Abstract
Introduction
Vertebrobasilar artery occlusion (VBO) produces high mortality and morbidity due to low recanalization rate utilization in endovascular therapy. The use of percutaneous transluminal angioplasty (PTA) to improve recanalization rate additional to local intra-arterial fibrinolysis (LIF) was investigated in this study. Results obtained following recanalization therapy in acute intracranial VBO are reported.
Methods
Eighteen consecutive patients with acute VBO underwent LIF with or without PTA, from August 2000 to May 2006. Eight patients were treated using LIF alone, and ten required additional PTA. Rate of recanalization, neurological status before treatment, and clinical outcomes were evaluated.
Results
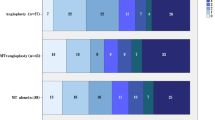
Of 18 patients, 17 achieved recanalization. One procedure-related complication of subarachnoid hemorrhage occurred. Overall survival rate was 94.4% at discharge. Seven patients achieved good outcomes [modified Rankin scale (mRS) 0–2], and the other 11 had poor outcomes (mRS 3–6). Five of six patients who scored 9–14 on the Glasgow Coma Scale (GCS) before treatment displayed good outcomes, whereas ten of 12 patients who scored 3–8 on the GCS showed poor outcomes. GCS prior to treatment showed a statistically significant correlation to outcomes (p < 0.05). Moreover, the National Institutes of Health Stroke Scale (NIHSS) before treatment correlated well with mRS (correlation coefficient 0.487). No statistical difference between the good and poor outcome groups was observed for the duration of symptoms, age, etiology, and occlusion site.
Conclusions
Endovascular recanalization can reduce mortality and morbidity of acute VBO. Good GCS and NIHSS scores prior to treatment can predict the efficacy of endovascular recanalization.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acute vertebrobasilar artery occlusion leads to poor morbidity and mortality, even following anticoagulation and platelet inhibitor therapy, with the mortality rate with anticoagulation therapy reported to be approximately 90% [1]. Several reports have shown that local intra-arterial fibrinolysis (LIF) of vertebrobasilar artery occlusion can improve mortality and morbidity. However, recanalization rates are relatively low, and mortality has remained high, at ∼60%, even with the use of LIF [1–5]. In patients with embolic vertebrobasilar artery occlusion, the embolus is often so large as to be resistant to LIF and requires high doses of fibrinolytic agents, which can cause hemorrhagic complications. In patients with atherothrombotic occlusion, recanalization can rarely be obtained by LIF alone. Furthermore, residual high-grade stenosis usually remains after recanalization, which often causes reocclusion. The reocclusion rate after LIF has been reported to be 10–30% [2, 6]. Percutaneous transluminal angioplasty (PTA) has been developed for the treatment of intracranial atherosclerotic stenosis. Some investigators have applied PTA for acute occlusion, which can lead to higher recanalization rates and decrease morbidity. However, few reports have described the efficacy and safety of PTA for the treatment of acute intracranial vertebrobasilar artery occlusion in a large number of cases. In this study, retrospective analysis of patients with acute vertebrobasilar artery occlusion treated using LIF with or without PTA, in our institutions, was performed. This study, therefore, aimed to establish the factors increasing survival rate and good neurological outcomes.
