Abstract
Introduction
Apparent diffusion coefficient (ADC) values in the developing fetus can be used in the diagnosis and prognosis of prenatal brain pathologies. To this end, we measured regional ADC in a relatively large cohort of normal fetal brains in utero.
Methods
Diffusion-weighted imaging (DWI) was performed in 48 non-sedated 3rd trimester fetuses with normal structural MR imaging results. ADC was measured in white matter (frontal, parietal, temporal, and occipital lobes), basal ganglia, thalamus, pons, and cerebellum. Regional ADC values were compared by one-way ANOVA with gestational age as covariate. Regression analysis was used to examine gestational age-related changes in regional ADC. Four other cases of CMV infection were also examined.
Results
Median gestational age was 32 weeks (range, 26–33 weeks). There was a highly significant effect of region on ADC, whereby ADC values were highest in white matter, with significantly lower values in basal ganglia and cerebellum and the lowest values in thalamus and pons. ADC did not significantly change with gestational age in any of the regions tested. In the four cases with fetal CMV infection, ADC value was associated with a global decrease.
Conclusion
ADC values in normal fetal brain are relatively stable during the third trimester, show consistent regional variation, and can make an important contribution to the early diagnosis and possibly prognosis of fetal brain pathologies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Diffusion-weighted imaging (DWI) is gaining ground in developmental studies of the human brain in vivo, specifically with regard to myelination [1]. Maturational changes in diffusion indices in healthy fetuses are thought to be related to the development of the myelin sheath [2–7], which proceeds from primary cortices to secondary cortices and to associative cortices. These processes have been intensely studied in postmortem tissue [8]. There is a growing need for a comprehensive in vivo database of apparent diffusion coefficient (ADC) values in different brain regions of the developing fetus, which can be used in the diagnosis and prognosis of prenatal brain pathologies.
In the present study, we measured ADC in several brain regions of a relatively large cohort (N = 48) of non-sedated healthy fetuses and compared them to four cases of congenital CMV infection scanned at similar gestational ages.
Subjects and methods
This is a prospective cohort study performed to establish normal values of the ADC of normal fetuses in relation to gestational age (GA).
Institutional review board approval was given.
Subjects
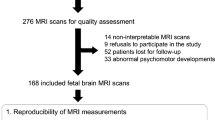
Forty-eight normal fetuses, scanned in our diagnostic imaging department in the years 2006–2012, gestational age (GA) from 26–33 weeks (mean GA 30 weeks, median 32 weeks) were included in the study. The indications for the MR scan were (1) normal ultrasound (US), but an abnormal outcome in previous pregnancies in siblings (n = 27); and (2) inconclusive findings in fetal neurosonography which were excluded by the MRI (N = 21) and by subsequent US scans (Table 1). Fetuses were considered normal if they had normal prenatal ultrasonographic results (group 1) or suspected sonographic findings, with subsequent normal fetal MR and US imaging results (group 2). Maternal disease and pregnancy complications as well as poor overall scan quality/motion artifacts were used as exclusion criteria. In eight cases, not all the regional values were obtained due to technical difficulties.
MRI
According to our MRI protocol, the mothers refrained from eating or drinking fluids with sugar 4 h before the MRI examination, which was performed without sedation. Scans were obtained using a 1.5 T MR system (GE Medial System, Milwaukee, WI). A single-shot fast spin echo (SSFSE) T2-weighted sequences in three orthogonal planes was employed with slice thickness of 3–4 mm, no gap, using a flexible coil (eight channels cardiac coil). The field of view was determined by the size of the fetal head and was 24 cm for smaller fetuses, up to 30 cm for the bigger fetuses. Other parameters were a matrix of 320/224, echo time (TE) of 90 ms, and repetition time (TR) of 1,298 ms. A FSPGR T1 sequence was performed only in the axial plane with a larger field of view of 40 cm, 4-mm slice thickness and .0.5-mm gap, and TR 160 and TE 2.3. Then, a DWI sequence in one to three orthogonal planes (axial coronal and sagittal planes) was performed with a 40-cm field of view, b value of 0 and 1,000 or 700 msec, slice thickness of 4 mm with no gap, and scan time of 56 s. The apparent diffusion coefficient (ADC) was calculated in each region of interest (ROI), using the functool software of the AD-HD work station (GE Medial System, Milwaukee, WI). A circular ROI was used, placed over the desired anatomical area.
