improvement after high doses of steroids is usually seen. However, disability and cognitive impairment associated with CNS atrophy (involving hindbrain and sometimes supratentorial areas and spinal cord) may be observed. Following imaging features should be considered as “red flags”: diffusion restriction, marked vasogenic oedema, tumour-like lesion with mass effect, absence or mild radiological response to steroids, another epicentre than pons or brachium pontis, intraparenchymal haemorrhage, and abnormal cerebral angiography.
PCGE in the setting of CLIPPERS. On axial (a) and coronal (c) contrast T1WI, PCGE involve mainly the pons and the middle cerebellar peduncles and diffuse rostrally into the supratentorial areas (e), and caudally into the cervical spinal cord (g). These lesions match with hyperintensities in the corresponding areas on axial (b, f) and coronal T2WI of the brain (d) and sagittal T2WI of the spinal cord (h)
Brainstem PCGE are related to perivascular and transmural inflammatory infiltrates involving the small vessels of the white and grey matter. These angiocentric infiltrates are composed predominantly of CD4-positive T cells and histiocytes. Small number of EBV-negative B cells is also present [4, 32].
After the description of CLIPPERS, brainstem PCGE have been reported in several diseases such as glioma, sentinel lesions of PCNSL, grade I LYG, mantle cell lymphoma, primary-CNS vasculitis, and MS. Except for glioma, all these diseases respond to high doses of steroids (at least initially), have a relapsing-remitting course (requiring immunosuppressive therapy), and exhibit on brainstem biopsy histological features compatible with CLIPPERS. However, unlike CLIPPERS, brainstem is not systematically affected at each relapse and lesion distribution does not remain concentrated in the pons. Therefore, the fifth criterion seems to be the most robust for the diagnosis of CLIPPERS. However in absence of specific biologic or histologic markers, it is always unknown if CLIPPERS is a new disorder, a syndrome, or a prestage of well-determined disease. In this later issue, distinction between CNS grade I LYG and CLIPPERS is particularly challenging.
Punctuate and curvilinear enhancing lesions, a practical approach
Before considering intra intraaxial PCGE, two differential diagnoses must be excluded: (1) extraaxial PCGE related to leptomeningeal enhancements following the cerebellar folia and the cerebral sulci; and (2) punctate hyperintense lesions on nonenhanced T1WI (usually seen in MS). Once the diagnosis of intraaxial PCGE is confirmed, clinical context together with cerebral vascular imaging and FLAIR and T2WI are necessary to distinguish physiological from pathological PCGE.
Physiologic PCGE usually follow the anatomical arrangement of the deep medullary veins that run perpendicular to the long axis of the lateral ventricles and converge toward the fourth ventricle at the level of the brachium pontis. Cerebral imaging of venous and arterial flow is normal, and T2/FLAIR images show no abnormality in the corresponding regions of PCGE.
After ruling out a physiologic PCGE, intraaxial PCGE could be seen in three situations: (1) new arteriolar network of collateral vessels in the setting of Moyamoya, (2) small vessels enlargement related to developmental or acquired venous drainage disturbances, and (3) in BBB disruption of the small vessels.
In the situations 1 and 2, since the BBB is usually unspoiled, T2/FLAIR images reveal no abnormality in the corresponding areas of PCGE. The localization of PGCE matches with either the perforating arteries in Moyamoya or the anatomy of the venous system in case of venous congestion. In addition, vascular imaging (e.g. ARM, VRM, CT angiography, conventional angiography) reveals the presence of distal internal carotid stenosis in Moyamoya and shows venous outflow disturbances when developmental or acquired venous anomalies are present.
In the situation 3, as the BBB is disrupted, PCGE are accompanied by small foci of T2/FLAIR hyperintensity. In this third situation, medical history, clinical symptoms/signs, and radiological findings help to discern endotheliopathies (i.e. PRES, Susac syndrome, and radiochemotherapy-induced injuries) from disorders associated with angiocentric infiltrates. Disorders associated with perivascular infiltrates include infectious diseases complicated by secondary vasculitis and/or host immune response, inflammatory autoimmune diseases (i.e. connective tissue diseases, sarcoidosis, histiocytosis, vasculitis, and demyelinating diseases), prelymphoma states (i.e. sentinel lesions of PCNSL and grade I LYG), non-Hodgkin lymphoma (i.e. mantle cell, marginal zone B cell and intravascular lymphomas), and CLIPPERS. Since all of these diseases require immunosuppressive therapies, it is necessary to exclude infectious diseases. Extensive investigations, including routine blood tests, serological tests for infectious and autoimmune diseases, LDH levels, CSF analysis, salivary gland biopsy, cerebral angiography, bone marrow biopsy, and whole body PET scan are often essential to reach the diagnosis. Brain biopsy should be performed when all investigations remain inconclusive and when CLIPPERS criteria are not fitted (Fig. 7).