Methods
Patients
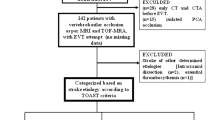
Endovascular treatment of vertebrobasilar artery occlusion included patients admitted with neurological symptoms who were subsequently found to have vertebrobasilar artery occlusion using magnetic resonance angiography (MRA) and/or computed tomography (CT). Exclusion criteria for endovascular recanalization were a large brain stem infarction [more than half the area of the brain stem on at least one axial slice of CT and/or magnetic resonance imaging (MRI)], recent history (within 4 weeks) or presence of intracranial hemorrhage or hemorrhagic infarction, or long duration after onset (>12 h). From August 2000 to May 2006, 18 consecutive patients [14 males and four females, aged 50–84 years (mean age 69.9 years)] with acute intracranial vertebrobasilar artery occlusion underwent endovascular recanalization therapy at our institutions, including LIF using urokinase and PTA. Informed consent for endovascular treatment was obtained from each patient and/or their nearest relatives. Their clinical findings, angiograms, and outcomes are summarized in Table 1. The duration between the onset of neurological symptoms and endovascular recanalization therapy ranged from 1 to 8.5 h. The median Glasgow Coma Scale (GCS) score on admission was 7 (range 3–14). The median National Institutes of Health Stroke Scale (NIHSS) was 20.5 (range 3–35). Among the 18 patients, etiology of occlusion was cardiogenic embolism in 11 patients and atherothrombotic occlusion in seven patients. All patients underwent noncontrast brain CT before treatment to exclude hemorrhagic transformation of brain parenchyma and diffuse brain stem infarction. MRI and MRA were performed in all but three patients. Neurosurgeons and/or neurologists estimated neurological status before treatment and scored with the GCS and NIHSS. Clinical outcomes at 3 months were classified using the modified Rankin scale (mRS). Mean hospitalization days and follow-up days were 61.4 and 697, respectively.
Angiography and interventions
In most cases, a transfemoral arterial or a brachial arterial approach was taken for transarterial digital subtraction angiography of the aortic arch, bilateral vertebral arteries, and bilateral common carotid arteries. The site of vertebrobasilar artery occlusion was categorized as: distal vertebral artery (VA), intracranial portion of the VA; proximal basilar artery (BA), from the vertebral arterial confluence to the origin of the anterior inferior cerebellar artery; mid-BA, from the origin of the anterior inferior cerebellar artery to the origin of the superior cerebellar artery; distal BA, distal to the superior cerebellar artery. Collateral flow that opacified the BA from the tip inferiorly to the level of the superior cerebellar arteries was termed distal, while collateral flow that opacified the BA from the tip to below the level of the anterior inferior cerebellar arteries was termed distal and middle. The number of collateral opacification of the P1 segment of the posterior cerebral artery (from the basilar tip to the confluence of the posterior communicating artery (PcoA)) was also recorded. At least one P1 segment could be obtained from nine patients via carotid injections. One P1 segment with leptomeningeal collateral flow via vertebral injections was also obtained from one patient.
All procedures were performed under local anesthesia with intravenous injection of heparin (1,500–3,000 U); patients with poor GCS required intubation, but no patients underwent intravenous anesthetics or inhalation anesthetics. A microcatheter was advanced distally beyond the occlusion site through a guiding catheter which was placed at the cervical portion of the VA. Urokinase was infused at a rate of 60,000 U every 5 min. During urokinase infusion, the tip of the microcatheter was slowly pulled back to the proximal portion of the occlusion site, and angiography was performed after every injection of 60,000 U to estimate recanalization. When no or minimal thrombus regression was observed on angiography after injection of 120,000 U of urokinase, PTA was performed using a small balloon catheter with a balloon diameter 0.5–1 mm less than the estimated arterial diameter and a low inflation pressure (<4 atmospheric pressure; Fig. 1). Selection of PTA balloon catheter depended on the operator, i.e., 5 Gateway (Boston Scientific, Natick, MA, USA), 4 fasSTEALTH (Boston Scientific), and 1 Sasuga (Boston Scientific). When recanalization was obtained after PTA, additional infusion of urokinase was performed until sufficient lysis of the residual thrombus in the vertebral BA was obtained, or 360,000 U of urokinase was infused. Total dosage of urokinase used ranged from 120,000 to 360,000 (mean 228,000) U. Eight patients were treated with LIF alone, and ten patients were treated with LIF and additional PTA. Six of the seven patients with atherothrombotic occlusion were treated using LIF and additional PTA. Seven out of 11 patients with cardiogenic thromboembolism were treated by LIF alone. Follow-up CT scanning was performed immediately, 12 h, 24 h, and 3 days after the procedure. Continuous intravenous infusion of heparin (10,000 to 15,000 U/day) was performed for 3 days after the procedure. Antiplatelets were administrated after endovascular procedure for all cases of atherothrombotic occlusion. In contrast, no cases of cardiogenic thromboembolism were treated with antiplatelets.
