Abstract
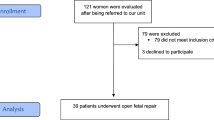
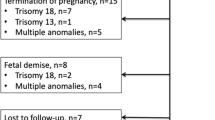
The management of myelomeningocele study trial showed significant prognostic improvement in fetal repair before 26 weeks of gestation. Hence, surgery in utero represents the best treatment option for open-neural tube defects (NTDs). Fetal surgery of open-NTDs has specific inclusion and exclusion criteria, which can be adequately studied with fetal MRI. The main concern: the spine (spinal defects other than Myelomeningocele and Myeloschisis, the level of the lesion higher than T1 or lower than S1 and the degree of kyphosis ≥ 30°), the skull/brain (no cerebellum herniation and Chiari II malformation and the presence of any intracranial abnormality unrelated to open NTDs), the uterus (cervix length less than 2 cm, multiple gestations and placental and uterine abnormalities) and any other fetal abnormality not attributed to spinal defect. In this review, we describe the fundamental role of fetal MRI in supporting therapeutic decisions in pre-surgery intrauterine planning through the accurate and comprehensive description of findings, providing a proposal of a structured report. In addition, we describe how post-surgical MRI is important in investigating the effectiveness of surgery and detecting repairing complications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Myelomeningocele (MMC)
Myelomeningocele (MMC) represents the most frequent neural tube defects (NTDs), affecting nearly 1500 newborns in the USA annually and 0.2–6.5 newborns from every 1000 births globally [1,2,3,4], despite considerable advances having been made in disease prevention by periconceptional folic acid supplementation.
The open-NTDs, which result from failure of primary neurulation [5], are characterised by protrusion of the meninges and spinal cord through a midline fusion defect of the caudal neural tube, without an intact skin lining, forming either a sac containing cerebrospinal fluid (MMC) or a flat lesion (Myeloschisis or Myeloceles) with malformed and dysplastic neural tissue in the middle. Most MMCs occur in the lumbar region, though they can occur anywhere along the spine. They are described as “segmental” when the spinal cord continues distally beyond the dysraphism level and as “terminal” when the placode occurs at the end of the spinal cord [6].
Depending on the lesion level, individuals born with MMC have variable degrees of lower-extremity paraplegia, skeletal deformities, bowel and bladder incontinence, hindbrain herniation, hydrocephalus, and neurocognitive impairments [7].
It is hypothesised that cerebrospinal fluid (CSF) leakage can cause intracranial hypotension and result in a Chiari malformation Type II [8], present in almost every fetus with MMC. In most cases, it is characterised by a small posterior cranial fossa with a hindbrain herniation (HBH).
The HBH seen in this malformation is caused by a downward displacement of the cerebellum below the level of the foramen magnum and may result in a compressed brainstem and obstructed fourth ventricle. This last can slow down the flow of the CSF until it is blocked and result in hydrocephalus [8,9,10].
“Two-hit hypothesis” and surgery techniques
The management of myelomeningocele study (MOMS) Trial proved that fetal surgery performed before 26 weeks of gestation significantly improved the prognosis [11]. In-utero repair surgery is the best treatment option for open-NTDs.
However, its application is limited to a few specialised centres, mainly in high-income countries.
The incomplete closure of the neural tube and the subsequent agenesia of the overlying neural arches and skin leave the neural placode exposed to mechanical trauma from the uterine wall and chemical trauma from the amniotic fluid. This damage represents the second step of the “two-hit hypothesis” [12]: it assumes that the functionally normal but dysraphic exposed (first “hit”) spinal cord is progressively damaged during intrauterine life by trauma and toxic effect of the amniotic fluid (second “hit”). A significant neuronal loss has already been demonstrated before 16 weeks of gestational age; the injury extends cranially with a significant functional reduction in motor neurons of the adjacent cord above the defect, which worsens at a rate of 16% per week of gestational age [13].
The improved outcomes resulting from intrauterine repair confirm that spinal cord injury is progressive during pregnancy [13]. Prenatal in-utero surgical closure of MMC aims to protect the neural placode from the intrauterine environment and stop CSF leakage, and, as the MOMS trial showed, it reduces hindbrain herniation, hydrocephalus and improves motor outcomes at 30 months [14] (in particular, this last aspect is assumed to derive from the prevention of the cranial extension of damage [13]).
Different approaches are possible for uterine MMC repair: open, fetoscopic, and hybrid. As regards the comparison between fetoscopic repair and open fetal surgery, some independent studies and metanalyses have described a lower risk of uterine dehiscence, premature rupture of membranes, placental abruption and chorioamnionitis and improved rates of mortality, prematurity, shunt placement and motor and mental development in fetoscopic repair[15,16,17,18,19,20,21,22,23].
However, not enough data are available to determine the best surgical approach and the choice of technique should also be considered in the cost-effectiveness analysis, that in a recent study demonstrated that the fetoscopic approach for MMC repair was cost-effective compared with the open approach: despite the procedure itself has a higher cost, there are improved long-term outcomes from the maternal and neonatal perspective[24].
Diagnosis and studies for surgery
Prenatal diagnosis of spina bifida is usually made by measurement of alpha fetal protein (AFP) in the maternal serum at 16 weeks of gestation or by ultrasound of the fetus at 18–24 weeks of pregnancy through the identification of direct (bone defect and sac protrusion) and indirect signs (smaller biparietal diameter, “lemon sign”, ventriculomegaly, obliteration of the cisterna magna and cerebellar abnormalities, like the downward displacement through the foramen magnum, small cerebellum or anterior concave shape—“banana sign”-) [25]. In addition, there is recent evidence of possible diagnostic anticipation by ultrasound at 11–14 weeks of gestation, mainly by indirect signs detection (abnormalities of the posterior fossa such as reduced or absent intracranial translucency [25, 26] or cisterna magna [27] or an abnormal relationship between the brainstem and the distance between the brainstem and the occipital—“crash sign”- [28]).
