Abstract
Introduction
We hypothesized that magnetic resonance imaging (MRI) can assess fetuses with sonographically (ultrasonography (US))-suspected neural tube defects (NTD) that might influence their diagnoses and management decision.
Methods
Institutional review board approval and informed consents were obtained to perform MRI for 19 fetuses referred with US-suspected NTD. Prenatal imaging findings were correlated with management decision, postnatal clinical, postnatal imaging, and pathology.
Results
Prenatal MRI correctly ruled out US diagnosis of cephalocele in a fetus. In the other 18 fetuses, MRI detected detailed topography and contents of NTD sacs in five, added central nervous system (CNS) abnormalities that were not apparent on US in three, and confirmed non-CNS findings in three fetuses. MRI changed diagnosis of 3/19 fetuses (15.8%), caused minor change in diagnosis of 5/19 (26.3%), and did not influence US diagnosis of 11/19 fetuses (57.9%). MRI findings changed/modified management decision in 21% of the fetuses.
Conclusion
Fetal MRI is an important adjunct to US in assessing NTD. It can identify topography and contents of sacs, add CNS and non-CNS findings, and influence management decision.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Neural tube defects (NTDs) are a heterogeneous group of malformations resulting from failure of normal neural tube closure early in the embryologic development [1]. NTDs include cranial presentations, such as anencephaly and cephalocele, as well as spinal presentations that include spina bifida, and less commonly, iniencephaly. Closed or open NTD describes the presence or absence of skin covering the defect [2]. The inheritance of NTD is multifactorial; it includes non-syndromal sporadic/familial NTDs and syndromal NTDs such as Meckel–Gruber syndrome. The estimated recurrence risk for a sporadic NTD in siblings is 2–5%, a 50-fold increased risk over that observed in general population, and 25% in autosomal recessive disorders such as Meckel–Gruber syndrome [1].
Prenatal investigations of NTD include measurements of the maternal serum alpha-fetoprotein (AFP). However, elevated AFP is only helpful in detecting open NTD along with a list of fetal anomalies that are associated with an elevated AFP such as omphalocele, Turner syndrome, oligohydramnios, and sacrococcygeal teratoma [3, 4]. Prenatal imaging of NTD is of utmost importance as the prognosis of the anomaly varies based on its type, size, location, involvement of neural tissues, as well as associated syndromes [4, 5].
Clinicians usually refer their patients for a targeted ultrasonography (US) examination once NTD has been suspected. Although sonography remains the primary imaging technique for evaluating the developing fetus, significant limitations may exist [2]. These limitations are largely due to obscuration of portions of fetal intracranial anatomy caused by reverberative artifacts of the bony calvarium, engagement of the fetal head deep in the maternal pelvis, and to the low sensitivity of fetal sonography to some brain malformations. Sonographic evaluation of the fetal head and spine can also be hampered by oligohydramnios and maternal body habitus [6].
Magnetic resonance imaging (MRI) does not suffer from these restraints and has higher intrinsic sensitivity than sonography to contrast between various fetal central nervous system (CNS) tissues [7]. With its superior spatial and contrast resolution, MRI is a potential prenatal imaging modality of suspected NTD that might provide anatomic information not previously available for counseling-management decision [8–10].
With the expanding role of in utero surgery, the coordinated effort of many specialists, including pediatric surgeons, neurosurgeons, maternal-fetal medicine specialists, ultrasonographers, and radiologists, with MRI expertise are required [9, 10]. Whether MRI adds value in the prenatal evaluation of NTDs needs further investigations [11–14].
The aim of this study is to determine the diagnostic utility of fetal MRI in fetuses with suspicious sonographic findings for NTD, especially in the presence of US technical difficulties, and to weigh the impact of MRI findings on parents counseling and pregnancy management.
Methods
Subjects
Nineteen fetuses with suspicious US findings for NTDs were enrolled for fetal MRI in this institutional review board-approved study between March 2006 and February 2008. A written informed consent was obtained from each expectant mother prior to MR examination. The mean maternal age was 25 years (range 21–40). All pregnancies were singleton with a median gestational age (GA) of 23 weeks SD 5.9 (range 19–39 weeks). The GA was based on the last menstrual period and the earliest US biometric measurements done during the pregnancy.