A 77-year-old man (case 12) with sudden-onset loss of consciousness and quadriparesis at the time of presentation. Pretreatment GCS score was 5. a Initial noncontrast CT shows the high density of the basilar tip. b Diffusion-weighted image showing the absence of high signal intensity area in the brain stem. c MRA shows occlusion of the distal portion of the basilar artery. The right posterior cerebral artery shown was most likely supplied via the right posterior communicating artery. d Cerebral angiography, started 3.5 h after onset, shows that the tip of the basilar artery was occluded with a thrombus. Both posterior cerebral arteries and the right superior cerebellar artery cannot be seen. e A microcatheter was introduced beyond the thrombus; 120,000 U urokinase was injected slowly. The right posterior cerebral artery and the superior cerebellar artery could not be seen after this procedure; however, the residual thrombus occluded the left posterior cerebral artery. PTA was performed from the distal basilar artery to the left posterior cerebral artery. Recanalization was achieved immediately. Another 60,000 U urokinase was injected to resolve the distal embolism. f Final angiography shows complete recanalization of the basilar artery; however, the slow blood flow caused by the distal embolism can be seen in the right superior cerebellar artery and left posterior cerebral artery. g, h Diffusion-weighted images performed 8 days after the procedure show no brain stem infarction and minimal left thalamic infarction. The cortical infarction of the left posterior lobe is an old infarction which existed before onset. The patient had mild right hemiparesis and an mRS of 3
Recanalization rate, complications, and clinical outcomes were evaluated. Recanalization was classified with arterial occlusive lesion score (AOL score) [7] which focused on recanalization of the primary arterial occlusive lesion. The AOL score was defined as: 0 = no recanalization of the primary occlusion, I = incomplete or partial recanalization of the primary occlusion with no distal flow, II = incomplete or partial recanalization of the primary occlusion with distal flow, or III = complete recanalization of the primary occlusion with distal flow. We also analyzed the relationship between neurological outcomes and factors potentially affecting these outcomes, including age, duration before treatment, sites of occlusion, etiology of occlusion, use of additional PTA, GCS, and NIHSS before treatment. All statistical analyses were performed using SPSS version 10.0.7 J software. Student’s t test, Fisher’s exact test, χ 2 test, and Pearson’s product moment correlation coefficient were used.
Results
Vertebrobasilar artery occlusion as observed with vertebral angiography was found in the distal VA in two patients, mid-BA in six patients, and distal BA in ten patients. In both patients with distal VA occlusion, contralateral vertebral angiography showed hypoplasty of the contralateral VA. Two of the ten patients with distal BA occlusion showed concurrent occlusion of the VA at the origin and hypoplasty of the contralateral VA.
Collateral opacification of the distal BA beyond the occlusion site and the P1 segment of the posterior cerebral artery are shown in Table 1. Distal BA opacification from collaterals could be estimated only when the occlusion site was below the mid-BA. Six patients with mid-BA occlusion were observed. Three patients displayed no collateral distal basilar flow, while three were observed with retrograde collateral flow via PcoA or leptomeningeal anastomosis. There was no correlation between the opacification of the distal BA and mRS (Table 2). Two patients with distal VA occlusion revealed retrograde distal to middle BA opacification in one patient and no retrograde BA opacification in the other. The outcomes were the same as mRS 1. There was no significant correlation between the opacification number of P1s and mRS (Table 2). However, a trend showed that only 20.0% of patients could achieve good outcomes when no P1 opacification was observed. By contrast, 50.0% of patients showed good outcomes when at least one P1 opacification site was present.
