Abstract
Introduction
Posterior reversible encephalopathy syndrome (PRES) is a clinico-neuroradiological entity, characterized by typical neurological deficits, distinctive magnetic resonance imaging (MRI) features, and a usually benign clinical course. Although frequently seen in association with hypertensive conditions, many other predisposing factors, notably cytotoxic and immunosuppressant drugs have been associated with PRES. The aim of this study was to determine differences in the MR appearance of PRES according to various risk factors.
Methods
Thirty consecutive patients with clinical and MRI findings consistent with PRES were included. We identified 24 patients with hypertension-related conditions, including 14 patients with preeclampsia–eclampsia, and six patients without hypertension, in whom PRES was associated with exposition to neurotoxic substances. Lesion distribution, extent of disease, and number of affected brain regions were compared between patients with PRES with and without hypertension, and patients with PRES with and without preeclampsia–eclampsia, respectively.
Results
No statistically significant differences in distribution of lesions and extent of disease were observed between patients with PRES with or without hypertension, and patients with or without preeclampsia–eclampsia, respectively. The number of affected brain regions was significantly higher in patients with preeclampsia–eclampsia (p = 0.046), and the basal ganglia region was more frequently involved in these patients (p = 0.066).
Conclusion
Apart from a significant higher number of involved brain regions and a tendency for basal ganglia involvement in patients with PRES associated with preeclampsia–eclampsia, the MRI appearance of patients with PRES does not seem to be influenced by predisposing risk factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Posterior reversible encephalopathy syndrome (PRES) is characterized by a combination of typical neurological symptoms and distinctive imaging findings. Clinical symptoms evolve within a few hours and include headaches, visual disturbances, seizures, altered mental state, and occasionally, focal neurological deficits. Magnetic resonance imaging (MRI) typically reveals bilateral, symmetric, T2-hyperintense signal alterations in the cortical and subcortical regions of the parietal and occipital lobes. In addition to these classic brain locations, involvement of the frontal and temporal lobes, as well as the basal ganglia, the brain stem, and the cerebellum has been described in patients with PRES [1, 2]. The clinical course is variable and ranges from complete reversibility of clinical and imaging findings to progression to ischemia, massive infarction, and death [3–5].
PRES was first described as a separate disease entity by Hinchey et al. in 1996 in patients with eclampsia, renal diseases, and patients who were taking immunosuppressive drugs [1]. Since then, a variety of medical conditions and drugs have been associated with this syndrome [5–9]. The pathophysiology of PRES is incompletely understood. But, given that most cases manifest with acute to subacute hypertension, the current more popular theory is that of a breakdown of the cerebral blood flow autoregulatory control due to an increased systemic blood pressure that leads to overwhelming vasodilatation and vasogenic edema [10, 11].
However, the fact that PRES has also been reported in patients without evidence of hypertension raises the possibility of a direct endothelial dysfunction due to circulating toxins, which may cause damage of the blood–brain barrier and subsequent extravasation [1, 12, 13].
Based on the different potential etiologies of PRES, the aims of this study were to categorize the distribution and severity of PRES on MRI according to different risk factors and to analyze whether differences in the MR appearance of PRES might support a theory of either direct hypertensive or toxic effects on vascular endothelial cells as pathogenic mechanisms.
Materials and methods
Subjects
We reviewed the MRI examinations of 30 consecutive patients with PRES (21 female patients, nine male patients; age range, 8–73 years; mean age, 42 ± 21years) who were investigated in the radiology department of our hospital during a 51-month period between October 2003 and January 2008. The patients were identified by searching the radiology report database at our institution for the key words “PRES”, “posterior reversible encephalopathy syndrome”, or “hypertensive encephalopathy”. We used the following inclusion criteria: (1) acute presentation with at least one of the following neurological symptoms: headache, seizures, visual disturbances, and mental status changes; (2) presence of a risk factor for PRES (e.g., preeclampsia–eclampsia, exposure to cytotoxic or immunosuppressant drug therapy, renal diseases); (3) MR examinations showing bilateral T2-weighted signal intensity abnormalities; and (4) complete or partial resolution of the signal intensity abnormalities in all patients with more than one MR examination (n = 21). For all patients, the MRI studies were performed between the first and third days of the onset of clinical symptoms.