In case of suspicion of open-NTDs in the fetal period, it is necessary to complete the diagnostic process to achieve a confident diagnosis. Identifying the inclusion and exclusion criteria for fetal surgery is also required to obtain the most appropriate perinatal management.
The following steps in the workup and selection of candidates for fetal surgery are:
-
Amniocentesis: for studying AFP and acetylcholinesterase in amniotic fluid to confirm open-NTDs and for genetic study to detect chromosomal abnormalities and other known genetic alterations. The inclusion criteria of all fetal surgery programs mention at least a standard karyotyping or quantitative fluorescence polymerase chain reaction (QF-PCR); some centres also request a standard microarray analysis [29].
-
Imaging studies: partly carried out through morphology ultrasound which can determine the anatomical (the highest level of the bone defect) and functional (assessment of hip, knee and ankle/foot mobility [30]) level, the associated malformation, the presence of kyphosis or ventriculomegaly and the cervix length. A fetal MRI study is required in all candidates for fetal surgery to have an accurate and comprehensive study of NTDs and other imaging criteria for fetal surgery. Furthermore, MRI may provide crucial additional prognostic information for parents deciding whether to proceed with intrauterine MMC repair or terminate the pregnancy.
Fetal MRI protocol
Usually, the fetal MRI is performed with 1.5 or 3 T machines with a phased array surface coil without contrast or sedation. Hypoglycemia can be induced by performing the fetal MRI after fasting for at least four hours to reduce fetal motility. Furthermore, execution of the US immediately before the fetal MRI can induce fetal sleep. The supine position is the most commonly used, but lateral positions can also be considered if it is not well tolerated [31, 32]. First, the “localiser sequence” is acquired; it is usually represented by 6 mm slices coronal T2-weighted single-shot fast turbo spin-echo to identify fetal presentation (fetal position to the mother’s one) and to study uterine walls and placenta. Later, the images of each series performed are used as a reference for subsequent sequences to minimise the orientation problems related to fetal motility. The total examination time is around 20–30 min, according to the number of sequences to be repeated due to fetal movement artefacts and according to the additional sequences performed to clarify any findings identified that might require it.
In the context of open-NTDs, the fetal MRI protocol should be composed in the first part by sequences useful for properly studying the spine and the brain and then by sequences focused on the remaining anatomical fetal areas. Subsequent sequences of the fetal MRI study can be divided into mandatory and optional sequences (Table 1) [31,32,33]:
-
Mandatory sequences:
-
o
T2-weighted fast or turbo spin-echo (HASTE, SSFSE or SSTE)[34] with axial, sagittal and coronal orientation orthogonal to the area of interest. These sequences allow an accurate representation of fetal anatomy. In addition, we can consider the possibility of obtaining fast or turbo spin echo sequences with different echo times (TE) and different FOV sizes for better image quality in different districts: for example, long TE and small FOV in imaging of the fetal brain and shorter TE on the abdomen to have more contrast [32, 35].
-
p
T2-weighted steady-state free-precession (SSFP), that represents a potentially three-dimensional sequence (thanks to 1.6-mm thick contiguous slices); however, the quality reduction in reconstructed images on different planes leads to prefer acquisition of T2w-SSFP with different acquisition orientation. These sequences also accurately represent vessels [32, 35].
-
q
T1-weighted gradient echo (GRE), to identify methemoglobin in subacute haemorrhage and calcification [32, 36] to better delineate bone structure also T2*-weighted “Black-Bone” images have been proposed.
-
r
Single-shot high-resolution (SSH) GRE echoplanar (EP) sequences, which allow to evaluate bony structures, calcification and products of blood degradation, such as deoxyhemoglobin, which suggests a recent bleed, or hemosiderin, which represents an older haemorrhage [32, 37].
-
s
Diffusion-weighted imaging (DWI) with reconstruction of the apparent diffusion coefficient (ADC) maps, to detect hypoxic-ischemic brain lesions [32, 38].
-
o
-
Optional sequences: single-shot fluid attenuated inversion recovery (FLAIR) and inversion-recovery-prepared single-shot fast spin-echo T1-weighted sequence (SNAPIR).
Instead, to evaluate the remaining fetal regions to detect any abnormalities not associated with the spinal defect, which could exclude the fetus from the in-utero repair program, we carry out sequences T2-weighted fast or turbo spin-echo (HASTE, SSFSE or SSTE) in two planes, usually axial and coronal on the fetus. In addition, we add to the protocol sequences such as T1-weighted gradient echo (GRE), diffusion-weighted imaging and SSH magnetic resonance cholangiopancreatography sequences to clarify any findings of uncertain significance.
Imaging criteria for fetal surgery of open-NTDs
The typical inclusion and exclusion criteria for fetal surgery of open-NTDs derive from the MOMS trial (Table 2) [14]. These criteria are not applied strictly in today’s clinical practice, such as BMI (usually increased to 40) and gestational age (up to 27–28 weeks) [29, 39].
Within the criteria of inclusion and exclusion for uterine surgery of open-NTDs, there are some fundamental imaging criteria, which may be included in the following imaging exclusion criteria [40]:
Spine:
types of lesions other than MMC or Myeloschisis;
Upper level of defect higher than T1 or lower than S1;
Kyphosis ≥ 30°.
Brain:
Absent hindbrain herniation or Chiari II malformation;
Intracranial anomaly not explained by open spinal dysraphism.
Any fetal anomaly not explained by open spinal dysraphism.