Technical results and complications
Recanalization was achieved in 17 of the 18 patients (94.4%). After LIF using 120,000 U urokinase, complete recanalization (AOL III) was obtained in six patients; partial recanalization (AOL II) was found in five, and no recanalization (AOL 0) was found in seven patients. No patients had minimal recanalization without distal flow (AOL I). Additional PTA was performed in all seven patients of AOL 0 and in three of the five patients classified as AOL II. Finally, recanalization of the vertebrobasilar artery was obtained in 17 out of 18 patients, which included nine complete recanalizations without residual stenosis or thrombi at the occlusion site (AOL III) and eight incomplete recanalizations with residual filling defects or stenosis (AOL II). All nine cases which showed complete recanalization had cardiogenic embolism due to atrial fibrillation. Among the eight patients who showed incomplete recanalization, all except two had atherothrombotic occlusion. The remaining patient suffered subarachnoid hemorrhage caused by penetration of the microguidewire during its passage through the occlusion site of the BA. The procedure was, therefore, interrupted in this patient and resulted in no recanalization (AOL 0).
Acute or subacute reocclusion was not observed. Two patients who had been recanalized with PTA showed restenosis 1 month after the procedures and were retreated by stenting. Hemorrhagic infarction after the procedure was observed in four patients on follow-up CT. In three patients, petechial hemorrhagic changes that did not affect the outcomes were found in the occipital lobe. Massive symptomatic hematoma was observed in one patient, which caused severe neurological aggravation. No other complications relating to the procedures were observed.
Clinical outcomes and related factors
Outcomes at discharge or 3 months after treatment were favorable (mRS 0–2) in seven patients (38.9%) and poor (mRS 3–6) in 11 patients (61.1%). During a follow-up period of 0–62 months (mean 22.9 months), one patient died 23 days after the procedure due to pneumonia. Good outcomes were more frequently observed in patients with atherothrombotic occlusion (43%) than in those with cardiogenic thromboembolism (36%); however, there was no statistically significant difference between both etiologic groups (Table 3).
No statistical relationship was shown between AOL score after treatment and mRS.
Both patients whose clots were located at the distal VA showed good neurological outcomes, as did five of the 16 patients (31.3%) with mid-BA or distal BA occlusion. Although patients with mid-BA/distal BA occlusion tended to show poorer outcomes than those with proximal occlusion, statistical analysis showed no correlation between outcomes and site of occlusion.
The mean duration between onset of symptoms and start of endovascular procedure was similar in both the good- (260 and 60–445 min) and poor-outcome groups (250 and 110–510 min).
Five out of six patients (83.3%) who scored 9–14 on the GCS before treatment showed good outcomes. By contrast, only two of 12 patients who scored 3–8 on the GCS recovered well. There was a statistically significant correlation between GCS score before treatment and neurological outcomes (p = 0.013).
Pearson’s correlation coefficient was 0.487 between NIHSS and mRS which demonstrated a significant correlation. As NIHSS score increased, so did observed mRS. All the patients who demonstrated an NIHSS greater than 29 returned an mRS of 5 or 6.
No significant correlation between outcomes and age was observed.
Etiology and related factors
No differences were found in ages and mean number of occlusion of PCA and SCA after procedure in both etiologies. Patients with cardiogenic thromboembolism tended to have poor GCS score and NIHSS than the patients with atherothrombotic occlusion. Atherothrombotic occlusion required additional PTA (6 of 7) more frequently, and therefore, it required longer procedure time (199 min) than cardiogenic thromboembolism (requirement of PTA, four of 11; procedure time, 122 min). However, there were no statistically significant differences between both etiologies in those factors. A significant difference was found in AOL score which shows lower in atherothrombotic occlusion (1.71) than in cardiogenic thromboembolism (2.73; p = 0.01; Table 4).