Suspected NTD referral diagnosis was according to detailed neurosonographic 2D and 3D studies performed by three of the authors (E A E-K, M A-R, and MS) with 7–20 years experience in obstetric US imaging (average 15.6 years) using 2.5–5.0 MHz transducers of Accuvix XQ (Medison, Seoul, Korea) or Voluson E8 (GE healthcare, Milwaukee, WI, USA) ultrasound scanners. Vaginal US with 4–8 or 6–12 MHz transducers was performed when the fetus was in cephalic position or when the fetus was in breech position and there was a suspected spinal abnormality. US studies were done with knowledge of the patient’s history.
Methods
MRI was performed with 1.5 T superconducting magnet (Intera, Philips Medical Systems, Best, Netherlands) using a phased-array surface coil. No patients were excluded because of contraindication to MRI or claustrophobia. Most patients were positioned supine and head first into the gantry. Patients who could not lie supine were put in the left lateral position. CNS images were obtained in the fetal sagittal, coronal, and transverse planes. Each new acquisition was prescribed by using images from the immediately prior acquisition to avoid the misregistration caused by fetal movement.
T2-weighted images were obtained using SSh/TSE sequence (Philips proprietary version of single shot fast spin echo using repetition time TR/echo time TE 10,000/100 msec, 4 mm slice thickness with no intersection gap, matrix 196 × 256 or 256 × 256) and balanced fast field echo (b-FFE) sequence (Philips proprietary version of steady state free precession: TR/TE 3.5–4/1.7–2 msec, flip angle (FA) 60–90, 1–2 signals acquired, 256 × 256 matrix, and 4 mm slice thickness with no inter-slice). The smallest field of view was used to allow for visualization of fetal anatomy without aliasing artifact from wraparound of the maternal anatomy. T1-weighted MR images were obtained by using a breath-hold spoiled gradient echo sequence (TR/TE: 100–140/4.2 msec, 70–90°FA, 256 × 160–256 matrix, one signal acquired, slice thickness between 4 and 6 mm with an inter-slice gap of 0.2–0.4 mm). No contrast agent or sedative was used.
All fetal MRI studies were conducted by two radiologists (S N S, N M) with 10- and 1-year experience in fetal MRI, respectively. Data obtained by the radiologist at the time of MRI included referral US diagnosis, GA, and history of fetal anomalies in previous pregnancies, if present. MRI studies were reviewed by two radiologists (S N S, A H-S) in this study with more than 18 years experience in neuroimaging. MR images were analyzed for their detection of NTD, determination of NTD sac contents and topography, presence of associated CNS, and non-CNS findings. The cranial level of the studied spinal NTD was assigned by scanning the fetal spine in a transverse plane. Each vertebra was sequentially examined, and the most cephalic vertebra with evidence of laminar separation was used to identify the lesion level.
The patients and their referring physicians were informed of the results of MRI. Patients counseling was done by a neurogeneticist (M S Z) of 19 years experience. The referring physicians were asked how the additional information provided by MRI changed patient counseling and case management.
Reference standards were pathology in cases that went to termination of pregnancy or a combination of postnatal MRI, surgery, and postnatal clinical examination in cases that continued pregnancy.
Retrospectively, we correlated fetal MRI findings with US and final diagnoses and analyzed MRI findings impact on diagnosis and counseling-management decision. Abnormalities seen at US and MRI and the definitive diagnoses were graded in a scale of three: a major change (a new finding unsuspected at US or a change in diagnosis of the anomaly), a minor change (a slightly different diagnosis without a change in the classification of the anomaly), and no change. Changes in case management were grouped by type of decision to a scale of 4: changed to termination of pregnancy (TOP), changed to continuation of pregnancy, different direction of the mode and/or location of delivery or perinatal care, and no change in management.
Results
All of the cases were referred for fetal MRI due to inadequacy of their US examinations. Technical difficulties in US studies included large maternal habitus and advanced gestation (n = 5), oligohydramnios (n = 4), fetal position (n = 5), fetal spinal deformity (n = 1), skull artifacts (n = 3), and maternal abdominal scars (n = 1). Referral indications for fetal MRI and MRI findings in relation to the US data are included in Table 1. In the 19 cases with sonographically suspected NTD, fetal MRI correctly ruled out US diagnosis of cephalocele in a fetus with oligohydramnios (Fig. 1) and documented NTD in the other 18 fetuses. The NTDs included in this study were posterior cephaloceles (n = 6), anterior cephaloceles (n = 2), anencephaly (n = 1), iniencephaly (n = 1), and myelomeningoceles (MMC; n = 8).
