Abstract
Introduction
Hypoplastic cochleae are among the inner ear malformations more frequently encountered by radiologists; little detailed information is available on these, however. We present the first large series of hypoplastic cochleae and document imaging findings to better characterize this anomaly radiologically.
Methods
We used our electronic database to search for inner ear malformations described between 1995 and 2009 and extracted 81 ears (of 47 patients) with hypoplastic cochleae out of 289 patients with inner ear malformations. Two neuroradiologists evaluated the available CT and MRI data. Measurements of all inner ear structures were performed. Accompanying findings were listed.
Results
Cochlear hypoplasia (58 ears, 32 patients) often involves not only the apical turn being reduced in size but also the basal turn being smaller in length. Additionally, 11 ears (eight patients) of hypoplastic cochleae with only a basal turn and five ears (four patients) of cochleae with only a small bud were identified. Non-classifiable hypoplastic cochleae (seven ears, five patients) were those with either a rudimentary or an absent basal turn or a “dwarf appearance” with no further partition.
Conclusions
The term “hypoplastic cochlea” is very general; a further division into severe and less severe forms based on the length and existence of cochlea turns is possible and can help enhance the comparison of CI outcome data. Measurements can help the less experienced radiologist to detect them more easily.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A wide variety of cochlear malformations exists. The anomalies of the cochlea that can be visualized by computed tomography (CT) are related to its size, the lumen, the modiolus and the bony partitions between the coils: the range of histologically visible anomalies is even wider. The size of the cochlea varies from normal to complete absence. This present study included cochleae of less than normal size; conditions known as cochlear hypoplasia. Even today, little information is available on these cochleae of significantly reduced size. Although there are frequent references to them as hypoplastic cochleae, studies even exist that do not mention this entity at all, as do otherwise very exhaustive textbooks that omit this malformation altogether. For a time, nearly every inner ear malformation involving the cochlea, including malformations where the cochlea was below normal size, was designated a Mondini or Mondini-type malformation [1]. A clarification of terms concerning the true Mondini malformation and the incomplete partition type I was published several years ago by Sennaroglou [2]. Our study does not include these Mondini malformations, which have now been clarified as describing a very special type of inner ear malformation with three characteristic features—a cystic apex, a dilated vestibule and a large vestibular aqueduct (VA) [3]—although (because of its cystic apex) the definition of a cochlea with less than two and a half turns did exist. Under Sennaroglou’s [2] classification it is now designated an incomplete partition type II, whereas the incomplete partition type I describes an empty, cystic cochlea and vestibule without an enlarged VA. Both malformations usually have a characteristic appearance without the cochlea being of reduced height or length.
Hypoplastic cochleae of reduced height generally have cochlear ducts that are (to differing extents) shortened: some may exhibit only slightly less than the normal two and a half turns, whereas others have a small bud—an excrescence of the vestibulum where the cochlear duct begins to grow. Since they may vary greatly in appearance, we subdivided these short or hypoplastic cochleae into three groups based on the existence of anything more than a basal turn, only a basal turn or a small bud that does not even attain a sufficient length to form a cochlear aperture. These differentiations have been made possible by a CT technique that has seen remarkable advances since Jackler [4] defined his theory of developmental arrest in 1987, chiefly on the basis of polytomography scans. In his drawings of inner ear malformations, however, Jackler had already depicted a severe and a mild form of cochlear hypoplasia; these involve, respectively, one with only a small bud in place of the cochlea, and a cochlea whose duct is of less than normal length. According to Jackler’s theory, developmental arrest takes place in the sixth week of gestation—in the former case, an early sixth-week arrest would be involved, and in the latter a late sixth-week arrest. Given the growing number of cochlear implantations (CIs), it would appear beneficial to describe malformations in as much detail as possible, so as to better compare outcome data from cochlear implant users.
Materials and methods
Patients
We used our electronic database to collect 289 patients with inner ear malformations between 1995 and September 2009 and extracted all patients with hypoplastic cochleae by visual inspection (47 patients). The patients were all referred by our Department of Otolaryngology for evaluation of their sensorineural hearing loss and possible cochlear implantation. Thirty-one of the 47 selected patients underwent additional magnetic resonance imaging (MRI) of the head and temporal bone.