Use of additional PTA
There were eight patients treated by LIF alone (LIF group) and ten patients treated by LIF and additional PTA (PTA group). PTA group included larger number of atherothrombotic occlusion (six of ten patients) than LIF group (one of eight patients). The mean ages, initial GCS, and NIHSS were similar in both groups. PTA group showed slightly longer procedure time (164 vs. 143 min), slightly lower AOL score (2.10 vs. 2.63), and better outcome (good outcome: 50% vs. 25%). However, there were no statistically significant differences (Table 5).
Discussion
Acute intracranial vertebrobasilar artery occlusion is often associated with high morbidity and mortality, even when treated with anticoagulation and platelet inhibitors [1]. During the last two decades, several authors have reported the efficacy of LIF for the treatment of occluded vertebrobasilar artery. However, reports of recanalization rates were low (44–65%), and mortality rates were still high (>50%) [1–5]. A higher recanalization rate was considered to lead to a lower mortality rate. Hacke et al. [1] reported that the recanalization rate by LIF was 44%, and the mortality rate was 69%. Recently, Arnold et al. [8] reported that the recanalization rate by LIF and PTA was 80%, and the mortality rate was 42%. Ezaki et al. [9] reported similar results, with a recanalization rate for LIF and PTA of 92% and a mortality rate of 27%. Approximately 10% of patients were treated with PTA in these studies [8, 9]. More recently, Eckert et al. [10] reported the results of a multicenter study of aggressive therapy with intravenous abciximab and intra-arterial rtPA, and additional PTA/stenting, in 47 patients with acute vertebrobasilar occlusion. Balloon PTA or stenting was performed in 31.9% of patients, resulting in a 72% recanalization rate and a 38% mortality rate. These results suggest that higher recanalization rates may be related to lower mortality. Lindsberg et al. [11] reported the systematic analysis of the treatment for vertebrobasilar artery occlusion. From their data, successful recanalization was a decisive factor in promoting good outcomes, as the likelihood of good outcomes in the nonrecanalized cases was only 2%. In the present study, we achieved 94% recanalization and 94% survival. PTA was performed in 55.5% of patients who had residual stenosis/thrombus after LIF with a small dosage of urokinase (120,000 U). Prolonged infusion of thrombolytic agents in LIF-resistant patients, such as those with firm clots or atherothrombotic occlusion, may lead to lower recanalization and increased risk of hemorrhagic complications. PTA can immediately restore blood flow in the stenotic or occlusive artery by crushing the clots or dilation of the atherosclerotic stenosis. Additional PTA in the procedure would be a major contributor to the high recanalization rates and good outcomes in our study. The dose of urokinase used (mean 228,000 U) was less than that in other reports (400,000–1,800,000 U) [1–6, 8, 9]. Massive hemorrhagic transformation is one of the most important complications associated with endovascular recanalization. This complication occurred after treatment of acute vertebrobasilar artery occlusion in 8–25% of previously reported cases. Only one case (5.6%) in our study showed symptomatic hemorrhage after treatment. The lower incidence of hemorrhagic complications may be related to good outcomes and may have been caused by the low dosage of urokinase. Therefore, early judgment of LIF-resistant occlusion and additional PTA could be associated with good outcome. However, there are potential risks of balloon PTA for acute occlusion of intracranial arteries, which include arterial dissection, subarachnoid hemorrhage, and acute occlusion, which can be fatal. Nahser et al. [12] have discussed their experiences of 20 patients with vertebrobasilar artery stenosis treated by balloon angioplasty and presented a review of 126 published cases. From their data, angiographic complications occurred in seven patients (8.2%; five dissections, one acute occlusion of the BA, and one perforating occlusion), of which four (4.7%) were fatal. No dissection was encountered in our study. We performed balloon angioplasty using a small caliber balloon (0.5–1 mm less than the ideal size) inflated gently with low pressure (<4 atm). Use of these techniques may reduce the risk of angioplasty-related vessel injury. We experienced one complication directly related to the procedure, in which a microguidewire penetrated the BA during navigation through the occluded portion of the artery. The penetrated portion of the BA was occluded, and CT following the procedure showed only a small subarachnoid hemorrhage. The complication seemed not to worsen patient outcomes. However, careful attention should be practiced when manipulating the catheter and guidewire through the occluded portion of the artery. Another potential disadvantage of balloon PTA is clot disruption and dislocation especially in cases of cardiogenic embolism, which can cause distal embolisms and occlusion of perforators. Recent developing technique of clot retrieval such as suction catheters technique and mechanical clot retriever might have an advantage in order to remove large clots without clot disruption in cases of cardiogenic thromboembolism [13–18]. These reports consisted of a small number of cases, and further investigations would be required. The utility of these extraction and thrombectomy devices for acute vertebrobasilar artery occlusion is limited to patients with embolic occlusion, who constitute less than half of patients. It would be easier to perform LIF with additional PTA than to use extraction/thrombectomy devices for the treatment of acute vertebrobasilar occlusion.