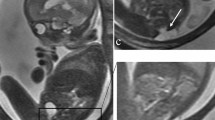
A 28-week-old fetus in utero with oligohydramnios (case 14). a A transverse 2D ultrasonography (US) shows a mass at the level of the occiput and posterior fossa (between arrowheads) and suspects the diagnosis of a posterior cephalocele. b Sagittal T2-SSFSE magnetic resonance image documents a low-positioned placenta (arrow) and rules out the US diagnosis of a cephalocele. Postnatal clinical examination revealed no abnormality
Fetal MR images were analyzed for findings concerning the NTD sac contents and topography, as well as for any associated CNS or non-CNS fetal abnormalities. Fetal MRI delineated the US findings in 11 fetuses with more clarity than US did without adding new findings. The cases included iniencephaly (Fig. 2), anencephaly (Fig. 3), frontoparietal encephalocele (case number 10), posterior cephalocele (case number 3), and seven fetuses with MMCs (cases numbers 4, 6, 11, 13, 15, 17, and 18).
A 20-week-old fetus in utero with ultrasonography diagnosis of iniencephaly (case 5). a Sagittal T2-weighted balanced fast field echo image shows well a large defect in the occiput and rachischisis of the posterior vertebral arches of the cervicodorsal spine with herniated neural tissues (black short arrow). The spinal retroflexion (white arrow) forces the fetus to look upward with the mandibular skin directly continuous with that of the chest (black long arrow). Fetal magnetic resonance imaging documented the fatal prognosis of the malformation. Labor was induced at 35 weeks of gestation, and the infant died after 1 h. b Postmortem photograph of the back of the patient confirmed the diagnosis
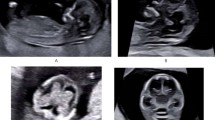
A 22-week-old fetus in uterus with impacted head in the maternal pelvis and ultrasonography (US)-suspected diagnosis of anencephaly; fetal magnetic resonance (MR) imaging confirmation was requested for medico-legal reasons (case 7). a 3D US image of the fetal face and head suspects absence of the skull vault (arrow) and relatively large orbits (arrowhead). b Sagittal T2-weighted balanced fast field echo MR image documents total absence of the skull vault and cerebral tissues (black arrow); notice the relatively large orbits (white arrow). Labor was induced at 23 weeks of gestation, and the infant died at birth. Postmortem examination documented the prenatal diagnosis
NTD sac topography and contents
Fetal MRI detected details of the NTD sac contents and topography that were US occult in five fetuses. In case number 2 (Fig. 4), with suspected posterior meningocele, fetal MRI showed herniation of bilateral occipital poles into the meningeal sac and changed the diagnosis to meningoencephalocele. In a fetus with anterior cephalocele (Fig. 5), fetal MRI documented herniation of both lateral ventricles into the sac and showed basal extension of the sac. In a fetus with marked kyphoscoliosis (Fig. 6), fetal MRI demonstrated a neural placode within the suspected spinal NTD. In two fetuses with posterior cephaloceles of sonographically undetermined contents, fetal MRI documented herniated brain tissues in one case (case number 16) and the presence of only cerebrospinal fluid (CSF) in the other (case number 19).
A 22-week-old fetus in uterus with ultrasonography (US) diagnosis of posterior meningocele versus cystic neck mass (case 2). a Sagittal T2-weighted balanced fast field echo (b-FFE) magnetic resonance (MR) image shows a large cystic mass at the occiput and posterior neck region (between arrowheads). b Axial T2-weighted b-FFE MR image of the brain shows herniation of the occipital poles (black arrow) into the sac (white arrow) and changes the US diagnosis to a posterior meningoencephalocele. Because of the poor prognosis of this malformation, labor was induced at the age of 23 weeks of gestation, and the infant died after 2 h of labor. Postnatal pathological examination confirmed the diagnosis
A 23-week-old fetus in utero with ultrasonography (US) diagnosis of anterior cephalocele (case 10). a Coronal 2D US image shows herniation of the cerebral tissue through a calvarial defect (arrows). b 3D US image of the face and frontal head region shows the sac. c Coronal T2-weighted balanced fast field echo provided more detailed topography of the swelling and its contents. The white arrowhead points to the basal extension of the sac through an anterior cranial fossa defect. The arrow points to the disorganized brain and dilated ventricles within the sac. The black arrowhead points to cerebral cortical interruption (spontaneous ventriculostomy) that was occult in US
A 30-week-old fetus in utero with marked kyphoscoliosis and ultrasonography-suspected diagnosis of myelomeningocele (case 8). a Sagittal T2-weighted balanced fast field echo (b-FFE) image of the brain shows a small posterior fossa, obliterated cisterna magna (arrowhead), and caudal displacement of the hindbrain. Magnetic resonance imaging findings are typical for Chiari-II malformation. b Sagittal T2-weighted b-FFE image of the fetal torso, documents neural placode (white arrow) herniating in a dorsolumbar meningocele (arrowheads). Notice the awkward position of the fetal head with the face turned backwards (black arrow). c Axial T2-weighted b-FFE at the level of D12 vertebra (arrow) shows a CSF-filled sac herniating through the posterior vertebral defect (white arrowhead). The neural placode within the sac exhibits myelomalacic high signal intensity (black arrowhead)
In the eight cases with the final diagnosis of MMC, prenatal determination of the cranial level of the lesion by US in comparison with the reference standard (postnatal MRI and postnatal radiographs) were in agreement in three cases, within one spinal level in four and could not be determined in one case. Prenatal determination of MMC level by MRI was in agreement with the reference standard in four cases, within one spinal level in three cases and within two spinal levels in one case.