Imaging
All 47 patients were evaluated using high-resolution spiral computed tomography (sCT) of the temporal bone. Different CT scanners were used over the very lengthy period covered by our literature review:
-
Eleven patients were examined using a HiSpeed Advantage RP CT scanner (GE, Milwaukee, WI, USA): helical CT examinations were performed at 140 kV and 80 mAs, with a section thickness of 1 mm and a pitch of 1.
-
Nine patients were examined using a HiSpeed Advantage CT scanner (GE, Milwaukee, WI, USA): helical CT examinations were performed at 120 kV and 80 mAs, with a section thickness of 1 mm and a pitch of 1. The field of view was 16 cm using a 512 × 512 matrix.
-
Twenty-seven patients were examined using a LightSpeed16 CT scanner (GE, Milwaukee, WI, USA): helical CT examinations were performed at 120 kV, auto mAs with a maximum up to 100 mAs, a speed of 5.62 s, a thickness of 0.625 mm, and a pitch of 0.562:1.
The acquired images were uploaded to our current picture archiving and communications system (PACS), except for 10 patients in which only the plain films were available. These were scanned in order to perform the measurements at the workstation.
-
Thirty-one patients underwent MRI of the head and temporal bone using two 1.5-T MR-Systems (Signa Horizon and NVI, GE, Milwaukee, WI, USA): axial T2-weighted FLAIR (TR 9000; TE 172; TI 2200; FOV 24 × 24; section thickness 6 mm; spacing 1.5 mm; matrix 256 × 192), sagittal T2-weighted fast-spin echo (TR 6060; TE 95; FOV 24 × 24; section thickness 3 mm; spacing 0.3 mm; matrix 512 × 256), axial T1-weighted spin echo (TR 500; TE 14; FOV 24 × 18; section thickness 3 mm; spacing 0.3 mm; matrix 320 × 256) and a T2-weighted three-dimensional gradient echo sequence (TR 11; TE 5; FOV 16 × 16; section thickness 0.8 mm; flip angle 65°; matrix 512 × 512) of the cerebellopontine angle region. Reconstructions perpendicular to the internal auditory canal (IAC) were obtained.
Study design
The cochleae were divided by visual inspection into the following groups:
-
Cochlear bud (“XXS cochlea”): severe hypoplasia of the cochlea. A small canal or bud can be detected running from the vestibulum in the direction of the basal turn, representing an excrescence of the vestibulum that did not attain sufficient length to form a cochlear aperture. The latter was, therefore, not present in this type of cochlear malformation.
-
Basal turn cochlea (“XS cochlea”): The basal turn can be identified, but the middle and apical turns cannot. In this group, the basal turn may have the normal width of a basal turn or may be dilated. (Unlike in the common cavity described by Edward Cock, however, there is no widely patent cochleovestibular duct.)
-
Hypoplastic cochlea (“S cochlea”): the basal turn is of normal length and parts of the apical turns are identifiable (although markedly reduced in size), but the overall height of the cochlea is already visually diminished.
-
Hypoplastic cochleae that do not fit one of the former criteria.
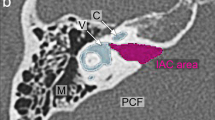
The CT and MRI data for of all these 47 patients were retrospectively evaluated by two neuroradiologists. Each ear was counted separately, giving a total of 81 ears, after subtracting 13 contralateral ears with other inner ear malformations or a normal appearance. The inner ear findings were categorized, and measurements of the following inner ear structures were performed in accordance with the procedure of Purcell et al. (2003) [5]. Measurements conducted using axial slices were the height and width of the basal and apical turns of the cochlea (Fig. 1), size of the bony island of the lateral SCC and width of the anterior and posterior SCC, height and width of the vestibulum and length of the IAC. The antero-posterior diameter (or width) of the IAC was measured in the mid-portion as per the procedure described by Krombach et al. (2005) [6]. In 72 ears (38 patients), coronal slices or reconstructions were also available and measurement of the cochlear height was performed in accordance with Purcell’s techniques.
The description of the vestibule and the lateral SCC included a special case: a cavity that incorporated the area of the vestibule and the lateral SCC, in the event that a bony island in the inner part of the lateral canal has not developed. Romo [7] termed this condition “common cavity of the vestibulum and the lateral SCC,” demonstrating a more severe dysplasia of the SCCs. In addition to the finding of an SCC with a blind ending, it was also found that the lateral branch of the anterior SCC fused with the posterior branch of the posterior SCC, while the other branches were absent, described in the table simply as fused. This condition is very similar to the absence of the common cruz, described by Schuhknecht et al. [8], although Schuhknecht published a drawing in which the two SCCs showed a retraction at the junction, which is not observed in most of our patients.