Other factors may affect patient outcomes. Brandt et al. [3] reported that distal BA occlusion and atherothrombotic occlusion tended to show high mortality. Atherothrombotic occlusion also showed significant resistance to recanalization. By contrast, Cross et al. [19] showed better neurological outcomes in patients with distal basilar thrombosis, where the survival rate in patients with distal BA occlusion was significantly higher than in those with proximal and middle BA occlusion (71 versus 15%). Furthermore, this study mentioned that distal BA occlusion is frequently of embolic origin and can often be recanalized by LIF. In our study, good outcomes were more frequently observed in patients with atherothrombotic occlusion than in those with cardiogenic thromboembolism (43% versus 36%). Regarding the site of occlusion, mid-BA/distal BA occlusion tended to show poorer outcomes than proximal occlusion. These differences in outcomes may have been caused by the different techniques used and the recanalization rates. Our technique using additional balloon PTA achieved a recanalization rate of 94% and 94% survival. Therefore, duration of ischemia and collateral blood flow are more important than the nature of the occlusion resistant to LIF. Cross et al. [4] demonstrated that most patients (83%) who had good collateral flow also had good neurological prognosis. These results suggest that recanalization of atherothrombotic occlusion of the vertebrobasilar artery may give good neurological outcomes when patients have good collateral blood flow. We investigated collateral flows in relation to distal basilar trunk opacification, PcoA visualization, and P1 segment visualization. There was no significant correlation between the above items and mRS. However, there was a slight tendency that, when a patient had at least one P1 opacification, five of ten patients (50.0%) showed good outcomes, indicating that better outcomes occur with atherothrombotic occlusion. Cardiogenic thromboembolisms can occlude the distal portion of the BA, so simultaneous occlusion of the P1 segment of the posterior cerebral artery can easily occur.
Pretreatment GCS can reflect severity of brain stem ischemia and was significantly correlated to outcomes in our study and in previous studies. We found that patients who scored >8 on the GCS had significantly better outcomes than patients who scored 3–8. Arnold et al. [8] reported that low NIHSS scores (<20) are predictive of favorable outcomes. Our results also showed NIHSS had a significant correlation coefficient with mRS. Ezaki et al. [9] reported that patients with a GCS score of <10 upon admission had a worse prognosis. The present study demonstrated that the initial condition of a patient is a predictor of outcomes.
The duration of ischemia before treatment may influence patient outcomes. Eckert et al. [5] reported that early treatment within 6 h of onset leads to significantly better neurological outcomes than delayed treatment. Arnold et al. [8] also reported that recanalization could be performed more frequently in cases treated within 6 h and that recanalization itself is an independent predictor of favorable outcomes. However, our results showed no difference in the mean duration of ischemia between the good-outcome and poor-outcome groups. Further investigations are necessary to determine the therapeutic time window that will achieve the best results.