ADC measurements
Fifteen circular regions of interest (ROIs) ranging in size from 62 to 104 mm2 (mean 83.22; SD 5.1) were placed as follows: two on each lobe (two frontal, two parietal, two temporal, two occipital), two on the basal ganglia, two on the thalami, and two on the cerebellar hemispheres. A single ROI was placed over the pons. Bilateral ROIs were averaged, resulting in eight values/fetus, which were averaged for each gestational age.
ADC measurements were also obtained in a subgroup of the CMV-infected fetuses previously described [9]. Four CMV-infected fetuses (GA range 30–33 weeks) were compared to a subgroup (N = 35) of the healthy fetuses in the same age range (i.e., fetuses <26 weeks old were not included in this analysis) using two-way analysis of variance (diagnosis × region). Two fetuses had a normal MR scan, one had an abnormal high signal in the white matter of the temporal lobes, in the anterior aspect of the lobes, and another fetus presented with multiple cystic periventricular lesions in the temporal and frontal lobes. The signal of the white matter of the temporal lobes was increased. There were no calcifications or other findings in these brains on US.
Results
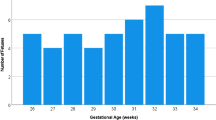
The characteristics of the individual subjects are summarized in Table 1. Fetuses included in this study were in the third trimester, and the distribution across GA is shown in Fig. 1. ROI placement is illustrated in Fig. 2. As shown in Fig. 3, changes in ADC were rather small over this relatively narrow gestational age range, and although a trend towards a decrease in ADC with increasing GA was observed in most regions, it was not statistically significant in any region. The only exception was the frontal lobe, which exhibited a trend towards an increase, rather than decrease, in ADC with increasing GA, but this trend also failed to reach statistical significance.
In view of this finding, mean ADC/region was calculated and subjected to statistical analysis by one-way ANOVA (Fig. 4). ADC values were highest in the white matter, with significantly (p < 0.05) lower values in basal ganglia and cerebellum and the lowest values in thalamus and pons.
Mean regional ADC in normal 3rd trimester fetuses. Bars represent means ± SEM of 40–48 cases/region. BG basal ganglia, Cb cerebellum, FWM frontal white matter, OccWM occipital white matter, ParWM parietal white matter, TempWM temporal white matter, Thal thalamus. *p < 0.05 relative to all white matter regions, ANOVA followed by Fisher’s PLSD post hoc analysis
Fetuses with confirmed CMV infection had significantly decreased ADC throughout the brain (Fig. 5), as revealed by two-way ANOVA. We found highly significant effects of diagnosis (F = 10, p < 0.003) and region (F = 19, p < 0.0001) but no significant interaction term. The decreases ranged from 20 % in the parietal white matter to 10 % in the cerebellum.
Finally, we have reanalyzed our data omitting the two normal cases that had siblings with white matter disease (cases #19 and 24, Table 1), since they may be at increased risk, but the MRI sequences used in our study are not diagnostic of white matter disease in fetuses. The removal of these cases (one with GA of 32 weeks and one with GA of 33 weeks, Table 1) had a negligible effect (less than 1 % change) on the mean ADC values across regions and GA and did not affect the statistical significance (or lack thereof) of the region and GA dependence of ADC or the comparison between normal and CMV-infected fetuses.