Uterus:
Cervix < 2 cm in length;
Multiple gestations;
Placental abnormalities (placenta previa, placenta accrete, placental abruption, suspected adhesion disorders);
Uterine abnormalities (e.g., bicornate uterus, large or multiple leiomyomata).
These imaging criteria can be evaluated with both US and MRI methods, although MRI is better assessed, ensuring higher standardisation.
What to see in fetal MRI performed for MMC
Spine
NTDs are represented by a varied and numerous group of alterations whose differential diagnosis requires an accurate and systematic analysis of MRI images, enabling the identification of vertebral anomalies, spinal cord and spinal canal anomalies (like Tethered cord syndrome, Split cord syndrome and Syrinx), linear tethering tracts anomalies (like dorsal dermal sinus, limited dorsal myeloschichis, meningocele manquè), dysraphic mass lesions (divided in fluid-containing lesions, fluid with soft tissue, fat-containing masses) and caudal cell mass [41]. In particular, as regards dysraphic mass lesions there are several subgroups and their distinction is possible only through a systematic study of their content, extent, components that exceed the vertebral and dural defect and the interface between intratumoral fat and subcutaneous fat and neural placode [41]:
Fluid-containing lesions:
Meningocele characterised by dorsal herniation of cerebrospinal fluid containing a meningeal sac through vertebral defect;
Intradural extramedullary cyst divided into epidermoid cyst, arachnoid cyst, filar cyst or neurenteric cyst;
Intraspinal enterogenous cysts;
Ependymal cyst or persistent fifth ventricle.
Fluid with soft tissue (neural elements):
MMC, characterised by herniation of the fluid-filled sac with neural elements;
Terminal myelocystocele characterised by conus and neural placode with dilated central canal in the protruded sac.
Fat-containing masses:
Intradural lipoma: lipid-containing masses encapsulated within the intact dural coating;
Lipomyeloceles/lipomyelomeningocele: lipid-containing masses traversed dural and vertebral defects and extended into subcutaneous tissues; in particular, the intratumoral fat is diffusely or focally continuous with the subcutaneous fat;
Lipomas of caudal cell mass;
Teratoma: cystic, solid, unilocular, or multilocular lesions with fat, calcification, bony, and other mesenchymal elements; in particular the intratumoral fat has no communication with subcutaneous fat.
The spinal defects eligible for fetal surgery are the MMC and the Myeloschisis (also known as Myelocele). They are characterised by the presence of a bone and skin defect with, in MMC, a protrusion of the neural placode beyond the skin surface due to enlargement of the adjacent subarachnoid space (Fig. 1), while in Myelocele the placode is at the level of the skin surface [41]. Most of the open-NTDs are MMC (98.8%). This difference is crucial from a surgical perspective because skin closure can be technically more challenging for a myeloschisis and graft closure is often necessary [42]. Open-NTDs are usually located in the lower lumbar and sacral regions (98%); they are rare in the cervical and upper thoracic spine, probably because the lesions in these areas are more severe and may not allow the survival of the fetus [43]. In cases where it is difficult to determine whether it is an open or closed spinal defect, especially in defects partially covered by skin, acetylcholinesterase can be researched in amniotic fluid as it indicates CSF leak.
Another fundamental characteristic of the eligibility for surgery is the lesion level, which must not be higher than the T1 vertebral body level or lower than S1.
The defect level can be determined both through US and MRI: the US allows better determination of bone structures with the limits of an operator-dependent modality [44]; instead, MRI does not have the limits of the operator dependent and allows a comprehensive study of the spinal defect. Nevertheless, an inaccuracy of about 20% in determining the lesion’s level has been observed with both methods [45]. To overcome this limit the use of T2*-weighted “Black-Bone” images have been proposed, as they may better delineate bone structures. In addition, other studies have shown an exact level match between fetal and postnatal MRI of 42.9% and within 1 level of concordance in 82% (98/119) of patients. These mistakes are partially related to the tiny size of the fetus, with reference points close to the millimetre, and partially related to the inadequate resolution of the discal spaces and vertebral bodies in the fetal MRI of the entire spine [46]. Further, there are normal anatomic variations in vertebral body, such as the presence of 6 lumbar vertebral bodies, which may make the vertebral count difficult. The level of the spinal dysraphic defect is determined in relation to the lumbosacral junction, using the following reference points: the most caudal spinal hyperintense disc space as L5–S1 and the lowest horizontal vertebral body as L5. In this way, it is possible to identify the vertebral body superior to the highest level of the absence of the posterior elements at the bone/skin defect [46].
An adequate characterisation of the spinal lesion also includes the measurement of the defect’s size: anterior–posterior and craniocaudal dimensions show a positive correlation with the lateral and third ventricular size in the fetus [47] and, from a surgical point of view, larger defects are more challenging to close [48]). In the case of MMC, the sac’s size should be described because inversely related to the degree of hindbrain herniation and might be protective against CSF leakage [47].
Kyphosis ≥ 30° is another imaging exclusion criterion. It can be measured either on fetal MRI or US and is represented by the difference by 180° and the angle composed of the two portions of the scoliotic spine (Fig. 2).
Any additional congenital vertebral defects should be described to complete the spine's characterisation. They include anomalies of vertebral formation (hemivertebrae, anteriorly wedged, and butterfly vertebrae), segmentation (block vertebra, unilateral unsegmented bars, lumbosacral transitional vertebra and additional vertebra) and a combination of both [41, 49]. They are described as simple (1–2 vertebrae) or complex (> 2 vertebrae).