Medical records were searched for clinical data, such as symptoms, highest blood pressure, level of creatinine, and lactate dehydrogenase (LDH), at the time of the event.
The presence of hypertension was defined according to the WHO guidelines (systolic blood pressure (SBP) >140 or diastolic blood pressure (DBP) >90). In two children with PRES (a 9-year-old boy, 14-year-old girl), the highest BP at the time of presentation was correlated with the standardized, age-related mean BP as defined by the National High Blood Pressure Education Program (NHBPEP) Working Group (hypertension: average SBP and/or DBP ≥95th percentile for gender, age, and height ≥3 occasions) [14].
MRI protocol
All exams were performed on a 1.5-T MRI scanner (Gyroscan NT-Intera, Philips, Netherlands). Our standard imaging protocol consisted of axial fluid-attenuated inversion-recovery (FLAIR)-weighted images (TR/TE/TI 11,000/120/2,800 ms), coronal T2-weighted images (TR/TE/ 4,000/90 ms, flip angle 90°), axial T1-weighted images (TR/TE/ 24/2 ms, flip angle 90°), and DWI (TR/TE 3,120/90 ms). The diffusion-sensitizing gradient was applied along the three main axes (x, y, and z) and images were acquired at b values of 0, 500, and 1,000 s/mm2. Apparent diffusion coefficient (ADC) maps were created for all patients on a pixel-by-pixel basis using commercially available software provided by the manufacturers.
Image analysis
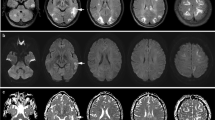
For all patients, involvement of the following nine brain regions was assessed on FLAIR-weighted images by two of the authors in consensus: occipital lobes, parietal lobes, temporal lobes, frontal lobes, basal ganglia, thalami, corpus callosum, cerebellar hemispheres, and pons. In all regions except the corpus callosum, the involvement of each side was evaluated separately. The extent of the abnormal signal in each region was graded on a scale of 0 to 3 (0: normal-appearing brain parenchyma, 1: subtle signal abnormalities that are only faintly visible, 2: large confluent areas of high-signal intensity abnormalities that are easily perceptible, 3: complete involvement of the brain region; Fig. 1). The diffusion-weighted imaging (DWI) studies were searched for the presence of high-signal intensities and, in cases of positive findings, the corresponding ADC values were evaluated.
Measurement of disease extent in the occipital lobe in three different patients. Grade 1 indicates subtle signal abnormalities that are only faintly visible; grade 2 indicates large confluent areas of high-signal intensity abnormalities that are easily perceptible; and grade 3 indicates complete involvement of the brain region
Statistical analysis
All statistical analyses were performed with the SPSS program for Windows (version 15.0). Differences in lesion distribution and extent of disease between hypertensive and normotensive patients and patients with and without eclampsia were determined by performing the chi-square test and the Mann–Whitney U test. A probability value of less than or equal to 0.05 was considered statistically significant.
Results
Clinical findings
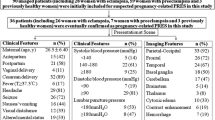
Table 1 summarizes the demographic information and clinical presentation of all patients. In patients with more than one factor that may have led to PRES, we used the patient’s clinical presentation to determine which factor was most relevant.