Discussion
The results of this study, utilizing the largest cohort of 3rd trimester fetuses relative to the published literature, demonstrate that brain ADC is regionally variable but relatively stable between gestational weeks 26 and 33. Regional variation was demonstrated by higher values in the white matter relative to the basal ganglia, cerebellum, thalamus, and pons. This regional profile is similar to the one reported in other studies of fetal, premature, and postnatal brains and follows the expected rank order based on the rate of maturation and myelination of these regions and also related to the cellularity of the region, as documented by other techniques such as US and T2- and T1-weighted sequences, diffusion tensor imaging (DTI) fMRI, and spectroscopy [10, 11]. Previous publications report decreases in ADC in the majority of brain regions [1] (with the exception of the frontal lobe) during fetal and postnatal brain development, while others [12] report significant GA-related decreases only in cerebellum, pons, and thalamus with no changes in other regions, over the age range of 19–37 weeks. Our results show a weak trend for regional ADC decline in all regions which does not reach statistical significance. This apparent disagreement most likely reflects the relatively narrow gestational age range in our study relative to some previous publications and is related to the fact that the white matter tracts are formed earlier, even before the 23rd week of gestation [13]. Thus, inspection of the data presented by Schneider et al. [2, 14] reveals that the apparent decrease in ADC with gestational age is driven by the subgroup of fetuses scanned during the 2nd trimester (21–25 weeks GA), which are not represented in our sample. This observation raises the interesting possibility that regional myelination and other processes which reduce ADC are not a linear function of GA, but rather occur in “waves” with some developmental periods showing higher rates of ADC change than others. This interpretation is supported by data from histology and other methods for evaluation of brain maturation and myelination [15–17]. Petra et al. [18] shared the ADC values of term infants; the highest value was found in the anterior white matter. They also found that decrease in the ADC value allows detection of changes in response to brain injury. It is well-established that reduction in ADC values of various brain areas occurs following different neuropathologies such as ischemia [19, 20] and malignancies [21, 22]. Our small subgroup of CMV-infected fetuses also presented with lowering of the ADC value, and the significance of this observation is still to be investigated.
In general, the absolute values of ADC we report are close to those reported by others for fetal brain, suggesting that ADC measurements are relatively platform-independent. The coefficient of variance within 3rd trimester fetal brain regions did not exceed 15 %, which is conducive to using these data as a normative data base. Viola et al. [23] compared the ADC value of premature infants with fetuses with mean age of 37 weeks GA. They found differences between the two groups, indicating that MR data from the premature brain are not appropriate for the assessment of the fetal brain maturation.
We also report the first evaluation of ADC in CMV-infected fetuses in utero. Our finding of reduced ADC most likely reflects microgliosis which is the hallmark of neuroinflammation of all causes [24]. Van der Voorn et al. [25] reported the ADC value and the fractional anisotropy (FA) in the infected pediatric brain. In their study, the ADC value was higher than the normal value, probably due to damage to the tissue.
The data presented here add to the previously published data on ADC values at various gestational ages, but represent the largest study of normal third trimester fetuses. Future research utilizing DWI in fetal neuroimaging should emphasize the early and accurate detection of perinatal brain abnormalities.
Limitations of the current study
The normal fetuses included in the current study were considered healthy at the time of scanning based on several criteria including normal course of pregnancy, healthy mother, and no overt findings on T1-, T2-, and diffusion-weighted MRI. While these inclusion criteria are similar to those used in the majority of studies on normal fetal development of ADC (e.g., [12, 23]), they do not exclude conditions for which these criteria are not diagnostic (e.g., fetal white matter disease, incipient autism spectrum disorder). Subtle motion artifacts and occult diseases cannot be excluded in this study, so the adoption of the values from the “normal” group as normative should be done with caution, and more studies need to be done with more extended postnatal follow-up to firm up a normative data base.
Conclusion
Brain ADC is regionally variable but relatively stable between gestational weeks 26 and 33. Regional variation is demonstrated by higher values in the white matter relative to the basal ganglia, cerebellum, thalamus, and pons. Establishing the normal values of ADC enables us to evaluate and investigate cases with suspected pathology in the future.