Hemimyelomeningocele and hemimyelocele are rare conditions characterised by an open-NTDs in association with a split cord malformation; they result from the primary neurulation defect of one hemicord, while the other hemicord is normal or tethered [50,51,52]. Split cord malformations can be divided into two types according to Pang’s classification [53]: type I consists of two hemicords, each contained within its dural tube and separated by a rigid osseocartilaginous median septum sheathed in dura; type II, formed by two hemicords housed in a single dural tube separated by a nonrigid, fibrous median septum. Despite the potential clinical value of this condition, it is not always easy to detect in the fetal MRI, especially in the case of type II. However, Pang’s classification type I or II does not exclude fetal surgery [46].
Lastly, hydromyelia can occasionally be depicted in association with MMC; these findings are characterised by fluid-filled space in the central canal [54]. Syringomyelia, characterised by fluid-filled space in the spinal cord parenchyma, is rarely visible in the fetal period but can develop later [54, 55]. From the pathological point of view, their causes are not entirely clear and various participant phenomena have been described, including altered CSF flow dynamics. Its presence in pre-surgery time does not exclude the patient from fetal repair but must be promptly depicted if it appears after fetal surgery [56].
Fetal brain
Indirect signs of open-NTDs and other intracranial anomalies associated with open-NTDs can be identified on fetal MRI (Fig. 3). They include abnormalities of:
-
Skull: concave shape of frontal bones -“lemon sign”- and a small posterior fossa;
-
Cerebellum and hindbrain: small cerebellum or anterior concave shape -“banana sign”- and hindbrain herniation through the foramen magnum (Chiari II malformation).
-
Liquoral system: obliteration of the cisterna magna and the fourth ventricle, ventriculomegaly, transependymal oedema and loss of the subarachnoid space in the convexity;
-
Other parenchymal abnormality: agenesis/dysgenesis of the corpus callosum, abnormal ventricular wall and heterotopia, defects in cortical thickness and the gyration pattern in frontal and temporal lobes and hippocampus [57,58,59]; in some cases, this assessment is made particularly difficult by the compression of such structures as a consequence of hydrocephalus.
T2 SSFSE images of the fetal brain performed at 24 gestational weeks show intracranial anomalies. Axial view (a) shows the concave shape of frontal bones called the “lemon sign” (arrows). Sagittal view (b) shows small posterior fossa and hindbrain herniation through the foramen magnum with the obliteration of the cisterna magna and the fourth ventricle. Coronal view at the level of the choroid plexus’ glomus (c) shows hydrocephalus measurement through lateral ventricular size (line)
The concept of a “third hit”, consisting of brain injuries caused by secondary alteration due to open-NTDs, has been introduced in the background of brain anomalies. Still, the relationship between these findings and their postnatal outcomes is not entirely clear and further studies about this association are required [59].
The main characteristics of the posterior cranial fossa are represented by two quantitative parameters that must be compared with reference for gestational age [60]:
-
o
Clivus-supraoccipital angle (CSA): measured using a line connecting the most cranial part of the clivus and the basion and a line along the superior surface of the supraoccipital, cutting the opisthion;
-
p
Maximum transverse diameter of the posterior fossa (TDPF): measured at the tentorium’s insertion level with a line between the lateral borders of the posterior cranial fossa.
The degree of Chiari II malformation and hindbrain herniation is represented by a scale derived from a modified version of a grading system initially described by Sutton et al. in 1999 [61, 62]:
-
Grade 1: normal or a downward sloping tentorium and a normal patent fourth ventricle and cisterna magna without cerebellar ectopia;
-
Grade 2: cerebellar ectopia with effacement of the fourth ventricle but a patent cisterna magna;
-
Grade 3: cerebellar ectopia and effacement of the cisterna magna and fourth ventricle.
Both Grade 2 and Grade 3 fetuses are potential candidates by the MOMS inclusion criteria; hindbrain herniation is necessary and only 8% of patients with open-NTDs have not [62].
Hydrocephalus is another element known to be studied in cerebral fetal MRI. The size of the lateral ventricles quantifies it. As suggested by fetal sonography guidelines, lateral ventricular size is measured in transverse dimensions in the axial plane at the level of the frontal horns or in the coronal plane at the level of the glomus of the choroid plexus. The reference values are: normal up to 10 mm; mild-moderate ventriculomegaly at 10–15 mm; severe ventriculomegaly > 15 mm [62, 63]. Several studies have been carried out without consensus regarding the size of the ventricles as a prognostic factor. A secondary analysis of the entire MOMS cohort found that in the case of severe ventriculomegaly (> 15 mm), there is no reduction in the need for ventriculoperitoneal shunting (VPS) after fetal MMC repair [64]. Consequently, fetal MMC repair should not be offered in these situations. However, another study shows that, despite the persistence of ventriculomegaly after surgery, the modification in postoperative CSF hydrodynamics may decrease the rate of ventricular dilatation and potentially improve the degree of cerebellar herniation, suggesting a delay in the need for VPS in fetal repaired cases when compared with unrepaired cases [65]. In addition, although there is no reduction in VPS in fetuses undergoing surgical repair with severe ventriculomegaly > 15 mm, the benefits of motor function may be maintained [64, 66], so the size of ventricles is not mentioned in the exclusion criteria but are a prognostic factor able to give us information on the subsequent need for VPS.
Lastly, it is necessary to ascertain the absence of anomalies not explained by open spinal dysraphism in the brain study.
Fetal anomaly not explained by open-NTDs
Fetal anomalies unrelated to the open-NTDs are still discussed as an exclusion criterion for fetal surgery [67]. For example, the absence of high signal intensity on T1-WI of rectal meconium signal cannot represent a coexistent anal malformation. This finding can be related to the neurogenic intestine in fetuses with open-NTDs [68].
Also, mild pelviectasis does not exclude fetal surgery. It must be distinguished from the unilateral obstruction of the ureteropelvic junction that does not allow fetal repair of the spinal defect [69].