Associated CNS findings
Hindbrain abnormalities typical for Chiari-II malformations (a small posterior fossa with caudal displacement of the vermis, brainstem, and fourth ventricle; Fig. 6) were documented by both US and MRI in the eight fetuses with US diagnosis of open MMC. In three fetuses with suspected NTDs (cases number 1, 9, and 12), MRI added CNS abnormalities that were US occult that included partial vermian hypoplasia, dysplastic brainstem, and multiple cerebral cortical interruptions (spontaneous ventriculostomies; Fig. 5).
Associated non-CNS findings
In three fetuses with Meckel–Gruber syndrome (cases number 3, 12, and 16), both US and MRI detected bilateral multicystic non-obstructive kidneys in association with posterior cephaloceles. MRI identified with more clarity than US did dilation of biliary ducts and added pulmonary hypoplasia in case number 3 (Fig. 7).
A 28-week-old fetus in utero with marked oligohydramnios and sonographically suspected diagnosis of a posterior meningocele associated with Dandy Walker malformation (DWM) and multicystic kidneys (case 3). a Sagittal T2-weighted balanced fast field echo (b-FFE) image of the head documents the presence of marked ventriculomegaly and posterior meningocele (white arrow). Elevated insertion of the tentorium cerebelli (black arrow), as well as vermian agenesis are typical for DWM. b Sagittal T2-weighted b-FFE image of the fetal body shows associated multicystic kidney (arrow) and dilated biliary ducts (arrowhead) indicating a syndromal neural tube defects (Meckel–Gruber)
No abnormalities were detected on prenatal sonography that were not apparent on fetal MRI. Table 1 includes final diagnoses based on reference standard findings, fate, and the impact of MRI findings on diagnosis and management decision.
Reference standards
Ten cases had TOP; autopsy was possible in eight. For religious reasons, parents of two fetuses (cases numbers 1 and 10) refused autopsy but allowed for external examination of the aborted fetuses. Nine cases continued pregnancy until term; six of them were delivered by cesarean section. Reference standard measures for cases that completed pregnancy were a combination of postnatal MRI (n = 7), surgery (n = 2), and postnatal clinical examination (n = 2) in the others. No disparity between the used reference standards and fetal MRI findings in any of the studied cases was noted.
Impact of fetal MRI findings on diagnosis
In correlation with the reference standard diagnosis, there was no recorded misdiagnosis on the basis of MR images. Fetal MRI detected new findings unsuspected at US that changed the US diagnosis in 3/19 cases (15.8%), detected US occult findings that caused minor change in the classification of the anomaly in 5/19 (26.3%), and did not influence the US diagnosis in the other 11/19 fetuses (57.9%; Table 1).
Impact of fetal MRI findings on counseling management
Fetal MR images were used to decide to terminate the pregnancy in two cases (cases numbers 1 and 2), with a mean GA of 20.5 weeks SD 2.12 and to continue the pregnancy of a normal fetus at 28 weeks of gestation. Fetal MRI directed the mode and location of delivery to cesarean section at term in a tertiary care hospital in a fetus with a sonographically occult large exposed neural placode in a dorsolumbar MMC (case number 8). Fetal MRI did not influence the management decision in 15 fetuses with mean GA of 26.06 weeks SD 6.1.
