Abstract
Introduction
Recently two classification methods based on the location and the extent of thrombosis detected with CT angiography have been introduced: the Boston Acute Stroke Imaging Scale (BASIS) and the clot burden score (CBS). We studied the performance of BASIS and CBS in predicting good clinical outcome (mRS ≤2 at 90 days) in an acute (<3 h) stroke cohort treated with intravenous thrombolytic therapy.
Methods
Eighty-three consecutive patients who underwent multimodal CT were analyzed. Binary logistic regression model was used to assess how BASIS, CBS, and cerebral blood volume (CBV) ASPECTS predict favorable clinical outcome. Diagnostic sensitivities and specificities were calculated and compared.
Results
Patients with low CBS and CBV ASPECTS scores and major strokes according to BASIS had significantly higher admission NIHSS scores, larger perfusion defects, and more often poor clinical outcome. In logistic regression analysis, CBV ASPECTS, CBS and BASIS were significantly associated with the clinical outcome. The performance of BASIS improved when patients with thrombosis of the M2 segment of the middle cerebral artery were classified as having minor stroke (M1-BASIS). In the anterior circulation, the sum of CBS and CBV ASPECTS (CBSV) proved to be the most robust predictor of favorable outcome. CBV ASPECTS and CBS had high sensitivity but moderate to poor specificity while BASIS was only moderately sensitive and specific.
Conclusion
CBS, BASIS, and CBV ASPECTS are statistically robust and sensitive but unspecific predictors of good clinical outcome. Two new derived imaging parameters, CBSV and M1-BASIS, share these properties and may have increased prognostic value.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Computed tomography angiography (CTA) of the intracranial vessels is increasingly being performed either separately or as part of multimodal CT evaluation of acute ischemic stroke to detect intravascular occlusion by clots, hemodynamically significant stenotic atherosclerotic lesions, arterial dissection, and other arteriopathies. CTA provides an independent prognostic factor with proximal, high-volume clots predicting poor clinical outcome when compared to distal, low-volume clots [1–9].
Recently two classification methods based on the location and the extent of the thrombus detected with CTA have been introduced. Boston Acute Stroke Imaging Scale (BASIS) is a binary classification scheme where patients are designated to have either major or minor stroke [5]. In short, if the distal internal carotid artery (ICA), the proximal (segments M1 and M2) middle cerebral artery (MCA), or the basilar artery is occluded or if there is a significant ischemic lesion either in noncontrast CT (NCCT) or diffusion-weighted MRI, the stroke is considered major, otherwise the stroke is considered minor [5]. BASIS is correlated to short-term clinical outcome evaluated at discharge from the hospital and the length and the costs of hospitalization [5, 6]. Clot burden score (CBS) is a more elaborate scheme in which a score from 0 to 10 is given based on the extent of arterial segments affected in the anterior circulation [7, 8]. The scoring system has been pictorially demonstrated by Puetz et al. [8]. CBS is correlated to the clinical and radiological outcomes [7–9].
We reviewed retrospectively the clinical and imaging data of 83 consecutive patients who underwent multimodal CT assessment and received intravenous thrombolytic therapy to treat acute (<3 h) ischemic stroke in order to study the performance of BASIS and CBS in predicting the clinical outcome. Further, we correlated the anatomical information conveyed by BASIS and CBS with CT perfusion (CTP) parameters that reflect the hemodynamic state in the cerebral vasculature and hypothesized that a derived parameter combining both CTA and CTP data might best predict the clinical outcome.
Materials and methods
Overview
We analyzed retrospectively the clinical and imaging data of 380 consecutive patients who were admitted to Tampere University hospital between January 2007 and December 2007 because of acute (duration <3 h) stroke-like symptoms. After clinical and imaging evaluation, 92 patients received intravenous recombinant tissue plasminogen activator (rtPA) to treat acute ischemic stroke. Among these patients full admission multimodal (NCCT, CTA, and CTP) imaging evaluation was successfully completed with 72 patients while an additional 11 patients were evaluated with just NCCT and CTA because of chronic renal failure, imminent closure of the 3 h time window, or movement artifacts that rendered some of the imaging data uninterpretable. These 83 patients were selected to this study. The selection of patients to receive thrombolytic therapy was based on institutional guidelines that did not have CTP or CTA-derived parameters as exclusion or inclusion criteria. Standard intravenous rtPA administration scheme was used: Actilyse (Boehringer-Ingelheim, Ingelheim, Germany), total dose 0.9 mg/kg from which 10% given as a bolus and the remaining 90% as a continuous infusion for 1 h. Stable access to an emergency angiography suite was not available at the time so intra-arterial interventions were not included in the treatment protocol. A follow-up NCCT was performed for all patients 24 h after the administration of the thrombolytic agent. National Institutes of Health Stroke Scale (NIHSS) was assessed at the admission and 24 h after the thrombolytic therapy. Modified Rankin scale (mRS) was evaluated preictally and on day 90. The clinical data were stored prospectively to the patient records during the hospital stay and on day 90 after the ictus, the latter following a phone interview. These data were collected from the patient records and critically reviewed for errors using the data available from all medical and related disciplines (JTS). The study was approved by Tampere University hospital ethics committee.