Of 30 patients with PRES, 24 patients (80%) had systemic hypertension at the time of the acute event. The most common associated condition in patients with PRES and systemic hypertension was preeclampsia–eclampsia (n = 10), followed by patients suffering from acute or chronic renal failure (n = 6), and patients receiving chemotherapeutic and immunosuppressant agents [cyclophosphamide (n = 2), cyclosporine A (n = 2), tacrolimus/FK-506 (n = 1)]; one patient developed PRES during an allergic shock after intake of strawberries and nuts; in two patients, PRES occurred during a hypertensive crisis after multi-drug abuse and 1 day after surgery for an ovarian carcinoma, respectively;
In six of 30 patients (20%), the systemic blood pressure level when PRES occurred was within normal limits. Three of six patients with PRES and normal BP were receiving immunosuppressive agents, such as tacrolimus/FK-506 (n = 2) and cyclosporine A (n = 1). One patient with PRES received high dose cyclophosphamide for treatment of systemic lupus erythematosus. Two patients with normotensive PRES developed symptoms during chemotherapy for treatment of pancreatic carcinoma (gemcitabine and oxaliplatin, #18) and multiple myeloma (Velcade®, generic name: Bortezomib, #15), respectively.
In one patient with PRES and tacrolimus/FK-506 therapy, the drug blood level was potentially toxic (#9); in all other patients with PRES and immunosuppressive drug therapy or chemotherapy, drug levels were within the therapeutic range at presentation.
Two patients died 8 and 6 weeks after the acute event due to thromboembolic brain infarctions (#20) and multi-organ failure (#8), respectively. Six patients (#13, #14, #15, #28, #29, and #30) had residual symptoms at hospital dismissal, such as extremity weakness and confusion. The remaining patients were discharged without residual neurological symptoms.
No significant differences were seen in LDH levels (hypertensive patients: mean 393.83 ± 227.66 U/l; normotensive patients: mean 389.5 ± 152.62; normal range <248; Mann–Whitney U test, p = 0.77) or creatinine levels (hypertensive patients: mean 2.29 ± 2.36 mg/dl; normotensive patients: mean 2.44 ± 2.06 mg/dl; Mann–Whitney U test, p = 0.454) between patients with normotensive and hypertensive PRES.
Imaging findings
MR appearance of pathological changes
Signal intensity abnormalities on T2-weighted and FLAIR images were bilaterally symmetric in five patients only; in all other patients, asymmetric involvement of at least one brain region was observed. In four female patients and in one male patient with PRES and hypertension, the initial MRI revealed parenchymal hemorrhage [right caudate nucleus (1 cm) with intraventricular extension (#4; Fig. 2), left parietal lobe (0.8 cm; #14), right parietal lobe (2 cm; #28), parietal lobes bilaterally (1 cm, 0.3 cm; #16), left pons (0.4 cm; #30)]. In one patient with PRES and preeclampsia–eclampsia (#26), subarachnoid hemorrhage was present on initial MRI in the right parietal region.
PRES in a 39-year-old patient (#4) with eclampsia 2 days after delivery. a–c FLAIR-weighted images show extensive, bilateral, abnormal signal intensity in the parietooccipital lobes, the pons, the thalamus, the basal ganglia, and the corpus callosum (splenium). The heterogeneous signal in the right basal ganglia is caused by additional intracerebral hemorrhage with intraventricular extension (arrow). Some smaller foci of abnormal signal are present in the temporal and frontal lobes and in the left cerebellum; d diffusion-weighted MRI shows normal to slightly hyperintense signal intensity in the areas of the FLAIR abnormality, indicating “T2 shine through”. The distinct hyperintense area in the right lateral ventricle is due to hemorrhage
On DWI, most patients (n = 22) had edema isointense to normal-appearing parenchyma. In seven patients with PRES and hypertensive conditions, DWI revealed high-signal intensity abnormalities in the cortical to subcortical regions of the frontal and parietal lobes with isointensity to hyperintensity on ADC maps (Fig. 3), and thus represented “T2 shine through effect”. In one patient (#30), an area of restricted diffusion was present in the left cerebellar hemisphere (0.5 cm), indicating progression to ischemic infarction. None of our patient showed tumefactive edema on FLAIR- or T2-weighted imaging.