Discussion
While US has been the traditional mainstay of fetal imaging, its ability to resolve critical features of CNS anatomy faces many limitations [14]. Technical limitations of US studies were attributed in this study to oligohydramnios, fetal position, skull artifacts, large maternal habitus, advanced gestation, or maternal abdominal scars from previous surgery. US limitations made the diagnosis of NTD questionable. Previous reports showed the usefulness of fetal MRI in diagnosing NTD in the presence of US limitations as well as in late stages of pregnancy [6–8, 10].
In this study, fetal MRI correctly established the diagnosis of all of the cases referred with sonographically suspected findings of NTD. Fetal MRI ruled out US diagnosis of cephalocele in a fetus with oligohydramnios and confirmed the presence of NTDs in the other 18 cases.
The key for successful fetal MRI is tailoring the study according to the referral data by an attending experienced radiologist using the proper sequences [15, 16]. The brain structures and the entire length of the fetal spine could be studied in multiple planes on MRI, which is important to document possible cranial or spinal presentation of NTDs [7, 9, 17]. In this study, fetal MRI correctly diagnosed nine fetuses with cranial NTDs (posterior cephaloceles, anterior cephaloceles, and anencephaly) as well as nine fetuses with spinal NTDs with MMC and iniencephaly.
Cephalocele in general means herniation of brain matter through a defect in skull [4]. In the USA, approximately 80% of lesions are found near the occipital bone. In contradistinction, many cephaloceles in some countries in Asia as well as in Egypt involves the frontal bone [2]. In our study, two out of the eight fetuses with cephaloceles were anteriorly located. The prognosis of cephaloceles varies based upon the size, location, involvement of neural structures, and the presence of any associated syndromes [4]. In this study, fetal MRI correctly documented varying amounts of brain tissues and CSF within the studied cephaloceles. Fetal MRI detected too the details of the contents and topography of five out of the 18 NTD sacs that were sonographically occult.
MMC is identified by the absence of posterior elements of the vertebral bodies at affected levels and extension of the subarachnoid space and neural tissues posteriorly through the bony spinal defect [18–20].
Leg movement in fetuses with MMC has been observed in prenatal imaging as early as 16 to 17 weeks of gestation [21]. In contrast, most MMC fetuses exhibit severe neurologic impairment of the lower extremities by the time of birth, suggesting that the neurologic injury may occur later in gestation due to exposure to the intrauterine environment [22].
Although surgical closure of MMC is usually performed in the early postnatal period, intrauterine repair was performed in a few specialized centers worldwide [23]. The rationale for prenatal correction of MMC is to repair the defect before neurologic damage has occurred or when there is still potential for recovery [24]. A fetus with MMC is considered for surgery if the GA at the time of the proposed surgery was 26 weeks or less, if the transatrial cerebral ventricular diameter was less than 16 mm (normal <10 mm), if the estimated level of the lesion was S1 or above, and if there was convincing leg and foot motion in the absence of foot or leg deformity [24, 25].
As interest in fetal surgery for open spinal NTDs has increased, so has the need for more detailed information from imaging of the fetal brain and spine [24–26]. Fetal MRI is considered imperative to document the criteria of selection of in utero repair of MMC and to exclude skin-covered dysraphic lesions such as lipomyelomeningocele or myelocystocele [25, 26]. A thick-walled sac, absence of hindbrain hernia, and lack of elevation of maternal or amniotic fluid AFP should raise suspicion of an occult dysraphism such as lipomyelomeningocele or myelocystocele [26].
In this study, fetal MRI correctly diagnosed eight fetuses with MMC. Accurate determination of MMC lesion level is critical to the proper counseling of prospective parents of an affected fetus. Lesion level is correlated with both leg functions and shunt-dependent hydrocephalus [18]. Recent studies found that lesion level is an important determinant of outcome after intrauterine MMC repair. For prenatal counseling, especially if intrauterine MMC repair is an option, an error of plus or minus two levels could substantially affect a prospective parent’s decision to terminate a pregnancy or choose between intrauterine and conventional therapy [19]. In this study, prenatal imaging (US and MRI) determined the cranial level of MMC within one level of the reference standard in seven out of the eight cases with MMC (87.5%); the results are in concordance with a previous study [20]. Although, improved neurologic function from repair of MMC in utero was reported [27], definite expectations for improved neurological outcome have not been yet fulfilled as not all patients benefited from fetal surgery in the same way [25].