The VA was either described as visible (in patients where size was normal) or as enlarged. In patients where a VA could not be identified, this was termed “unable to identify” (UTI). The designation UTI was also used to describe the situation where it was not possible to clearly identify the number of nerves in the IAC, either because the canal was too small, for example, or for technical reasons such as artefacts.
In patients where MRI is available, the nervous structures in the IAC are evaluated. Adopting the method described by Casselman [9], axial and parasagittal slices of 1 mm thickness were obtained and the nervous structures counted. Other accompanying intracranial pathologies were also listed.
Statistics
All statistical evaluation was done using Microsoft Excel 2007. The measurements were compared with our normal data for inner ear structures. Our normal data was acquired from 50 normal controls, with an exclusion of patients with profound sensory neural hearing loss. The mean value, standard deviation (SD) and the range (minimum and maximum) were calculated from each subgroup.
Results
A hypoplastic cochlea is defined as a cochlea which is smaller than normal. This general definition held true for 81 of the ears included in our data collection.
Subclassification based on the presence of more or less than a basal turn and the existence of only a cochlear bud led to the following groups being formed: a hypoplastic cochlea with more than a basal turn but less than two and a half turns (58 ears) (Fig. 2); a basal turn cochlea (11 ears) (Fig. 3); and a cochlear bud only (five ears) (Fig. 4). The remaining seven ears did not match the former criteria (Fig. 5).
Cochlear hypoplasia (Fig. 2) was found in 58 ears and the mean age of diagnosis with CT was 19 years. Twenty-six patients (81%) exhibited this malformation bilaterally; in six patients it was found unilaterally. Six of the patients with bilateral hypoplasia were family cases (with two families involved: a mother and son, and a father with his two sons and one daughter). Accompanying SCC malformations were found in 48 ears (83%), details see Table 1. Included in these SCC malformations were 14 ears with a complete SCC aplasia (24%). The VA was visible in 45 ears (78%) and enlarged in eight ears (14%). Of these enlarged cases, MRI was available for five ears, revealing a large endolymphatic sac in all of these patients. Additionally, MRI data (available for 33 ears) indicated that the majority of ears (67%) presented four nerves of normal appearance in the IAC. Measurements confirmed what was to be expected: the mean cochlear height in the coronal view was, at 3.45 mm, less than minus two standard deviations (−2 SD) from normal (4.14 mm), and the apical turn height (mean 3.07 mm) and width (mean 2.14 mm) on axial slices were also less than −2 SD from normal (height 3.49 mm; width 2.67 mm). Measurements also revealed the length of the basal turn to be reduced (mean 8.13 mm, range 6.8 to 9.25 mm) while the normals −2 SD are 8.77 mm.
The 11 ears with a cochlea that consists of a basal turn or less, as diagnosed by CT, belonged to patients with a mean age of 4.9 years. Three patients had a bilateral basal turn cochlea, whereas the other five patients presented it unilateral. Measurements showed that the length of the basal turn was markedly reduced (mean 7.64 mm), with the apical turns absent.
A cochlear bud was found in five ears of four patients with the mean age of diagnosis being 4.7 years. The VA was visible in one ear. The mean length of the cochlear basal turn (i.e. identical to the bud) is 4.43 mm.
The description of the inner ear structures, including the number of nerves detected by MRI, are listed in Table 1. The statistical values of mean, SD and range of the measurement data, broken down by the type of malformation, are listed in Table 2.
Discussion
Measurements
The difficulty in recognizing a hypoplastic cochlea is that, rather than a distinct boundary existing between a normal and a hypoplastic cochlea, there is a smooth transition between pathology and normality. A collection of 58 hypoplastic cochleae and measurement data should help and enable the untrained eye to identify an abnormality of this nature. Purcell [5] already found it easier to identify two patients with cochlear hypoplasia after establishing normative cochlear and vestibular measurements in 15 normal patients. However, our range of normals revealed a somewhat larger range and was shifted a little further to values smaller than those published by Purcell.
Shim [10] also used measurement of the cochlea to define a cochlear hypoplasia; in contrast to our study, however, his patients with cochlear hypoplasia were not included by visual inspection, but found by application of the measurement data to 570 profound SNHL ears, which resulted in the identification (apart from other malformations) of 22 ears with cochlear hypoplasia. He defined cochlear hypoplasia as less than 2 SD from the mean values of his normal controls, something that is true for all of our hypoplastic cochleae as well.