Uterus and placenta
Complete imaging evaluation for enlistment to fetal MMC surgery includes the study of the uterus and placenta.
Twin pregnancy is an exclusion criterion, easily determined in the first trimester.
MRI and US findings proper of the uterus include structural alterations that can increase the risk of post-surgical compliances, such as preterm delivery. The cervix length is well displayed on the US and MRI sagittal images; according to the inclusion criteria, it must exceed 2 cm (Fig. 4). Instead, abnormal uterine findings are best characterised on MRI, as in the case of Mullerian Ducts Anomalies [70] and leiomyomas.
It is essential to characterise the localisation and placental functionality to detect placenta previa, placental abruption, and placenta accrete spectrum disorders [71].
Fetal-MRI structured report about open-NTDs
To treat all fetal and uterine-placental compartment features, we propose a structured report that allows an orderly and efficient report of the fetal MRI of spinal NTDs, which is helpful in pre-surgery intrauterine planning (Table 3). An example of structured report use and corresponding images are provided in Supplementary Material 1.
Post-surgery MRI
MRI after surgery is recommended to assess the success of the repair and the need for subsequent surgery or treatment for hydrocephalus. Post-surgical MRI is usually performed after birth, but there is evidence that in-utero MRI after six weeks from surgical repair can give information about the outcome of the surgery and the relative risk of subsequent intervention for hydrocephalus [66]. Changes in HBH and ventricular volume are consequences of the prenatal repair on CSF hydrodynamics (Fig. 5). If further studies confirm, post-surgical fetal MRI could be adopted as a standard. Prenatal MRI avoids some difficulties regarding neonatal MRI, first of all sedation, but the quality of images is lower. Several recent studies confirm the need for a post-surgery study as presurgical findings, such as mild ventriculomegaly (width between 10 and 15 mm) or the severity of the degree of HBH, have limited predictive value about the need for hydrocephalus treatment (VP shunt or an endoscopic third ventriculostomy with choroid plexus cauterisation [72]) in the first year postpartum [64, 66, 73].
The best predictors of subsequent need for hydrocephalus treatment in the first year postpartum in patients undergoing fetal MMC repair are:
-
Ventricular volume growth > 2.02 mL/week (higher enlargement than expected, calculated using T2-WI from the pre- and post-surgery MRI);
-
The persistence of HBH below the level of the C1 posterior arch and lack of reversal of HBH at 6-week post-surgery MRI;
-
And mean ventricular width ≥ 15 mm on pre-surgery ultrasound or MRI [66].
Although the latter parameter is pre-surgical, it does not exclude in-utero repair because motor function benefits may be maintained [64, 66]. Ventriculomegaly, once established, does not appear to resolve. Still, the modification in post-operative CSF hydrodynamics could delay the VP shunt in patients in-utero repaired compared to those not repaired [65].
In the context of patients repaired in utero, many studies are emerging to identify those needing further treatment for hydrocephalus; in particular, the use of diffusion tensor imaging (DTI) has been proposed [74].
As regards the spine, there will be the typical imaging of an elongated spinal cord with the neural placode attached to the back of the thecal sac at the repair site with the common tethered spinal cord [75] (Fig. 6). Another assessment to be carried out concerns spinal cord syrinx or pre-syrinx oedema or other surgery complications [46], such as post-operative extra-spinal fluid collections or pseudomeningoceles [76].
T2 SSFSE sagittal and axial views at pre-surgery time during 24 gestational weeks (a and b, respectively) show bone and skin defect (arrow) with herniation of the dural sac and neural placode protruding outside skin surface. Sagittal T2 balanced steady-state gradient echo sequence (c) at post-surgery time during 29 gestational weeks shows the typical imaging of the elongated spinal cord with the neural placode attached to the back of the thecal sac at the repair site and, in axial view (d), the continuity of skin and bone after intrauterine repair. T2 Turbo Spin Echo sagittal view of the spine at the postnatal time (e) shows the typical imaging of tethered spinal cord
Conclusion
In the background of fetal surgical repair as the best therapeutic option for open-NTDs, fetal MRI is evolving to support therapeutic decisions through comprehensive information about fetal conditions. MRI may have a pivotal role in the post-surgical period when detecting the effectiveness and repair complications is essential. Radiologists need to know and report all crucial information to clinicians and surgeons for the best management of open NTDs.