MMCs are almost always seen in combination with a small posterior fossa and herniation of cerebellar tissue into the cervical subarachnoid space (referred to as the Chiari-II malformation). In general, Chiari-II malformations and MMC can be easily diagnosed on prenatal ultrasound [2]. However, previous studies showed that fetal MR imaging can be a helpful adjunct when sonography analysis is limited by large maternal body habitus, oligohydramnios, or low position of the fetal head [8, 9, 11]. In this study, Chiari-II malformations were documented by both US and MRI in all the eight fetuses with MMCs.
It has been reported that almost all neonates with thoracolumbar MMC require ventriculoperitoneal shunting for hydrocephalus [26]. However, following fetal surgery for MMC, preliminary findings suggested a reduced incidence of shunt-dependent hydrocephalus as well as an improved hindbrain herniation. Serial fetal MRI was used to document the improvement in hindbrain herniation following in utero surgery for MMC [27, 28].
Fetal MRI has been reported to be useful in identifying additional CNS anomalies that could be associated with NTDs such as hindbrain malformations, corpus callosal dysgenesis, and cerebral parenchymal abnormalities [2, 8, 19]. In three out of the 18 fetuses with NTDs in this study, MRI added CNS abnormalities (dysplastic brainstem, Dandy Walker malformation continuum, and cerebral cortical interruptions) that were not apparent on US. Previous reports showed that prenatal US was occasionally unable to visualize the brainstem and other posterior fossa structures [29, 30]. Conversely, fetal MR can display the posterior fossa more clearly especially on midline sagittal image [9]. Parenchymal abnormalities in association with NTDs frequently cannot be visualized by US [2]. In this study, multiple cortical cerebral interruptions (porencephalies due to spontaneous ventriculostomies in case number 9) were occult on US and were only detected by prenatal MRI.
NTD could be part of a recognized syndrome with associated non-CNS findings [2]. In three out of six fetuses with posterior cephaloceles in this study, prenatal imaging detected associated renal abnormalities and suggested the diagnosis of Meckel–Gruber syndrome; fetal MRI documented with more clarity hepatic biliary dilatation in one of these fetuses.
Anencephaly is the most severe form of NTDs that refers to an extensive defect in the craniovertebral bone which causes the brain to be exposed to amniotic fluid. The incidence of anencephaly is highest in Egypt among other countries such as Ireland, Scotland, and New Zealand [2, 4]. In one of our cases with impacted head in the maternal pelvis, fetal MRI documented the US diagnosis of anencephaly that was needed for medico-legal reasons.
Iniencephaly is a rare type of spinal NTD characterized by a variable deficit of the occipital bones, malformed cervicothoracic spine, and an upward-turned face with the mandibular skin directly continuous with that of the chest [2]. Although the diagnosis of iniencephaly is easy to make on ultrasound due to the typical stargazing fetus, the details of the fetal brain and spinal cord may not be adequately delineated [31]. There are few reports of MRI diagnosis in utero of cases with iniencephaly [31, 32]. In these reported cases, as well as in our case, fetal MR delineated the intracranial and intraspinal anomalies to a much greater extent than US did [33, 34].
Although fetal MRI detected new findings unsuspected at US in 8/19 (42.1%) fetuses, the new findings changed the prenatal diagnosis in only three (15.8%); the additional findings detected by MRI in the other five fetuses did not change the main diagnosis of the anomaly.
The results of fetal MR imaging in this study, whether verifying absence of abnormality, confirming sonographically detected abnormalities, or discovering additional abnormalities that were not apparent by sonography, have been shown to affect clinical decision-making during pregnancy, both by physicians and parents. The degree of confidence required for prenatal diagnosis is clearly higher in cases where TOP is considered [8].