A new aspect for which we did not find comparable data is the mean reduced basal turn length of hypoplastic cochlea. This was not seen by visual inspection alone; on the basis of our data, however, a normal basal turn length can be found in only 19% of patients with cochlear hypoplasia.
Jackler also used measurements to differentiate between the different kinds of cochlear malformation. His data were, however, taken from polytomography scans and are therefore not directly comparable, polytomography being subject to a 30% magnification factor.
Embryology
The hypoplastic cochlea in its severe and mild forms is described by Jackler [4]. He and many other authors place the time of a developmental arrest in such cases in the sixth gestational week. A developmental arrest resulting in a severe form will take place in the early sixth week and the mild form will occur as a late sixth-week arrest. Comparison of different descriptions of cochlear embryologic development reveals that different time points are indicated for the crucial period. Romo [7] describes the cochlear pouch as existing at three and a half to 4 weeks of gestation, at an embryo length of 7–8 mm. He states that the two and a half turns are fully developed at 10 weeks’ gestation (this actually being the longest period described) and a length of 30 mm. Streeter [11], however, who uses the developmental stages of many organs to classify embryos into different estimated ovulation ages, describes in great detail the short period in which the cochlear duct develops. He uses its advances to determine the age of an embryo in this critical period.
According to his description, it takes only approximately 10 days for the cochlea to develop from a cochlear bud into the full-length structure; with the cochlear pouch as the starting point, this period would be 16 days. The corresponding size of the embryos ranges from 7 to 12 mm up to 28–30 mm, which is in line with Som’s figures, although Streeter and Som differ in the length of time they indicate (Fig. 6).
Timeline of cochlear development according to different authors: Jackler, Som, and Streeter. Streeter used an estimated ovulation age, while Jackler and Som refer to the gestational age. Som and Streeter both additionally give the crown-rump length of the embryo (but citing different gestation periods/ovulation dates). The ovulation age is the gestation age plus 14 days
Hypoplastic cochlea
The hypoplastic cochlea is often listed as one of the more commonly occurring inner ear malformations with a reported percentage between 7% (Sennaroglou [2]), 16% (Papsin [12]), 17% (Shim [10]) and up to 36% (Park [13]). It is noticeable that other studies do not include (or did not find?) a cochlear hypoplasia at all [14]. However, while the cochlear aplasia is described in detail in current textbooks [15, 16], little information can be found on cochlear hypoplasia. It is usually included in descriptions that are broader in scope. In 1993, Schuhknecht [8] described the Mondini dysplasia as a dysplasia of the bony and membranous labyrinth, exhibiting a wide range of morphological and functional abnormality, that definitely included the malformation of a hypoplastic cochlea but also the incomplete partition type I and II. Our study included all cochlear malformations that present with a cochlea of reduced height. This was detected visually in all our patients and confirmed by measurement. Descriptions and definitions of cochlear hypoplasia are given by a number of authors, some describing cochleae similar to our “normal cochlear hypoplasia” (Rodriguez [17]), with others more closely resembling the cochlear bud malformation (Romo [7], Robson [18]): Jackler [4] describes a mild and a severe form of hypoplastic cochlea as a developmental arrest during the sixth gestational week. Rodriguez [17] characterizes it by its reduced dimensions, the patients presenting with differing degrees of hearing loss depending on the exact time of the arrest. According to Rodriguez, the patients who show greater differentiation of the membranous labyrinth and more neuroepithelial elements have superior hearing. This aspect is also emphasized in the study by Zheng [19].
Romo [7] describes cochlear hypoplasia as a small rudimentary cochlear bud associated with a normal or malformed vestibule and SCCs. In severe cases of cochlear hypoplasia, the labyrinthine segment of the facial nerve can—according to a study by Romo [20]—be displaced anteromedially. This anterior migration was not, however, found in most of the patients with normal cochlear hypoplasia in our study.
Our finding of seven patients with cochlear hypoplasia accompanied by a large endolymphatic sac and duct is consistent with the findings of Davidson who found cochlear dysmorphism (mild and severe) in approximately 50% of his patients with large vestibular aqueduct syndrome (LVAS) [21].