References
Bhide P, Sagoo GS, Moorthie S et al (2013) Systematic review of birth prevalence of neural tube defects in India. Birth Defects Res A 97:437–443. https://doi.org/10.1002/bdra.23153
Januschek E, Röhrig A, Kunze S et al (2016) Myelomeningocele — a single institute analysis of the years 2007 to 2015. Childs Nerv Syst 32:1281–1287. https://doi.org/10.1007/s00381-016-3079-1
Parker SE, Mai CT, Canfield MA et al (2010) Updated national birth prevalence estimates for selected birth defects in the United States, 2004–2006. Birth Defects Res A Clin Mol Teratol 88:1008–1016. https://doi.org/10.1002/bdra.20735
Rabiu TB, Adeleye AO (2013) Prevention of myelomeningocele: African perspectives. Childs Nerv Syst 29:1533–1540. https://doi.org/10.1007/s00381-013-2126-4
Copp AJ, Greene NDE (2013) Neural tube defects-disorders of neurulation and related embryonic processes: neural tube defects-disorders of neurulation and related embryonic processes. WIREs Dev Biol 2:213–227. https://doi.org/10.1002/wdev.71
Volochovič J, Vaigauskaitė B, Varnelis P et al (2021) Intrauterine fetoscopic closure of myelomeningocele: clinical case and literature review. Taiwan J Obstet Gynecol 60:766–770. https://doi.org/10.1016/j.tjog.2021.05.032
Mitchell LE, Adzick NS, Melchionne J et al (2004) Spina bifida. Lancet 364:1885–1895. https://doi.org/10.1016/S0140-6736(04)17445-X
Shoja MM, Johal J, Oakes WJ, Tubbs RS (2018) Embryology and pathophysiology of the Chiari I and II malformations: a comprehensive review: embryology and pathophysiology of the Chiari I and II malformations. Clin Anat 31:202–215. https://doi.org/10.1002/ca.22939
Copp AJ, Adzick NS, Chitty LS et al (2015) Spina bifida. Nat Rev Dis Primers 1:15007. https://doi.org/10.1038/nrdp.2015.7
Stevenson KL (2004) Chiari type II malformation: past, present, and future. FOC 16:1–7. https://doi.org/10.3171/foc.2004.16.2.6
Paslaru FG, Panaitescu AM, Iancu G et al (2021) Myelomeningocele surgery over the 10 Years following the MOMS trial: a systematic review of outcomes in prenatal versus postnatal surgical repair. Medicina 57:707. https://doi.org/10.3390/medicina57070707
Yamashiro KJ, Galganski LA, Hirose S (2019) Fetal myelomeningocele repair. Semin Pediatr Surg 28:150823. https://doi.org/10.1053/j.sempedsurg.2019.07.006
Ben Miled S, Loeuillet L, Duong Van Huyen J-P et al (2020) Severe and progressive neuronal loss in myelomeningocele begins before 16 weeks of pregnancy. Am J Obstet Gynecol 223:256.e1-256.e9. https://doi.org/10.1016/j.ajog.2020.02.052
Adzick NS, Thom EA, Spong CY et al (2011) A Randomized trial of prenatal versus postnatal repair of myelomeningocele. N Engl J Med 364:993–1004. https://doi.org/10.1056/NEJMoa1014379
Espinoza J, Belfort MA, Whitehead W et al (2021) 81 A three-layer fetoscopic spina bifida closure has fewer neonatal complications than open in-utero closure. Am J Obstet Gynecol 224:S56–S57. https://doi.org/10.1016/j.ajog.2020.12.082
Sacco A, Van der Veeken L, Bagshaw E et al (2019) Maternal complications following open and fetoscopic fetal surgery: a systematic review and meta-analysis. Prenat Diagn 39:251–268. https://doi.org/10.1002/pd.5421
Kabagambe SK, Jensen GW, Chen YJ et al (2018) Fetal surgery for myelomeningocele: a systematic review and meta-analysis of outcomes in fetoscopic versus open repair. Fetal Diagn Ther 43:161–174. https://doi.org/10.1159/000479505
Joyeux L, Engels AC, Russo FM et al (2016) Fetoscopic versus open repair for spina bifida aperta: a systematic review of outcomes. Fetal Diagn Ther 39:161–171. https://doi.org/10.1159/000443498
Pedreira DAL, Zanon N, Nishikuni K et al (2016) Endoscopic surgery for the antenatal treatment of myelomeningocele: the CECAM trial. Am J Obstet Gynecol 214:111.e1-111.e11. https://doi.org/10.1016/j.ajog.2015.09.065
Kohl T (2014) Percutaneous minimally invasive fetoscopic surgery for spina bifida aperta. Part I: surgical technique and perioperative outcome. Ultrasound Obstet Gynecol 44:515–524. https://doi.org/10.1002/uog.13430
Degenhardt J, Schürg R, Winarno A et al (2014) Percutaneous minimal-access fetoscopic surgery for spina bifida aperta. Part II: maternal management and outcome. Ultrasound Obstet Gynacol 44:525–531. https://doi.org/10.1002/uog.13389
Chmait RH, Chu J, Kontopoulos EV et al (2021) 80 Outcomes of percutaneous fetoscopic open spina bifida (OSB) repair. Am J Obstet Gynecol 224:S56. https://doi.org/10.1016/j.ajog.2020.12.081
Diehl D, Belke F, Kohl T et al (2021) Fully percutaneous fetoscopic repair of myelomeningocele: 30-month follow-up data. Ultrasound Obstet Gynecol 57:113–118. https://doi.org/10.1002/uog.22116
Packer CH, Hersh AR, Caughey AB (2021) Fetoscopic compared with open repair of myelomeningocele: a 2-delivery cost-effectiveness analysis. Am J Obstet Gynecol MFM 3:100434. https://doi.org/10.1016/j.ajogmf.2021.100434
Meller C et al (2021) Update on prenatal diagnosis and fetal surgery for myelomeningocele. Arch Argent Pediat. https://doi.org/10.5546/aap.2021.eng.e215
Chaoui R, Benoit B, Mitkowska-Wozniak H et al (2009) Assessment of intracranial translucency (IT) in the detection of spina bifida at the 11–13-week scan. Ultrasound Obstet Gynecol 34:249–252. https://doi.org/10.1002/uog.7329