Fetal MRI ruled out the US diagnosis of a cephalocele and changed the management decision to continue the pregnancy. While in two fetuses (cases number 1 and 2), fetal MRI detected additional findings that worsened the prognosis and were used to decide to terminate the pregnancy. The superior resolution provided by MRI allowed the delineation of hindbrain abnormalities in association with posterior cephalocele that worsened the prognosis (case number 1). A fetus with diagnosed hindbrain malformation (brainstem and/or vermian dysplasia) usually has a poor neurodevelopmental outcome [9, 10]. Fetal MRI identified brain tissue herniation in a sonographically suspected posterior neck mass in case number 2 that led to the diagnosis of cephalocele. Previous studies showed that a fetus with a meningocele (without brain tissue) may have a normal outcome; whereas, in cases with brain tissue presents within the defect, the mortality rate is as high as 71% [2]. However, decision-making during pregnancy is multifactorial. Parent’s decision to terminate or continue pregnancy depends on the GA among other factors [1]. Cases who continued pregnancy had a higher GA (26.06 weeks SD 6.1). Other factors that influence decision-making during pregnancy are the severity and type of the fetal abnormality, presence of associated syndromes, and social or religious views [1, 10]. Fetal MRI can provide incremental information that may directly affect the mode and location of delivery of fetuses with NTDs or may help supplement or confirm indeterminate or equivocal US findings [9, 10, 26]. In our study, fetal MRI directed the mode and location of delivery to cesarean section at term in a tertiary care hospital in a fetus with a sonographically occult large exposed neural placode herniating in a MMC. In the other examined fetuses, fetal MRI provided a measure of confidence in their management decision.
This study has few limitations such as the relatively small sample size of 19 cases, which reflect the strict patient selection to only those with US technical difficulties or questionable US findings. The fact that pathological verification of MRI diagnosis was not possible in all of the studied cases is another limitation commonly encountered in many fetal imaging studies; for religious and emotional reasons, the parents often refuse autopsy for their offsprings. This study included an overall evaluation of the role of fetal MRI in a wide range of cranial and spinal presentations of NTDs. However, further studies are needed to evaluate the diagnostic ability and accuracy of in utero MR imaging of the different presentations of NTDs in specific.
Conclusion
Fetal MRI findings have important implications for clinicians and radiologists who may have difficulty reaching a diagnosis and critical management decisions in cases with sonographically suspected NTDs. Fetal MRI can identify additional findings that are sonographically occult and can influence management decision of NTD.
References
De Marco P, Merello E, Mascelli S et al (2006) Current perspectives on the genetic causes of neural tube defects. Neurogenetics 7(4):201–221
McGahan JP, Pilu G, Nyberg D (2003) Neural tube defects and the spine. In: Nyberg D, McGahan J, Pretorius D, Pilu G (eds) Diagnostic imaging of fetal anomalies. Lippincott Williams & Wilkins, Philadelphia, pp 291–334
Birnbacher R, Messerschmidt AM, Pollak AP (2002) Diagnosis and prevention of neural tube defects. Curr Opin Urol 12(6):461–464
Shurtleff DB, Lemire R (1995) Epidemiology, etiologic factors, and prenatal diagnosis of open spinal dysraphism. Neurosurg Clin N Am 6(2):183–193
Steinbok P, Irvine B, Cochrane DD et al (1992) Long-term outcome and complications of children born with meningomyelocele. Childs Nerv Syst 8(2):92–96
Hubbard AM, Simon EM (2002) Fetal imaging. Magn Reson Imaging Clin N Am 10:389–408
Simon EM, Goldstein RB, Coakley FV et al (2000) Fast MR imaging of fetal CNS anomalies in utero. AJNR Am J Neuroradiol 21:1688–1698
Turgut F, Turgut M, Onur E et al (2001) In utero MR imaging and management of foetal hydrocephalus and NTDs in the third trimester. J Neurosurg Sci 45(3):189–192
Glenn OA, Barkovich AJ (2006) Magnetic resonance imaging of the fetal brain and spine: an increasingly important tool in prenatal diagnosis, part 2. AJNR Am J Neuroradiol 27:1807–1814
Griffiths PD, Widjaja E, Paley MN et al (2006) Imaging the fetal spine using in utero MR: diagnostic accuracy and impact on management. Pediatr Radiol 36(9):927–933