Other authors also report the coexistence of a large endolymphatic duct and sac (LEDS) with other inner ear malformations in general; the frequency here varies between 15% and 50% [22–24].
Since the variability of cochlear hypoplasia was great, we further divided these into subgroups based on the length of the cochlear duct. No comparable radiological study was found. Zheng [19] presented a study of shortened cochleae from a histological point of view, in which he classified shortened cochlea into three groups, that however cover a much wider range of cochlear malformations than our study. His study clearly shows that most cochlear malformations are inadequately described by their bony appearance, and many features such as the length of the cochlear duct and the modiolus, hair cell loss, ganglion cell loss and the stria vascularis are important in terms of actual residual function; this also applies where cochlear implantation has been performed. It is not possible, however, to directly compare his results with our primarily radiological classification, which is based on easy visible criteria. Apart from the importance of ganglion and hair cell loss, Papsin [12] and Phelps [25] nevertheless underlined the clinical importance of the presence of even a rudimentary basal turn, since it implies that some auditory function is possible.
In the cases with only a basal turn and a wide lumen, the question arises as to how these should be differentiated from the common cavity described by Edward Cook [26]. In these cases, in particular, it is helpful to use his original description of a widely patent cochleovestibular duct (the connection between vestibulum and cochlea). To fit the definition of a common cavity, therefore, the requirements are twofold: a wide cochlea with no inner separation, and this wide connection with the vestibule. In those of our cases which we categorize as hypoplastic cochlea with a wide basal turn, this duct is of normal width. The use of the width of the cochleovestibular duct for differentiation purposes has already been described by Papsin [12].
Aberrant cochleae
We described three types of cochleae of smaller size—thus placing them in the category of hypoplastic cochleae, but which nevertheless cannot be explained solely in terms of developmental arrest theory (Fig. 5).
Our first aberrant type of cochlea is unusual because of its small or partially absent basal turn, but with a cochlear aperture. A differential diagnosis would be that of an otosclerosis. We consider this highly unlikely, however, because the appearance is identical on both sides in each of our two family cases (Fig. 5a, b).
In the literature, a kind of “dwarf cochlea” is mentioned by Som and Schuhknecht, but unfortunately no radiological images are available. The description of a dwarf cochlea might fit our second aberrant type of cochlea (Fig.5c), although Schuhknecht’s description and drawing indicate that this should be smaller but fully partitioned. Som also mentions two other unusual kinds of cochleae: a double cochlea and one with additional turns. We did not encounter any of these.
The third aberrant type of cochlea we described was found in only a single ear (Fig. 5d–f). With its characteristics—a shortened cochlea with less than two turns, a cystic apex formed from the end of the basal turn, and the small apical turn that follows it—it could conceivably be a combination of a short cochlea and a cystic apex found in true Mondini malformations (identical to incomplete partitions type II). A combination of two genetic defects would then be probable.
Conclusion
The term hypoplastic cochlea is very general; a further division into severe and less severe forms (the latter of which occur more frequently) based on the length of the cochlear duct can be made by visual inspection. Measurements can help the less experienced radiologist to reliably identify a hypoplastic cochlea.
The accompanying SCC malformations in cochlear bud malformations would appear to be more severe, becoming gradually less so in cases where a basal turn exists and in simple cochlear hypoplasia. Cochlear hypoplasia is a malformation that often involves not only the apical turn being reduced in size but also the basal turn being smaller in length.
In addition, cochlear malformations that cannot be explained in terms of Jackler’s gradual developmental arrest theory—such as a cystic apex together with a hypoplastic cochlea, or a kind of dwarf cochlea, do bear out the theory described by Papsin, namely that there must be multiple, isolated, independent paths of aberrant development.
A distinction must be made between the severe form in which only a basal turn is present, and a common cavity in which the duct between vestibulum and cochlea is much wider. If only a small bud exists, this malformation has to be distinguished from a complete aplasia of the cochlea.
The question remains of whether these subtypes, especially the hypoplastic cochleae, are clinically identifiable merely on the basis of their audiograms and other clinical tests. A more detailed subclassification of cochlear malformations—specifically, cochlear hypoplasia—can help enhance the comparison of CI outcome data. As yet, however, the question of whether the different length of the cochlear duct also implies a better outcome remains unanswered.