References
Righini A, Bianchini E, Parazzini C, Gementi P, Ramenghi L, Baldoli C, Nicolini U, Mosca F, Triulzi F (2003) Apparent diffusion coefficient determination in normal fetal brain: a prenatal MR imaging study. AJNR Am J Neuroradiol 24(5):799–804
Schneider JF, Confort-Gouny S, Le Fur Y, Viout P, Bennathan M, Chapon F, Fogliarini C, Cozzone P, Girard N (2007) Diffusion-weighted imaging in normal fetal brain maturation. Eur Radiol 17(9):2422–2429. doi:10.1007/s00330-007-0634-x
Cannie M, De Keyzer F, Meersschaert J, Jani J, Lewi L, Deprest J, Dymarkowski S, Demaerel P (2007) A diffusion-weighted template for gestational age-related apparent diffusion coefficient values in the developing fetal brain. Ultrasound Obstet Gynecol Off J Int Soc Ultrasound Obstet Gynecol 30(3):318–324. doi:10.1002/uog.4078
Manganaro L, Perrone A, Savelli S, Di Maurizio M, Maggi C, Ballesio L, Porfiri LM, De Felice C, Marinoni E, Marini M (2007) Evaluation of normal brain development by prenatal MR imaging. Radiol Med 112(3):444–455. doi:10.1007/s11547-007-0153-5
Huppi PS, Maier SE, Peled S, Zientara GP, Barnes PD, Jolesz FA, Volpe JJ (1998) Microstructural development of human newborn cerebral white matter assessed in vivo by diffusion tensor magnetic resonance imaging. Pediatr Res 44(4):584–590. doi:10.1203/00006450-199810000-00019
Neil JJ, Shiran SI, McKinstry RC, Schefft GL, Snyder AZ, Almli CR, Akbudak E, Aronovitz JA, Miller JP, Lee BC, Conturo TE (1998) Normal brain in human newborns: apparent diffusion coefficient and diffusion anisotropy measured by using diffusion tensor MR imaging. Radiology 209(1):57–66. doi:10.1148/radiology.209.1.9769812
Tanner SF, Ramenghi LA, Ridgway JP, Berry E, Saysell MA, Martinez D, Arthur RJ, Smith MA, Levene MI (2000) Quantitative comparison of intrabrain diffusion in adults and preterm and term neonates and infants. AJR Am J Roentgenol 174(6):1643–1649. doi:10.2214/ajr.174.6.1741643
Miller SP, Vigneron DB, Henry RG, Bohland MA, Ceppi-Cozzio C, Hoffman C, Newton N, Partridge JC, Ferriero DM, Barkovich AJ (2002) Serial quantitative diffusion tensor MRI of the premature brain: development in newborns with and without injury. J Magn Reson Imaging JMRI 16(6):621–632. doi:10.1002/jmri.10205
Hoffmann C, Grossman R, Bokov I, Lipitz S, Biegon A (2010) Effect of cytomegalovirus infection on temporal lobe development in utero: quantitative MRI studies. Eur Neuropsychopharmacol J Eur Coll Neuropsychopharmacol 20(12):848–854. doi:10.1016/j.euroneuro.2010.08.006
Mailath-Pokorny M, Kasprian G, Mitter C, Schopf V, Nemec U, Prayer D (2012) Magnetic resonance methods in fetal neurology. Semin Fetal Neonatal Med 17(5):278–284. doi:10.1016/j.siny.2012.06.002
Maas LC, Mukherjee P, Carballido-Gamio J, Veeraraghavan S, Miller SP, Partridge SC, Henry RG, Barkovich AJ, Vigneron DB (2004) Early laminar organization of the human cerebrum demonstrated with diffusion tensor imaging in extremely premature infants. NeuroImage 22(3):1134–1140. doi:10.1016/j.neuroimage.2004.02.035
Boyer AC, Goncalves LF, Lee W, Shetty A, Holman A, Yeo L, Romero R (2013) Magnetic resonance diffusion-weighted imaging: reproducibility of regional apparent diffusion coefficients for the normal fetal brain. Ultrasound Obstet Gynecol Off J Int Soc Ultrasound Obstet Gynecol 41(2):190–197. doi:10.1002/uog.11219
Vasung L, Huang H, Jovanov-Milosevic N, Pletikos M, Mori S, Kostovic I (2010) Development of axonal pathways in the human fetal fronto-limbic brain: histochemical characterization and diffusion tensor imaging. J Anat 217(4):400–417. doi:10.1111/j.1469-7580.2010.01260.x