Imaging parameters
Computed tomography scans were obtained using two different multidetector scanners: General Electrics LightSpeed 16-slice (GE Healthcare, Milwaukee, WI) and Philips Brilliance 64-slice (Philips, Cleveland, OH). The imaging procedures and the parameters used are described thoroughly in our previous study available online as an open-access article at the website of the publisher [10].
Image analysis
NCCT examinations were reviewed using dedicated medical imaging workstations. CTA and CTP images were analyzed with Advantage Workstation version 3.2 (GE Healthcare). The examinations were reviewed in the order NCCT, CTA, and finally CTP paralleling that of the clinical work flow. The reviewers were blinded to the clinical data apart from the side and nature of the acute symptoms. The analysis of the NCCT and the CTP images is detailed in our previous article [10]. CTA images were studied by examining the raw data and maximum intensity projection images. The principles of the CBS scoring system and the assignment of BASIS have been described in recent studies [5, 7]. CBS was scored, and BASIS was assigned independently by two radiologists (NS and AL). In cases where the scoring or the assignment differed, a consensus opinion was agreed on. These results were correlated with the original neuroradiological report. If significant discrepancies were present, the neuroradiologist that had issued the report was further consulted. Intraclass correlation coefficient (ICC) between a staff radiologist (NS) and an experienced neuroradiologist (JH) for a test sample (n = 20) for CBS was 0.87. The interobserver agreement index for BASIS was 95%. The interobserver variability statistics for the other imaging parameters used are described in our previous article [10].
Statistics
The data was analyzed with SPSS version 18 (SPSS Inc., Chicago, IL). Group comparisons were performed by using the Mann–Whitney U test and the Fisher exact test. Patients with mRS ≤2 at 90 days were considered to have experienced good clinical outcome. After excluding cases with thrombosis of the basilar artery, receiver operating characteristic curves (ROC) were computed for the imaging parameters studied using dichotomized clinical outcome as the state variable. Youden index was evaluated to select for optimal threshold value. A binary logistic regression model using the clinical outcome as the dependent variable was repeated for different variables of interest. Age and gender were treated as potential confounders and were controlled for by treating them as covariates. One variable of interest was included in the model at a time. The calibration of the models was evaluated with the Hosmer–Lemeshow test and the discrimination with the C statistic. Odds ratio (OR) with 95% confidence interval (CI) was calculated for each covariate. Sensitivity, specificity, and confidence interval calculations were performed using standard procedures. The McNemar test was used to compare the sensitivities and specificities calculated. The Bonferroni correction was applied to adjust for multiple comparisons.
Results
Baseline characteristics
The median age of the patients was 71 years (interquartile range 62–80 years, 40 female). Based on the clinical features and the imaging studies, in 11 of the 83 patients evaluated (13%), the ischemic episode involved the posterior circulation. The rest of the episodes were considered to involve the anterior circulation. Thrombosis could be demonstrated with CTA in 37 cases (45%). The locations of the thrombi are described in Table 1. In 40 cases (56%) of the 72 evaluated with CTP, a perfusion defect could be detected in the Alberta Stroke Program Early CT Score (ASPECTS) planes. An additional six perfusion defects were found outside the ASPECTS planes. In total, a perfusion defect could be demonstrated in 64% of the CTP studies (50% of all patients). The median NIHSS score at the admission was 7 (interquartile range 4–12, 54% had NIHSS <8, 18% had NIHSS >15), and 24 h later, the score was 2. The median time from symptom onset to treatment was 138 min (interquartile range 114–162). The median mRS was 1 preictally and 2 90 days later. The median change in mRS (∆mRS) was 1 point. Seventy-four percent of the patients experienced favorable clinical outcome at 90 days (mRS ≤2). At 24 h a local hemorrhagic complication (HI1, HI2, PH1, or PH2) was detected in five cases (6.0%) and four patients (4.8%) had parenchymal hemorrhage distant to the site of the infarct (PHr1 or PHr2). The validation of the ASPECTS scoring method for CTP is depicted in our previous study [10].