References
Lo WW (1999) What is a ‘Mondini’ and what difference does a name make? AJNR Am J Neuroradiol 20:1442–1444
Sennaroglu L, Saatci I (2002) A new classification for cochleovestibular malformations. Laryngoscope 112:2230–2241
Mondini C (1997) Minor works of Carlo Mondini: the anatomical section of a boy born deaf. Am J Otol 18:288–293
Jackler RK, Luxford WM, House WF (1987) Congenital malformations of the inner ear: a classification based on embryogenesis. Laryngoscope 97:2–14
Purcell D, Johnson J, Fischbein N et al (2003) Establishment of normative cochlear and vestibular measurements to aid in the diagnosis of inner ear malformations. Otolaryngol Head Neck Surg 128:78–87
Krombach GA, van den Boom M, Di Martino E et al (2005) Computed tomography of the inner ear: size of anatomical structures in the normal temporal bone and in the temporal bone of patients with Meniere’s disease. Eur Radiol 15:1505–1513
Romo LVC, JW RCD (2003) Temporal bone: congenital anomalies. In: Som P, Curtin H (eds) Head and neck imaging. Mosby, St Louis, pp 1109–1171
Schuknecht HF (1993) Pathology of the ear. Lea & Febiger, Malvern
Casselman JW, Offeciers FE, Govaerts PJ et al (1997) Aplasia and hypoplasia of the vestibulocochlear nerve: diagnosis with MR imaging. Radiology 202:773–781
Shim HJ, Shin JE, Chung JW et al (2006) Inner ear anomalies in cochlear implantees: importance of radiologic measurements in the classification. Otol Neurotol 27:831–837
Streeter GL (1948) Developmental horizons in human embryos. Description of age groups XV, XVI, XVII, and XVIII, being the third issue of a survey of the Carnegie Collection. Contrib Embryol 32:133–203
Papsin BC (2005) Cochlear implantation in children with anomalous cochleovestibular anatomy. Laryngoscope 115:1–26
Park AH, Kou B, Hotaling A et al (2000) Clinical course of pediatric congenital inner ear malformations. Laryngoscope 110:1715–1719
Ma H, Han P, Liang B et al (2008) Multislice spiral computed tomography imaging in congenital inner ear malformations. J Comput Assist Tomogr 32:146–150
Koch BL (2007) Labyrinthine aplasia. In: Barkovitch AJ (ed) Diagnostic imaging pediatric neuroradiology. Amirsys, Salt Lake City, pp II1-2–II1-3
Hudgins PA (2004) Labyrinthine aplasia. In: Harnsberger HR (ed) Diagnostic imaging head and neck. Amirsys, Salt Lake City, pp I2-96–I2-97
Rodriguez K, Shah RK, Kenna M (2007) Anomalies of the middle and inner ear. Otolaryngol Clin North Am 40:81–96, vi
Robson CD, Robertson RL, Barnes PD (1999) Imaging of pediatric temporal bone abnormalities. Neuroimaging Clin N Am 9:133–155
Zheng Y, Schachern PA, Cureoglu S et al (2002) The shortened cochlea: its classification and histopathologic features. Int J Pediatr Otorhinolaryngol 63:29–39
Romo LV, Curtin HD (2001) Anomalous facial nerve canal with cochlear malformations. AJNR Am J Neuroradiol 22:838–844
Davidson HC, Harnsberger HR, Lemmerling MM et al (1999) MR evaluation of vestibulocochlear anomalies associated with large endolymphatic duct and sac. AJNR Am J Neuroradiol 20:1435–1441
Jackler RK, De La Cruz A (1989) The large vestibular aqueduct syndrome. Laryngoscope 99:1238–1242, discussion 1242–1233
Valvassori GE (1983) The large vestibular aqueduct and associated anomalies of the inner ear. Otolaryngol Clin North Am 16:95–101
Koesling S, Rasinski C, Amaya B (2006) Imaging and clinical findings in large endolymphatic duct and sac syndrome. Eur J Radiol 57:54–62
Phelps PD (1990) Mondini and ‘pseudo Mondini’. Clin Otolaryngol Allied Sci 15:99–101
Cock E (1838) A contribution to the pathology of congenital deafness. Guys Hosp Rep 7:289–307
Conflict of interest statement
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Giesemann, A.M., Goetz, F., Neuburger, J. et al. Appearance of hypoplastic cochleae in CT and MRI: a new subclassification. Neuroradiology 53, 49–61 (2011). https://doi.org/10.1007/s00234-010-0777-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-010-0777-3