Schneider MM, Berman JI, Baumer FM, Glass HC, Jeng S, Jeremy RJ, Esch M, Biran V, Barkovich AJ, Studholme C, Xu D, Glenn OA (2009) Normative apparent diffusion coefficient values in the developing fetal brain. AJNR Am J Neuroradiol 30(9):1799–1803. doi:10.3174/ajnr.A1661
Ramenghi LA, Martinelli A, De Carli A, Brusati V, Mandia L, Fumagalli M, Triulzi F, Mosca F, Cetin I (2011) Cerebral maturation in IUGR and appropriate for gestational age preterm babies. Reprod Sci 18(5):469–475. doi:10.1177/1933719110388847
Weidenheim KM, Epshteyn I, Rashbaum WK, Lyman WD (1993) Neuroanatomical localization of myelin basic protein in the late first and early second trimester human foetal spinal cord and brainstem. J Neurocytol 22(7):507–516
Weidenheim KM, Bodhireddy SR, Rashbaum WK, Lyman WD (1996) Temporal and spatial expression of major myelin proteins in the human fetal spinal cord during the second trimester. J Neuropathol Exp Neurol 55(6):734–745
Huppi PS, Dubois J (2006) Diffusion tensor imaging of brain development. Semin Fetal Neonatal Med 11(6):489–497. doi:10.1016/j.siny.2006.07.006
Marks MP, de Crespigny A, Lentz D, Enzmann DR, Albers GW, Moseley ME (1996) Acute and chronic stroke: navigated spin-echo diffusion-weighted MR imaging. Radiology 199(2):403–408. doi:10.1148/radiology.199.2.8668785
Desai V, Shen Q, Duong TQ (2012) Incorporating ADC temporal profiles to predict ischemic tissue fate in acute stroke. Brain Res 1458:86–92. doi:10.1016/j.brainres.2012.04.004
Kralik SF, Taha A, Kamer AP, Cardinal JS, Seltman TA, Ho CY (2013) Diffusion imaging for tumor grading of supratentorial brain tumors in the first year of life. AJNR Am J Neuroradiol. doi:10.3174/ajnr.A3757
Barajas RF Jr, Rubenstein JL, Chang JS, Hwang J, Cha S (2010) Diffusion-weighted MR imaging derived apparent diffusion coefficient is predictive of clinical outcome in primary central nervous system lymphoma. AJNR Am J Neuroradiol 31(1):60–66. doi:10.3174/ajnr.A1750
Viola A, Confort-Gouny S, Schneider JF, Le Fur Y, Viout P, Chapon F, Pineau S, Cozzone PJ, Girard N (2011) Is brain maturation comparable in fetuses and premature neonates at term equivalent age? AJNR Am J Neuroradiol 32(8):1451–1458. doi:10.3174/ajnr.A2555
Carson MJ, Thrash JC, Walter B (2006) The cellular response in neuroinflammation: the role of leukocytes, microglia and astrocytes in neuronal death and survival. Clin Neurosci Res 6(5):237–245. doi:10.1016/j.cnr.2006.09.004
van der Voorn JP, Pouwels PJ, Vermeulen RJ, Barkhof F, van der Knaap MS (2009) Quantitative MR imaging and spectroscopy in congenital cytomegalovirus infection and periventricular leukomalacia suggests a comparable neuropathological substrate of the cerebral white matter lesions. Neuropediatrics 40(4):168–173. doi:10.1055/s-0029-1243228
Ethical standards and patient consent
We declare that all human and animal studies have been approved by the Institutional Review Board and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. We declare that patient consent was waived in this study.
Conflict of interest
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Chen Hoffmann and Boaz Weisz contributed equally to the manuscript.
Rights and permissions
About this article
Cite this article
Hoffmann, C., Weisz, B., Lipitz, S. et al. Regional apparent diffusion coefficient values in 3rd trimester fetal brain. Neuroradiology 56, 561–567 (2014). https://doi.org/10.1007/s00234-014-1359-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-014-1359-6