von Koch CS, Glenn OA, Goldstein RB et al (2005) Fetal magnetic resonance imaging enhances detection of spinal cord anomalies in patients with sonographically detected bony anomalies of the spine. J Ultrasound Med 24:781–789
Rossi A, Cama A, Piatelli G et al (2004) Spinal dysraphism: MR imaging rationale. J Neuroradiol 31(1):3–24
Kolble N, Huisman TA, Stallmach T et al (2001) Prenatal diagnosis of a fetus with lumbar myelocystocele. Ultrasound Obstet Gynecol 18:536–539
Mangels KJ, Tulipan N, Tsao LY et al (2000) Fetal MRI in the evaluation of intrauterine myelomeningocele. Pediatr Neurosurg 32(3):124–131
Haacke EM, Wielopolski PA, Tkach JA et al (1990) Steady-state free precession imaging in the presence of motion: application for improved visualization of the cerebrospinal fluid. Radiology 175(2):545–552
Chung HW, Chen CY, Zimmerman RA, Lee KW, Lee CC, Chin SC (2000) T2-Weighted fast MR imaging with true FISP versus HASTE: comparative efficacy in the evaluation of normal fetal brain maturation. AJR Am J Roentgenol 175(5):1375–1380
Guibaud L (2004) Practical approach to prenatal posterior fossa abnormalities using MRI. Pediatr Radiol 34:700–711
Coniglio SJ, Anderson SM, Ferguson JE (1996) Functional motor outcome in children with myelomeningocele: correlation with anatomic level on prenatal ultrasound. Dev Med Child Neurol 38:675–680
Aaronson OS, Hernanz-Schulman M, Bruner JP (2003) Myelomeningocele: prenatal evaluation—comparison between transabdominal US and MR imaging. Radiology 227:839–843
Kollias SS, Goldstein RB, Cogen PH, Filly RA (1992) Prenatally detected myelomeningoceles: onographic accuracy in estimation of the spinal level. Radiology 185:109–112
Korenromp MJ, van Gool JD, Bruinese HW, Kriek R (1986) Early fetal leg movements in myelomeningocele. Lancet 1(8486):917–918
Correia-Pinto J, Reis J, Hutchins G, Baptista MJ, Estevao-Costa J, Flake AW, Leite-Moreira AF (2002) In utero meconium exposure increases spinal cord necrosis in a rat model of myelomeningocele. J Pediatr Surg 37:488–492
Sutton LN (2008) Fetal surgery for neural tube defects. Best Pract Res Clin Obstet Gynaecol 22(1):175–188
Rintoul NE, Sutton LN, Hubbard AM, Cohen B, Melchionni J, Pasquariello PS, Adzick NS (2003) A new look at myelomenigoceles: functional level, vertebral level, shunting, and the implications for fetal intervention. Pediatrics 109:409–413
Fichter MA, Dornseifer U, Henke J, Schneider KTM, Kovacs L, Biemer E, Bruner J, Adzick NS, Harrison MR, Papadopulos NA (2008) Fetal spina bifida repair—current trends and prospects of intrauterine neurosurgery. Fetal Diagn Ther 23:271–286
Leung EC, Sgouros S, Williams S, Johnson K (2002) Spinal lipoma misinterpreted as a meningomyelocele on antenatal MRI scan in a baby girl. Childs Nerv Syst 18(6–7):361–363
Adzick NS, Walsh DS (2003) Myelomeningoclele: prenatal diagnosis, pathophysiology and management. Semin Pediatr Surg 12(3):168–174
Bouchard S, Davey MG, Rintoul NE, Walsh DS, Rorke LB, Adzick NS (2003) Correction of hindbrain herniation and anatomy of the vermis after in utero repair of myelomeningocele in sheep. J Pediatr Surg 38(3):451–458
D’Addario V, Pinto V, Di Cagno L et al (2005) The midsagittal view of the fetal brain: a useful landmark in recognizing the cause of fetal cerebral ventriculomegaly. J Perinat Med 33:423–427
Pilu G, Segata M, Ghi T et al (2006) Diagnosis of midline anomalies of the fetal brain with the three-dimensional median view. Ultrasound Obstet Gynecol 27:522–529
Chen CP (2007) Prenatal diagnosis of iniencephaly. Taiwan J Obstet Gynecol 46(3):199–208
Pungavkar SA, Sainani N, Karnik AS et al (2007) Antenatal diagnosis of iniencephaly: sonographic and MR correlation: a case report. Korean J Radiol 8(4):351–355
Simon EM, Pollock AN (2004) Prenatal and postnatal imaging of spinal dysraphism. Semin Roentgenol 39(2):182–196
Coakley FV, Hricak H, Filly RA et al (1999) Complex fetal disorders: effect of MR imaging on management-preliminary clinical experience. Radiology 213:691–696
Acknowledgment
The authors thank Miss Amal Mahmoud, the MRI technician.
Conflict of interest statement
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Saleem, S.N., Said, AH., Abdel-Raouf, M. et al. Fetal MRI in the evaluation of fetuses referred for sonographically suspected neural tube defects (NTDs): impact on diagnosis and management decision. Neuroradiology 51, 761–772 (2009). https://doi.org/10.1007/s00234-009-0549-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-009-0549-0