A 46-year-old female patient (#8) with PRES related to multi-drug abuse. a FLAIR-weighted image shows extensive, rather symmetric, hyperintense signal intensity in the parietal and posterior frontal lobes; b diffusion-weighted MRI shows band-like high signal intensity in the left pre- and post-central gyrus (arrowhead); c ADC map shows normal signal throughout the brain. The areas of high signal in b (arrowhead) do not have low ADC values, as would be expected in the setting of brain ischemia
Follow-up MRI was performed in 21 patients, with a time interval from the initial MR examination between 1 and 25 days. In five patients, follow-up MRI revealed complete resolution of signal alterations, whereas in all other patients, there was improvement of PRES-related signal alterations.
Lesion distribution
Statistical evaluation did not reveal any significant difference between the normotensive and hypertensive patient groups with regard to the location of affected brain regions; the occipital lobes were the most commonly affected brain region in both the hypertensive and the normotensive patient groups and were involved in all but two patients (93%). The second most commonly affected brain regions were the frontal lobes and the cerebellum in 16 (53%) and 13 patients (43%), respectively. The parietal lobes were affected in 12 (40%), and the temporal lobes in ten patients (33%). The pons was affected in nine patients (30%), three of whom suffered from preeclampsia–eclampsia. The basal ganglia were exclusively affected in patients with elevated blood pressure levels (n = 9; 30%) and six of whom suffered from preeclampsia–eclampsia. There was a tendency toward involvement of the basal ganglia in patients with preeclampsia–eclampsia compared to patients without preeclampsia–eclampsia (Mann–Whitney U test, p = 0.066). Basal ganglia involvement, at least unilateral, was apparent in 60% of patients with preeclampsia–eclampsia compared to 18.2% in non-eclamptic patients. Of seven patients with lesions in the thalamic regions, four were suffering from preeclampsia–eclampsia and, in five of seven patients with thalamic involvement, the basal ganglia were affected simultaneously. The corpus callosum was affected in four patients, two of whom had normal blood pressure levels.
Extent of edema and number of affected brain regions
There was no statistically significant difference between the extent of edema in the various brain regions in patients with hypertension compared to patients without hypertension. When patients with or without preeclampsia–eclampsia were compared, there was also no statistically significant difference with regard to disease severity.
In all but three patients, more than one brain region was involved (Fig. 4). With regard to the number of affected brain regions, there was a significant difference between patients with and without preeclampsia–eclampsia. The mean number of affected brain regions in patients with preeclampsia–eclampsia was 4.9 ± 1.66 compared to 3.74 ± 1.84 brain regions in patients without preeclampsia–eclampsia (Mann–Whitney U test, p = 0.046).
a, b FLAIR-weighted images in a 14-year-old patient (#20) with PRES, related to cyclophosphamide therapy, show marked frontal and parietooccipital involvement; c, d FLAIR-weighted images in a 29-year-old patient (#2) with PRES, related to preeclampsia–eclampsia, show only subtle involvement of the right occipital lobe (arrow) and marked involvement of the brainstem and the basal ganglia (arrowheads)
Discussion
PRES is considered as a variant of hypertensive encephalopathy, and although an elevation of the blood pressure is not required for the diagnosis, it is largely believed that hypertension is one of the main predisposing factors for PRES [1, 15]. Previous reports have speculated that the degree of hypertension necessary to induce encephalopathy depends on the baseline pressure, and thus, PRES can occur even with blood pressures that are close to the acceptable range of normotensive if the pressure represents a substantial elevation above the patient’s normotensive standard [15, 16]. However, the fact that PRES is increasingly observed in patients on immunosuppressive therapy or chemotherapy, and in patients with infection, sepsis, and shock without elevation of the systemic blood pressure, implies that there could be a different, or at least an additional, pathophysiologic mechanism contributing to the disease pattern [2, 5]. Several immunosuppressive and chemotherapeutic substances have been reported to be associated with PRES, most notably cyclosporine A and tacrolimus/FK-506 [1, 2, 5, 17, 18].