CBS, BASIS, and CBV ASPECTS as prognostic classifiers
CBS and cerebral blood volume (CBV) ASPECTS were dichotomized using the thresholds (CBS >6 and CBV ASPECTS >6) that best differentiated good from poor clinical outcome in the previous studies [7, 10–14]. BASIS is by definition a dichotomous variable that classifies strokes as either major or minor. Table 2 summarizes the comparison of patients in the subgroups so formed for all intracranial vascular territories (n = 83), whereas in Table 3, only patients suffering from anterior circulation stroke were included in the analysis (n = 72). There was no significant difference in age between the patients in the different subgroups. There were more female patients with major strokes and more male patients with minor strokes according to the BASIS classification (p = 0.01). As expected, patients with low CBS and CBV ASPECTS scores and patients with major strokes had significantly higher admission NIHSS scores, significantly larger perfusion defects in the CBV and mean transit time (MTT) maps and more findings related to acute ischemic process in the admission NCCT. Patients in the low CBS and low CBV ASPECTS subgroups invariably had major stroke according to BASIS. Patients with low CBV ASPECTS and major stroke had more proximal and higher volume thrombi shown by significantly lower CBS. Low CBS and CBV ASPECTS and major stroke significantly predicted poor clinical outcome and larger infarct volume 24 h after the administration of thrombolytic therapy. The ability of CBS and CBV ASPECTS to predict the clinical outcome was enhanced when only anterior circulation strokes were included in the analysis, whereas the predictive power of BASIS improved when all vascular territories were included in the analysis. BASIS did not reach statistical significance when only patients with anterior circulation strokes were analyzed (p = 0.23). This is because patients with thrombosis in the M2 segment of the MCA are classified as having major stroke, and yet in the study population, 83% of these patients had good clinical outcome. If these patients were classified as having minor stroke, BASIS performed considerably better (Table 4). This modification is referred to as M1-BASIS in Tables 4, 5, and 6 and in the following paragraphs.
There were eight cases of local and/or peripheral hemorrhagic complications in the study population. In four patients the hemorrhages were mild and did not produce any symptoms. In the other four patients, a notable space-occupying effect was present. When cross-tabulated with the dichotomized imaging parameters, none of the parameters predicted hemorrhagic transformation statistically significantly.
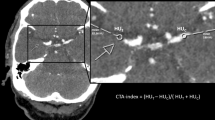
In order to further assess the prognostic value of these dichotomous imaging parameters, we performed binary logistic regression analysis using the mRS at 90 days dichotomized with the threshold ≤2 as the dependent variable (Table 5). We also devised a novel parameter which combines CBS and CBV ASPECTS by calculating an unweighted sum of the scores for each patient. This parameter was named CBSV. Using ROC analysis with clinical outcome as the state variable, an optimal threshold for dichotomization was calculated for CBSV (>15, area under the curve (AUC) = 0.72, Fig. 1) and this dichotomized variable was entered into the regression analysis. Figure 1 also shows ROC curves for CBS (AUC = 0.69) and CBV ASPECTS (AUC = 0.70). Age and gender were treated as potential confounders and were controlled for by treating them as covariates. When all vascular territories were included in the analysis, CBV ASPECTS, CBS, CBSV, BASIS, and M1-BASIS were all significantly associated with the clinical outcome. CBV ASPECTS displayed the largest odds ratio for good clinical outcome (p = 0.005, OR = 13.3). NCCT ASPECTS and gender were not significantly associated with the clinical outcome, whereas a low NIHSS score at presentation significantly predicted good clinical outcome (p = 0.007). Age had a modest effect with old age being a risk factor for poor outcome (p = 0.02). When only anterior circulation strokes were considered, CBV ASPECTS, CBS, CBSV, and M1-BASIS were significantly associated with the clinical outcome with CBSV having the best statistical confidence level (p = 0.002, OR = 16.3). CBS displayed the largest odds ratio (p = 0.005, OR = 25.1). BASIS did not reach statistical significance.