Engels AC, Joyeux L, Brantner C et al (2016) Sonographic detection of central nervous system defects in the first trimester of pregnancy: first-trimester detection of CNS malformations. Prenat Diagn 36:266–273. https://doi.org/10.1002/pd.4770
Ushakov F, Sacco A, Andreeva E et al (2019) Crash sign: new first-trimester sonographic marker of spina bifida. Ultrasound Obstet Gynecol 54:740–745. https://doi.org/10.1002/uog.20285
Moise KJ, Moldenhauer JS, Bennett KA et al (2016) Current selection criteria and perioperative therapy used for fetal myelomeningocele surgery. Obstet Gynecol 127:593–597. https://doi.org/10.1097/AOG.0000000000001296
Carreras E, Maroto A, Illescas T et al (2016) Prenatal ultrasound evaluation of segmental level of neurological lesion in fetuses with myelomeningocele: development of a new technique: functional ultrasound in MMC. Ultrasound Obstet Gynecol 47:162–167. https://doi.org/10.1002/uog.15732
Triulzi F, Manganaro L, Volpe P (2011) Fetal magnetic resonance imaging: indications, study protocols and safety. Radiol med 116:337–350. https://doi.org/10.1007/s11547-011-0633-5
Prayer D, Malinger G, Brugger PC et al (2017) ISUOG Practice Guidelines: performance of fetal magnetic resonance imaging. Ultrasound Obstet Gynecol 49:671–680. https://doi.org/10.1002/uog.17412
Manganaro L, Bernardo S, Antonelli A et al (2017) Fetal MRI of the central nervous system: state-of-the-art. Eur J Radiol 93:273–283. https://doi.org/10.1016/j.ejrad.2017.06.004
Yamashita Y, Namimoto T, Abe Y et al (1997) MR imaging of the fetus by a HASTE sequence. Am J Roentgenol 168:513–519. https://doi.org/10.2214/ajr.168.2.9016238
Brugger PC, Stuhr F, Lindner C, Prayer D (2006) Methods of fetal MR: beyond T2-weighted imaging. Eur J Radiol 57:172–181. https://doi.org/10.1016/j.ejrad.2005.11.017
Asenbaum U, Brugger PC, Woitek R et al (2013) Indikationen und technik der fetalen magnetresonanztomographie. Radiologe 53:109–115. https://doi.org/10.1007/s00117-012-2397-x
Prayer D, Brugger PC, Kasprian G et al (2006) MRI of fetal acquired brain lesions. Eur J Radiol 57:233–249. https://doi.org/10.1016/j.ejrad.2005.11.023
Righini A, Bianchini E, Parazzini C, et al (2003) Apparent diffusion coefficient determination in normal fetal brain: a prenatal MR imaging study. 6
Sanz Cortes M, Lapa DA, Acacio GL et al (2019) Proceedings of the first annual meeting of the international fetoscopic myelomeningocele repair consortium: international fetoscopic myelomeningocele repair consortium. Ultrasound Obstet Gynecol 53:855–863. https://doi.org/10.1002/uog.20308
Nagaraj UD, Kline-Fath BM (2020) Imaging of open spinal dysraphisms in the era of prenatal surgery. Pediatr Radiol 50:1988–1998. https://doi.org/10.1007/s00247-020-04734-w
Kumar I, Sachan A, Aggarwal P et al (2020) Structured MRI reporting in spinal dysraphism. Acta Radiol 61:1520–1533. https://doi.org/10.1177/0284185120903445
Heuer GG, Adzick NS, Sutton LN (2015) Fetal myelomeningocele closure: technical considerations. Fetal Diagn Ther 37:166–171. https://doi.org/10.1159/000363182
Kumar J, Afsal M, Garg A (2017) Imaging spectrum of spinal dysraphism on magnetic resonance: a pictorial review. WJR 9:178. https://doi.org/10.4329/wjr.v9.i4.178
Coleman BG, Langer JE, Horii SC (2015) the diagnostic features of spina bifida: the role of ultrasound. Fetal Diagn Ther 37:179–196. https://doi.org/10.1159/000364806
Aaronson OS, Hernanz-Schulman M, Bruner JP et al (2003) Myelomeningocele: prenatal evaluation—comparison between transabdominal US and MR imaging. Radiology 227:839–843. https://doi.org/10.1148/radiol.2273020535
Nagaraj UD, Bierbrauer KS, Stevenson CB et al (2018) Spinal imaging findings of open spinal dysraphisms on fetal and postnatal MRI. AJNR Am J Neuroradiol 39:1947–1952. https://doi.org/10.3174/ajnr.A5760
Nagaraj UD, Bierbrauer KS, Stevenson CB et al (2018) Myelomeningocele versus myelocele on fetal mr images: are there differences in brain findings? Am J Roentgenol 211:1376–1380. https://doi.org/10.2214/AJR.18.20088
Cherian J, Staggers KA, Pan I-W et al (2016) Thirty-day outcomes after postnatal myelomeningocele repair: a national surgical quality improvement program pediatric database analysis. PED 18:416–422. https://doi.org/10.3171/2016.1.PEDS15674
Trenga AP, Singla A, Feger MA, Abel MF (2016) Patterns of congenital bony spinal deformity and associated neural anomalies on X-ray and magnetic resonance imaging. J Child Orthop 10:343–352. https://doi.org/10.1007/s11832-016-0752-6
Reghunath A, Ghasi RG, Aggarwal A (2021) Unveiling the tale of the tail: an illustration of spinal dysraphisms. Neurosurg Rev 44:97–114. https://doi.org/10.1007/s10143-019-01215-z
Ansari S, Nejat F, Yazdani S, Dadmehr M (2007) Split cord malformation associated with myelomeningocele. J Neurosurg Pediatr 107:281–285. https://doi.org/10.3171/PED-07/10/281
Iskandar J, McLaughlin C, Oakes WJB (2000) Split cord malformations in myelomeningocele patients. Br J Neurosurg 14:200–203. https://doi.org/10.1080/026886900408360
Pang D, Dias MS, Ahab-Barmada M (1992) Split cord malformation. Neurosurgery 31:451–480. https://doi.org/10.1227/00006123-199209000-00010
Tsitouras V, Sgouros S (2013) Syringomyelia and tethered cord in children. Childs Nerv Syst 29:1625–1634. https://doi.org/10.1007/s00381-013-2180-y