Stenting for acute occlusion was not performed in our study, although two patients were treated using stenting for vertebrobasilar artery restenosis. Spreer et al. [20] reported three cases of primary stenting for residual stenosis immediately after LIF. There have been a few reports [10, 20–22] of intracranial stenting for vertebrobasilar artery occlusion after LIF. Eckert et al. [10] reported that additional PTA/stenting was performed after LIF in 31.9% of patients. However, they did not describe these cases in detail, such as the number of cases, efficacy, and complications. Levy et al. [23, 24] compared the safety of intracranial stenting for severe vertebrobasilar artery stenosis using three different methods: direct stenting without predilatation, stenting with predilatation, and staged stenting following balloon PTA. Direct stenting for acute vertebrobasilar artery occlusion was shown to possibly have a higher risk of complications than LIF with additional balloon PTA using a low inflation pressure.
There are possible factors affecting the results of this study. First, we used MR images for exclusion of patients. Evaluation by MRI, especially when using diffusion-weighted image before treatment, might increase patients who met exclusion criteria compared with CT evaluation alone. Second, we perform all procedure under local anesthesia because it can be performed immediately after diagnostic angiography without duration of preparing general anesthesia. Shorter duration after onset (within 12 h) than other articles (within 18–79 h) [1–5] might influence our good survival rate.
Conclusion
PTA can feasibly be performed after LIF in patients with acute vertebrobasilar artery occlusion. Although our study was limited by the small number of cases, we achieved a high recanalization rate and low mortality. Furthermore, a notable strong correlation of pretreatment GCS score with outcomes was observed.
References
Hacke W, Zeumer H, Ferbert A, Bruckmann H, del Zoppo GJ (1988) Intra-arterial thrombolytic therapy improves outcome in patients with acute vertebrobasilar occlusive disease. Stroke 19:1216–1222
Becker KJ, Monsein LH, Ulatowski J, Mirski M, Williams M, Hanley DF (1996) Intra-arterial thrombolysis in vertebrobasilar occlusion. AJNR Am J Neuroradiol 17:255–262
Brandt T, von Kummer R, Muller-Kuppers M, Hacke W (1996) Thrombolytic therapy of acute basilar artery occlusion. Variables affecting recanalization and outcome. Stroke 27:875–881
Cross DT 3rd, Moran CJ, Akins PT, Angtuaco EE, Diringer MN (1997) Relationship between clot location and outcome after basilar artery thrombolysis. AJNR Am J Neuroradiol 18:1221–1228
Eckert B, Kucinski T, Pfeiffer G, Groden C, Zeumer H (2002) Endovascular therapy of acute vertebrobasilar occlusion: early treatment onset as the most important factor. Cerebrovasc Dis 14:42–50
Zeumer H, Freitag HJ, Zanella F, Thie A, Arning C (1993) Local intra-arterial fibrinolytic therapy in patients with stroke: urokinase versus recombinant tissue plasminogen activator (r-TPA). Neuroradiology 35:159–162
Khatri P, Neff J, Broderick JP, Khoury JC, Carrozzella J, Tomsick T (2005) Revascularization end points in stroke interventional trials: recanalization versus reperfusion in IMS-I. Stroke 36:2400–2403
Arnold M, Nedeltchev K, Schroth G, Baumgartner RW, Remonda L, Loher TJ, Stepper F, Sturzenegger M, Schuknecht B, Mattle HP (2004) Clinical and radiological predictors of recanalisation and outcome of 40 patients with acute basilar artery occlusion treated with intra-arterial thrombolysis. J Neurol Neurosurg Psychiatry 75:857–862