Sensitivities and specificities for detecting good clinical outcome were calculated for all the imaging parameters that achieved statistical significance in the regression analysis (Table 6). When all vascular territories were included in the analysis, CBV ASPECTS was the most sensitive predictor of good clinical outcome (0.96, CI 95% = 0.86–0.99) while BASIS had the best specificity (0.57, CI 95% = 0.34–0.77). In the case of sensitivity, the differences between CBV ASPECTS, CBS, and CBSV were not statistically significant while BASIS was significantly less sensitive than any of the other parameters. M1-BASIS was less sensitive than CBV ASPECTS (p = 0.03). In the case of specificity, BASIS and M1-BASIS were significantly more specific when compared to CBS (p = 0.02 and p = 0.04, respectively). Otherwise there were no statistically significant differences. When only the anterior circulation was considered, CBV ASPECTS was the most sensitive (0.96, CI 95% = 0.86–0.99) and CBSV the most specific (0.47, CI 95% = 0.22–0.73) predictor. BASIS proved to be significantly less sensitive when compared to all the other parameters (p = 0.001–0.008). There were no statistically significant differences between specificities. When the Bonferroni correction was applied to adjust for multiple comparisons, BASIS remained to be significantly less sensitive than other parameters both in the case of all vascular territories and the anterior circulation while all other differences were rendered statistically nonsignificant.
Discussion
Recently a number of imaging parameters have been introduced that may be useful in the risk stratification and the treatment decision making in acute ischemic stroke. We studied the performance of two CTA-based classification schemes, BASIS and CBS, and one perfusion parameter, CBV ASPECTS, in a thrombolytic therapy cohort.
In the absence of adequate collateral circulation, vessel recanalization is a necessary condition to favorable clinical outcome. The location, the volume, and the composition of the clot essentially determine the effectiveness of intravenous rtPA in dissolving the occluding thrombus [1–9, 15]. The time from the onset of the symptoms to the possible recanalization largely determines the functional outcome as the duration of parenchymal ischemia dictates the progression of the irreversible changes, i.e., the size of the infarct core [16]. Both BASIS and CBS address the location of the clot, while CBS also takes into account the volume. CBV ASPECTS estimates the size of the infarct core.
Patients with low CBS and CBV ASPECTS scores and with major strokes according to BASIS had significantly higher admission NIHSS scores, larger perfusion defects, larger infarct volumes, more findings related to acute ischemic process in the admission NCCT, and more often poor clinical outcome. CBS and CBV ASPECTS predicted the clinical outcome more accurately when only anterior circulation strokes were analyzed which is to be expected as these scoring schemes do not include data from the posterior circulation. BASIS, on the other hand, also takes into account the posterior circulation. Thus it performs better when all vascular territories are included in the analysis as patients with occlusion of the basilar artery are correctly classified as having major stroke. However, BASIS did not reach statistical significance when only patients with anterior circulation stroke were analyzed. This is remedied if patients with thrombosis of the M2 segment are classified as having minor stroke (p = 0.23 vs. p = 0.002). This modified BASIS, which we named M1-BASIS, seems to perform slightly better than BASIS also when all vascular territories are included in the analysis. These findings probably reflect the effect of the thrombolytic therapy and support the notion that patients with thrombosis of the M2 segment of the MCA benefit from intravenous thrombolytic therapy, whereas a more proximal clot location predicts limited response [1, 3, 9, 17]. Only a minority of the patients (8%) received thrombolytic therapy in the study population that was originally used to validate BASIS [5].
In the logistic regression analysis, dichotomized M1-BASIS, CBV ASPECTS, CBS, and BASIS were all significantly associated with the clinical outcome (p = 0.001, p = 0.005, p = 0.02, and p = 0.01, respectively). When only anterior circulation strokes were considered, the sum of CBS and CBV ASPECTS, a novel variable which we named CBSV, proved to be the most robust predictor of favorable outcome (p = 0.002, OR = 16.3). CBSV combines two independent predictors of clinical outcome that reflect different pathophysiological processes: CBV ASPECTS that approximates the volume of already irreversibly damaged brain tissue and CBS that provides information about clot extent and location [7, 8, 10]. Thus, theoretically CBSV should have better predictive power than either of its components. This is supported by our results.