Punctuate and curvilinear enhancing lesions, a practical approach. (single asterisk) Vascular imaging: ARM, VRM, CT angiography, conventional angiography. (double asterisks) Extensive investigations: routine blood tests, serological tests for infectious and autoimmune diseases, CSF analysis, salivary gland biopsy, cerebral angiography, bone marrow biopsy, and whole body PET scan. (Triple asterisks) CLIPPERS criteria: (1) brainstem signs/symptoms; (2) PCGE involving predominantly the pons and the middle cerebellar peduncles; (3) steroid sensitivity; (4) absence of alternative diagnosis; (5) a relapsing-remitting course with relapses matching with the four first criteria; and (6) perivascular lymphohistiocytic infiltrates on brainstem biopsy. Biopsy is not recommended (criterion 6) when the first four criteria are present at the first attack and when the fifth criterion exists during relapse(s)
Key Points |
1. PCGE without FLAIR hyperintensities in the corresponding areas suggest intact BBB: |
Other MRI sequences are usually able to distinguish physiological from pathological conditions. |
2. PCGE with FLAIR hyperintensities in the corresponding areas indicate BBB disruption: |
Medical history, clinical presentations, other MRI sequences, and sometimes investigations such as serological tests for infectious and autoimmune diseases, LDH levels, CSF analysis, salivary gland biopsy, retinal angiography, cerebral angiography, bone marrow biopsy, and whole body PET scan are necessary to reach the diagnosis. |
Brain biopsy should be reserved for specific situations: |
1. Isolated CNS involvement with normal investigations. |
2. Disorders presenting with atypical CLIPPERS findings at the initial presentation or during the follow-up suggestive alternative diagnoses (e.g. CNS lymphoma, CNS vasculitis). |
Abbreviations
- DWI:
-
Diffusion-weighted images with increased
- ADC:
-
Apparent diffusion coefficient
- BBB:
-
Blood-brain barrier
- MRI:
-
Magnetic resonance imaging
- PCGE:
-
Punctate and curvilinear gadolinium enhancements
- SWI:
-
Susceptibility-weighted imaging
- T1WI:
-
T1-weighted images
- T2WI:
-
T2-weighted images
- PRES:
-
Posterior reversible encephalopathy syndrome
- SLE:
-
Systemic lupus erythematosus
- LCH:
-
Langerhans cell histiocytosis
- NLCH:
-
Non-Langerhans cell histiocytosis
- PCACNS:
-
Primary arteritis of the CNS
- ADEM:
-
Acute demyelinating encephalomyelitis\
- MS:
-
Multiple sclerosis
- NMOSD:
-
Neuromyelitis optica spectrum disorders
- IRIS:
-
Immune reconstitution inflammatory syndrome
- PML:
-
Progressive multifocal leukoencephalopathy
- PCNSL:
-
Primary CNS lymphoma
- LYG:
-
Lymphomatoid granulomatosis
- IVL:
-
Intravascular lymphoma
- CLIPPERS:
-
Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids
References
Carr JC, Carroll TJ (eds) (2012) Magnetic resonance angiography, principles and applications. Springer, New York, pp 215–216
Pittock SJ, Debruyne J, Krecke KN et al (2010) Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS). Brain 133:2626–2634
Tateishi U, Terae S, Ogata A, Sawamura Y, Suzuki Y, Abe S, Miyasaka K (2001) MR imaging of the brain in lymphomatoid granulomatosis. AJNR Am J Neuroradiol 22:1283–1290
Taieb G, Duflos C, Renard D et al (2012) Long-term outcomes of CLIPPERS (chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids) in a consecutive series of 12 patients. Arch Neurol 69:847–855
Uysal E, Erturk SM, Yildirim H et al (2007) Sensitivity of immediate and delayed gadolinium-enhanced MRI after injection of 0.5 M and 1.0 M gadolinium chelates for detecting multiple sclerosis lesions. AJR Am J Roentgenol 188:697–702
Friedman DP (1997) Abnormalities of the deep medullary white matter veins: MR imaging findings. AJR Am J Roentgenol 168:1103–1108
Komiyama M, Nakajima H, Nishikawa M et al (2001) Leptomeningeal contrast enhancement in moyamoya: its potential role in postoperative assessment of circulation through the bypass. Neuroradiology 43:17–23
Bartynski WS (2008) Posterior reversible encephalopathy syndrome, part 2: controversies surrounding pathophysiology of vasogenic edema. AJNR Am J Neuroradiol 29:1043–1049
Susac JO, Murtagh FR, Egan RA et al (2003) MRI findings in Susac’s syndrome. Neurology 61:1783–1787
Jennings JE, Sundgren PC, Attwood J et al (2004) Value of MRI of the brain in patients with systemic lupus erythematosus and neurologic disturbance. Neuroradiology 46:15–21
Christoforidis GA, Spickler EM, Recio MV et al (1999) MR of CNS sarcoidosis: correlation of imaging features to clinical symptoms and response to treatment. AJNR Am J Neuroradiol 20:655–669