Ezaki Y, Tsutsumi K, Onizuka M, Kawakubo J, Yagi N, Shibayama A, Toba T, Koga H, Miyazaki H (2003) Retrospective analysis of neurological outcome after intra-arterial thrombolysis in basilar artery occlusion. Surg Neurol 60:423–430
Eckert B, Koch C, Thomalla G, Kucinski T, Grzyska U, Roether J, Alfke K, Jansen O, Zeumer H (2005) Aggressive therapy with intravenous abciximab and intra-arterial rtPA and additional PTA/stenting improves clinical outcome in acute vertebrobasilar occlusion: combined local fibrinolysis and intravenous abciximab in acute vertebrobasilar stroke treatment (FAST): results of a multicenter study. Stroke 36:1160–1165
Lindsberg PJ, Mattle HP (2006) Therapy of basilar artery occlusion: a systematic analysis comparing intra-arterial and intravenous thrombolysis. Stroke 37:922–928
Nahser HC, Henkes H, Weber W, Berg-Dammer E, Yousry TA, Kuhne D (2000) Intracranial vertebrobasilar stenosis: angioplasty and follow-up. AJNR Am J Neuroradiol 21:1293–1301
Bose A, Henkes H, Alfke K, Reith W, Mayer TE, Berlis A, Branca V, Sit SP (2008) The penumbra system: a mechanical device for the treatment of acute stroke due to thromboembolism. AJNR Am J Neuroradiol 29:1409–1413
Mayer TE, Hamann GF, Brueckmann H (2002) Mechanical extraction of a basilar-artery embolus with the use of flow reversal and a microbasket. N Engl J Med 347:769–770
Mayer TE, Hamann GF, Schulte-Altedorneburg G, Bruckmann H (2005) Treatment of vertebrobasilar occlusion by using a coronary waterjet thrombectomy device: a pilot study. AJNR Am J Neuroradiol 26:1389–1394
Mangiafico S, Cellerini M, Nencini P, Gensini G, Inzitari D (2005) Intravenous glycoprotein IIb/IIIa inhibitor (tirofiban) followed by intra-arterial urokinase and mechanical thrombolysis in stroke. AJNR Am J Neuroradiol 26:2595–2601
Versnick EJ, Do HM, Albers GW, Tong DC, Marks MP (2005) Mechanical thrombectomy for acute stroke. AJNR Am J Neuroradiol 26:875–879
Chapot R, Houdart E, Rogopoulos A, Mounayer C, Saint-Maurice JP, Merland JJ (2002) Thromboaspiration in the basilar artery: report of two cases. AJNR Am J Neuroradiol 23:282–284
Cross DT 3rd, Moran CJ, Akins PT, Angtuaco EE, Derdeyn CP, Diringer MN (1998) Collateral circulation and outcome after basilar artery thrombolysis. AJNR Am J Neuroradiol 19:1557–1563
Spreer J, Els T, Hetzel A, Arnold S, Klisch J, Huppertz HJ, Oehm E, Schumacher M (2002) Primary stenting as emergency therapy in acute basilar artery occlusion. Neuroradiology 44:791–795
Phatouros CC, Higashida RT, Malek AM, Smith WS, Mully TW, DeArmond SJ, Dowd CF, Halbach VV (1999) Endovascular stenting of an acutely thrombosed basilar artery: technical case report and review of the literature. Neurosurgery 44:667–673
Callahan AS 3rd, Berger BL (2000) Basilar artery endoprosthesis placement: rescue therapy for recurrent thrombosis. J Neuroimaging 10:47–48
Levy EI, Hanel RA, Bendok BR, Boulos AS, Hartney ML, Guterman LR, Qureshi AI, Hopkins LN (2002) Staged stent-assisted angioplasty for symptomatic intracranial vertebrobasilar artery stenosis. J Neurosurg 97:1294–1301
Levy EI, Hanel RA, Boulos AS, Bendok BR, Kim SH, Gibbons KJ, Qureshi AI, Guterman LR, Hopkins LN (2003) Comparison of periprocedure complications resulting from direct stent placement compared with those due to conventional and staged stent placement in the basilar artery. J Neurosurg 99:653–660
Conflict of interest statement
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kashiwagi, J., Kiyosue, H., Hori, Y. et al. Endovascular recanalization of acute intracranial vertebrobasilar artery occlusion using local fibrinolysis and additional balloon angioplasty. Neuroradiology 52, 361–370 (2010). https://doi.org/10.1007/s00234-010-0658-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-010-0658-9