CBV ASPECTS, CBS, CBSV, and M1-BASIS all had high sensitivity (85–96%) but moderate to poor specificity (24–52%) in predicting good clinical outcome. The rather modest specificity is to be expected as not all patients with potentially favorable profile experience recanalization and as strategic infarcts may cause serious functional deficit with minimal imaging findings. Further, there were four patients (two with anterior circulation strokes) with prestroke mRS >2 that were classified as low-risk patients by CBS, CBV ASPECTS, and CBSV, which decreases the specificity of these parameters somewhat. BASIS was only moderately sensitive (70–71%). There were no statistically significant differences between specificities after the Bonferroni correction was applied to adjust for multiple comparisons. Tan et al. found CBS to be less sensitive but more specific when compared to our findings [7]. This is probably due to considerably higher median NIHSS score (16) and lower proportion of patients treated with rtPA (70.5%) in their study population.
Our study is limited by the retrospective design and sample size. There was some heterogeneity in the details of treatment and variation in onset-to-needle times which are to be expected in a clinically managed population. Because of the study design, data on vessel recanalization were not available for the majority of the patients. However, a large final infarct volume is intimately related to delayed or failed recanalization and can be used as a surrogate. M1-BASIS was created based on a post hoc analysis of the data set and should be further validated in other thrombolytic therapy cohorts.
In conclusion, novel imaging parameters that lie upstream to clinical parameters (NIHSS) in the pathophysiological chain of ischemic stroke potentially allow higher resolution in the risk stratification and the treatment decision making. Optimally a selection of markers portraying different aspects of the disease state and having independent prognostic value would be utilized. These markers include anatomical angiographic data revealing the location and the extent of the clot (CBS and BASIS) and dynamic perfusion data enabling the detection of irreversibly damaged and potentially salvageable brain tissue (CBV ASPECTS and CTP ASPECTS mismatch) [10]. We demonstrated that CBS, BASIS, and CBV ASPECTS are statistically robust and sensitive but unspecific predictors of good clinical outcome among patients receiving intravenous thrombolytic therapy. We introduced two derived imaging parameters, CBSV and M1-BASIS, that essentially share these same properties but seem to have slightly better prognostic accuracy. BASIS was significantly less sensitive than the other parameters studied.
Abbreviations
- ASPECTS:
-
Alberta Stroke Program Early CT Score
- AUC:
-
Area under the curve
- BASIS:
-
Boston Acute Stroke Imaging Scale
- CBV:
-
Cerebral blood volume
- C :
-
C statistic
- CBS:
-
Clot burden score
- CI:
-
Confidence interval
- CTA:
-
Computed tomography angiography
- CTP:
-
Computed tomography perfusion
- H-L:
-
Hosmer–Lemeshow
- MTT:
-
Mean transit time
- MCA:
-
Middle cerebral artery
- NCCT:
-
Noncontrast-enhanced computed tomography
- NIHSS:
-
National Institutes of Health Stroke Scale
- mRS:
-
Modified Rankin scale
- ROC:
-
Receiver operating characteristic
- rtPA:
-
Recombinant tissue plasminogen activator
References
Somford DM, Nederkoorn PJ, Rutgers DR, Kappelle LJ, Mali WP, van der Grond J (2002) Proximal and distal hyperattenuating middle cerebral artery signs at CT: different prognostic implications. Radiology 223:667–671
Gralla J, Burkhardt M, Schroth G, El-Koussy M, Reinert M, Nedeltchev K, Slotboom J, Brekenfeld C (2008) Occlusion length is a crucial determinant of efficiency and complication rate in thrombectomy for acute ischemic stroke. AJNR Am J Neuroradiol 29:247–252
Linfante I, Llinas RH, Selim M, Chaves C, Kumar S, Parker RA, Caplan LR, Schlaug G (2002) Clinical and vascular outcome in internal carotid artery versus middle cerebral artery occlusions after intravenous tissue plasminogen activator. Stroke 33:2066–2071
Smith WS, Tsao JW, Billings ME, Johnston SC, Hemphill JC 3rd, Bonovich DC, Dillon WP (2006) Prognostic significance of angiographically confirmed large vessel intracranial occlusion in patients presenting with acute brain ischemia. Neurocrit Care 4:14–17