Prayer D, Grois N, Prosch H et al (2004) MR imaging presentation of intracranial disease associated with Langerhans cell histiocytosis. AJNR Am J Neuroradiol 25:880–891
Sedrak P, Ketonen L, Hou P et al (2011) Erdheim-Chester disease of the central nervous system: new manifestations of a rare disease. AJNR Am J Neuroradiol 32:2126–2131
Forbes KP, Collie DA, Parker A (2000) CNS involvement of virus-associated hemophagocytic syndrome: MR imaging appearance. AJNR Am J Neuroradiol 21:1248–1250
Jennette JC, Falk RJ, Bacon PA et al (2013) 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum 65:1–11
Chenevier F, Renoux C, Marignier R et al (2009) Primary angiitis of the central nervous system: response to mycophenolate mofetil. J Neurol Neurosurg Psychiatry 80:1159–1161
Sakaguchi H, Ueda A, Kosaka T et al (2011) Cerebral amyloid angiopathy-related inflammation presenting with steroid-responsive higher brain dysfunction: case report and review of the literature. J Neuroinflammation 8:116
Young NP, Weinshenker BG, Parisi JE et al (2010) Perivenous demyelination: association with clinically defined acute disseminated encephalomyelitis and comparison with pathologically confirmed multiple sclerosis. Brain 133:333–348
Guttmann CR, Ahn SS, Hsu L et al (1995) The evolution of multiple sclerosis lesions on serial MR. AJNR Am J Neuroradiol 16:1481–1491
Pekcevik Y, Izbudak I (2015) Perivascular enhancement in a patient with neuromyelitis optica spectrum disease during an optic neuritis attack. J Neuroimaging 25:686–687
Post MJ, Thurnher MM, Clifford DB et al (2013) CNS-immune reconstitution inflammatory syndrome in the setting of HIV infection, part 1: overview and discussion of progressive multifocal leukoencephalopathy-immune reconstitution inflammatory syndrome and cryptococcal-immune reconstitution inflammatory syndrome. AJNR Am J Neuroradiol 34:1297–1307
Wattjes MP, Verhoeff L, Zentjens W et al (2013) Punctate lesion pattern suggestive of perivascular inflammation in acute natalizumab-associated progressive multifocal leukoencephalopathy: productive JC virus infection or preclinical PML-IRIS manifestation? J Neurol Neurosurg Psychiatry 84:1176–1177
Lescure FX, Moulignier A, Savatovsky J et al (2013) CD8 encephalitis in HIV-infected patients receiving cART: a treatable entity. Clin Infect Dis 57:101–108
Sanelli PC, Lev MH, Gonzalez RG et al (2001) Unique linear and nodular MR enhancement pattern in schistosomiasis of the central nervous system: report of three patients. AJR Am J Roentgenol 177:1471–1474
Taieb G, Uro-Coste E, Clanet M et al (2014) A central nervous system B-cell lymphoma arising two years after initial diagnosis of CLIPPERS. J Neurol Sci 344:224–226
Patsalides AD, Atac G, Hedge U et al (2005) Lymphomatoid granulomatosis: abnormalities of the brain at MR imaging. Radiology 237:265–273
De Graaff HJ, Wattjes MP, Rozemuller-Kwakkel AJ et al (2013) Fatal B-cell lymphoma following chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids. JAMA Neurol 70:915–918
Epaliyanage P, King A, Hampton T, Gullan R, Ashkan K (2014) “Brain on fire”: a new imaging sign. J Clin Neurosci 21:2015–2017
Faivre G, Lagarde J, Choquet S et al (2014) CNS involvement at diagnosis in mantle cell lymphoma with atypical MRI features. J Neurol 261:1018–1020
Yamamoto A, Kikuchi Y, Homma K et al (2012) Characteristics of intravascular large B-cell lymphoma on cerebral MR imaging. AJNR Am J Neuroradiol 33:292–296
Liow K, Asmar P, Liow M et al (2000) Intravascular lymphomatosis: contribution of cerebral MRI findings to diagnosis. J Neuroimaging 10:116–118
Simon NG, Parratt JD, Barnett MH et al (2012) Expanding the clinical, radiological and neuropathological phenotype of chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS). J Neurol Neurosurg Psychiatry 83:15–22
Acknowledgments
We want to especially thank Mr Benjamin Taieb for his help in figure design.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
We declare that this manuscript does not contain clinical studies. Anonymized data with a number were used to develop a practical approach.
Conflict of interest
We declare that we have no conflict of interest.
Rights and permissions
About this article
Cite this article
Taieb, G., Duran-Peña, A., de Chamfleur, N.M. et al. Punctate and curvilinear gadolinium enhancing lesions in the brain: a practical approach. Neuroradiology 58, 221–235 (2016). https://doi.org/10.1007/s00234-015-1629-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-015-1629-y