Bixenmann BJ, Kline-Fath BM, Bierbrauer KS, Bansal D (2014) Prenatal and postnatal evaluation for syringomyelia in patients with spinal dysraphism: clinical article. PED 14:316–321. https://doi.org/10.3171/2014.5.PEDS13482
Levine DN (2004) The pathogenesis of syringomyelia associated with lesions at the foramen magnum: a critical review of existing theories and proposal of a new hypothesis. J Neurol Sci 220:3–21. https://doi.org/10.1016/j.jns.2004.01.014
Bradley KA, Juranek J, Romanowska-Pawliczek A et al (2016) Plasticity of interhemispheric temporal lobe white matter pathways due to early disruption of corpus callosum development in spina bifida. Brain Connect 6:238–248. https://doi.org/10.1089/brain.2015.0387
Kunpalin Y, Richter J, Mufti N et al (2021) Cranial findings detected by second-trimester ultrasound in fetuses with myelomeningocele: a systematic review. BJOG: Int J Obstet Gynaecol 128:366–374. https://doi.org/10.1111/1471-0528.16496
Trigo L, Eixarch E, Bottura I et al (2021) Prevalence of supratentorial anomalies assessed by fetal magnetic resonance in fetuses with open spina bifida. Ultrasound Obstet Gynecol. https://doi.org/10.1002/uog.23761
Woitek R, Dvorak A, Weber M et al (2014) MR-based morphometry of the posterior fossa in fetuses with neural tube defects of the spine. PLoS ONE 9:e112585. https://doi.org/10.1371/journal.pone.0112585
Sutton LN (1999) Improvement in hindbrain herniation demonstrated by serial fetal magnetic resonance imaging following fetal surgery for myelomeningocele. JAMA 282:1826. https://doi.org/10.1001/jama.282.19.1826
Nagaraj UD, Bierbrauer KS, Zhang B et al (2017) Hindbrain herniation in Chiari II malformation on fetal and postnatal MRI. AJNR Am J Neuroradiol 38:1031–1036. https://doi.org/10.3174/ajnr.A5116
Melchiorre K, Bhide A, Gika AD et al (2009) Counseling in isolated mild fetal ventriculomegaly. Ultrasound Obstet Gynecol 34:212–224. https://doi.org/10.1002/uog.7307
Tulipan N, Wellons JC, Thom EA et al (2015) Prenatal surgery for myelomeningocele and the need for cerebrospinal fluid shunt placement. PED 16:613–620. https://doi.org/10.3171/2015.7.PEDS15336
Tulipan N, Bruner JP, Hernanz-Schulman M et al (1999) Effect of intrauterine myelomeningocele repair on central nervous system structure and function. Pediatr Neurosurg 31:183–188. https://doi.org/10.1159/000028859
Zarutskie A, Guimaraes C, Yepez M et al (2019) Prenatal brain imaging for predicting need for postnatal hydrocephalus treatment in fetuses that had neural tube defect repair in utero. Ultrasound Obstet Gynecol 53:324–334. https://doi.org/10.1002/uog.20212
Sepulveda W, Ximenes R, Wong AE et al (2012) Fetal magnetic resonance imaging and three-dimensional ultrasound in clinical practice: applications in prenatal diagnosis. Best Pract Res Clin Obstet Gynaecol 26:593–624. https://doi.org/10.1016/j.bpobgyn.2012.06.001
Nagaraj UD, Calvo-Garcia MA, Merrow AC et al (2018) Decreased rectal meconium signal on MRI in fetuses with open spinal dysraphism. Prenat Diagn 38:870–875. https://doi.org/10.1002/pd.5344
Nguyen HT, Benson CB, Bromley B et al (2014) Multidisciplinary consensus on the classification of prenatal and postnatal urinary tract dilation (UTD classification system). J Pediatr Urol 10:982–998. https://doi.org/10.1016/j.jpurol.2014.10.002
Behr SC, Courtier JL, Qayyum A (2012) Imaging of Müllerian duct anomalies. Radiographics 32:E233–E250. https://doi.org/10.1148/rg.326125515
Fadl S, Moshiri M, Fligner CL et al (2017) Placental imaging: normal appearance with review of pathologic findings. Radiographics 37:979–998. https://doi.org/10.1148/rg.2017160155
Warf BC, Campbell JW (2008) Combined endoscopic third ventriculostomy and choroid plexus cauterization as primary treatment of hydrocephalus for infants with myelomeningocele: long-term results of a prospective intent-to-treat study in 115 East African infants: clinical article. PED 2:310–316. https://doi.org/10.3171/PED.2008.2.11.310
Bruner JP, Tulipan N, Reed G et al (2004) Intrauterine repair of spina bifida: preoperative predictors of shunt-dependent hydrocephalus. Am J Obstet Gynecol 190:1305–1312. https://doi.org/10.1016/j.ajog.2003.10.702
Mangano FT, Stevenson CB, Nagaraj U et al (2020) Abnormal anisotropic diffusion properties in pediatric myelomeningocele patients treated with fetal surgery: an initial DTI study. Childs Nerv Syst 36:827–833. https://doi.org/10.1007/s00381-019-04339-1
Hudgins RJ, Gilreath CL (2004) Tethered spinal cord following repair of myelomeningocele. FOC 16:1–4. https://doi.org/10.3171/foc.2004.16.2.8
Surapaneni S, Hasoon J, Orhurhu V et al (2020) Presentation and management of a postoperative spinal pseudomeningocele. Pain Ther 9:333–335. https://doi.org/10.1007/s40122-019-00139-2
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript. The authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have not disclosed any competing interests.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Avesani, G., Perazzolo, A., Elia, L. et al. Fetal MRI prior to intrauterine surgery of open neural tube defects: What does the radiologist need to know. Radiol med 128, 113–124 (2023). https://doi.org/10.1007/s11547-022-01579-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-022-01579-1