Torres-Mozqueda F, He J, Yeh IB, Schwamm LH, Lev MH, Schaefer PW, González RG (2008) An acute ischemic stroke classification instrument that includes CT or MR angiography: the Boston Acute Stroke Imaging Scale. AJNR Am J Neuroradiol 29:1111–1117
Cipriano LE, Steinberg ML, Gazelle GS, González RG (2009) Comparing and predicting the costs and outcomes of patients with major and minor stroke using the Boston Acute Stroke Imaging Scale neuroimaging classification system. AJNR Am J Neuroradiol 30:703–709
Tan IY, Demchuk AM, Hopyan J, Zhang L, Gladstone D, Wong K, Martin M, Symons SP, Fox AJ, Aviv RI (2009) CT angiography clot burden score and collateral score: correlation with clinical and radiologic outcomes in acute middle cerebral artery infarct. AJNR Am J Neuroradiol 30:525–531
Puetz V, Dzialowski I, Hill MD, Subramaniam S, Sylaja PN, Krol A, O’Reilly C, Hudon ME, Hu WY, Coutts SB, Barber PA, Watson T, Roy J, Demchuk AM, Calgary CTA Study Group (2008) Intracranial thrombus extent predicts clinical outcome, final infarct size and hemorrhagic transformation in ischemic stroke: the clot burden score. Int J Stroke 3:230–236
Puetz V, Dzialowski I, Hill MD, Steffenhagen N, Coutts SB, O'Reilly C, Demchuk AM (2010) Malignant profile detected by CT angiographic information predicts poor prognosis despite thrombolysis within three hours from symptom onset. Cerebrovasc Dis 29:584–591
Sillanpaa N, Saarinen JT, Rusanen H, Hakomaki J, Lahteela A, Numminen H, Elovaara I, Dastidar P, Soimakallio S (2011) CT perfusion ASPECTS in the evaluation of acute ischemic stroke: thrombolytic therapy perspective. Cerebrovasc Dis Extra 1:6–16
Parsons MW, Pepper EM, Chan V, Siddique S, Rajaratnam S, Bateman GA, Levi CR (2005) Perfusion computed tomography: prediction of final infarct extent and stroke outcome. Ann Neurol 58:672–679
Aviv RI, Mandelcorn J, Chakraborty S, Gladstone D, Malham S, Tomlinson G, Fox AJ, Symons S (2007) Alberta stroke program early CT scoring of CT perfusion in early stroke visualization and assessment. AJNR Am J Neuroradiol 28:1975–1980
Kloska SP, Dittrich R, Fischer T, Nabavi DG, Fischbach R, Seidensticker P, Osada N, Ringelstein EB, Heindel W (2007) Perfusion CT in acute stroke: prediction of vessel recanalization and clinical outcome in intravenous thrombolytic therapy. Eur Radiol 17:2491–2498
Lin K, Rapalino O, Law M, Babb JS, Siller KA, Pramanik BK (2008) Accuracy of the Alberta stroke program early CT Score during the first 3 hours of middle cerebral artery stroke: comparison of noncontrast CT, CT angiography source images, and CT perfusion. AJNR Am J Neuroradiol 29:931–936
Liebeskind DS, Sanossian N, Yong WH, Starkman S, Tsang MP, Moya AL, Zheng DD, Abolian AM, Kim D, Ali LK, Shah SH, Towfighi A, Ovbiagele B, Kidwell CS, Tateshima S, Jahan R, Duckwiler GR, Viñuela F, Salamon N, Villablanca JP, Vinters HV, Marder VJ, Saver JL (2011) CT and MRI early vessel signs reflect clot composition in acute stroke. Stroke 42:1237–1243
Yoo AJ, Verduzco LA, Schaefer PW, Hirsch JA, Rabinov JD, González RG, MRI-Based Selection for Intra-Arterial Stroke Therapy (2009) Value of pretreatment diffusion-weighted imaging lesion volume in selecting patients with acute stroke who will benefit from early recanalization. Stroke 40:2046–2054
Kim YS, Garami Z, Mikulik R, Molina CA, Alexandrov AV, Collaborators CLOTBUST (2005) Early recanalization rates and clinical outcomes in patients with tandem internal carotid artery/middle cerebral artery occlusion and isolated middle cerebral artery occlusion. Stroke 36:869–871
Acknowledgement
This work was supported by the Pirkanmaa Hospital District General Medical Research Fund.
Conflict of interest
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sillanpaa, N., Saarinen, J.T., Rusanen, H. et al. The clot burden score, the Boston Acute Stroke Imaging Scale, the cerebral blood volume ASPECTS, and two novel imaging parameters in the prediction of clinical outcome of ischemic stroke patients receiving intravenous thrombolytic therapy. Neuroradiology 54, 663–672 (2012). https://doi.org/10.1007/s00234-011-0954-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-011-0954-z