In the present study, the development of PRES was attributed to immunosuppressive or chemotherapeutic treatment in 11/30 patients (36%); five of these patients had mild to severe hypertension, and the remaining six patients had normal systemic blood pressure levels at the time of the acute event. The most common pharmacological agents were tacrolimus/FK-506, cyclophosphamide, and cyclosporine A in three patients each. It has been shown that cyclosporine has direct toxic effects on vascular endothelial cells by inducing apoptosis [19, 20]. Experimental data indicate similar, but less severe, cytotoxic effects on the brain capillary endothelial cells with tacrolimus/FK-506 [21, 22]. The theory of direct endothelial injury is supported by a previous study by McKinney et al., where gyriform enhancement has been observed not only in hypertensive but also in non-hypertensive patients with PRES [2]. In these cases, the breakdown of the blood–brain barrier cannot be explained by the theory of severe hypertension leading to failed autoregulation and subsequent hyperperfusion [10]. In addition, cyclosporine is known to cause the release of potent vasoconstrictors, such as endothelin, prostacyclin, and thromboxane A2 [23]. An alternative hypothesis, therefore, is that neuropeptide-mediated ischemia contributes to the neurotoxicity of cyclosporine A [24].
One new drug associated with PRES was identified: One of our patients developed PRES during treatment for multiple myeloma with Velcade® (generic name: bortezomib), and there was marked improvement of clinical and neuroradiological symptoms after termination of the therapy. Velcade® is a newly developed drug that inhibits the activity of the proteasome, an enzyme complex that regulates cell activities necessary for reproduction and survival. Velcade® therapy is associated with potentially severe peripheral neuropathy [25]; however, negative side effects on the central nervous system have not been described to date.
With regard to the large number of different chemotherapeutic and immunosuppressant agents that are associated with PRES, a recent publication by Bartynski has focused on an immunogenic process as a theory for possible endothelial dysfunction in patients with PRES [26]. This theory is supported by a case report of a patient with PRES after cardiac transplantation where brain biopsy revealed evidence of endothelial activation, with T-cell trafficking, and expression of vascular endothelial growth factor (VEGF) [27]. VEGF, which can also be upregulated by activated endothelial cells in the setting of significant hypoxemia, can increase endothelial permeability and could be responsible for the vasogenic edema in PRES [28]. A similar T-cell-mediated immune response could have been present in one of our patients who developed PRES during an anaphylactic shock after the intake of nuts and strawberries (#14) and in another case from the literature in a patient with anaphylaxis from iodinated contrast material [2].
Our study did not reveal any statistically significant difference between location and severity of brain involvement between patients with PRES and simultaneous hypertension (the majority related to preeclampsia–eclampsia or renal failure) and patients without hypertension (all of them related to cytotoxic or immunosuppressant drug therapy). The finding that the presence of hypertension does not result in more severe brain involvement is consistent with previous studies by Bartynski et al. [5, 29]. In these studies on PRES, the extent of vasogenic edema was even greater in normotensive patients than in severely hypertensive patients, contrary to the expected result if passive dilatation and hyperperfusion were the mechanism in PRES. The authors found a high incidence of vasculopathy with focal and diffuse vasoconstriction, focal vasodilatation, and a string-of-bead pattern on catheter angiography and MR angiography in most patients [29]. In addition, MR perfusion showed reduced cerebral blood flow in the majority of their patients, a finding that has also been described in previous studies on PRES and hypertensive encephalopathy [30, 31]. These observations are in contrast to the hypothesis of hypertension-induced autoregulatory failure leading to vasodilatation, hyperperfusion, and vasogenic edema, but support an alternate theory in the mechanism behind PRES. This second theory has been initially derived based on early imaging reports of eclampsia, cyclosporine neurotoxicity, and severe hypertension and suggests that hypertension leads to autoregulatory vasoconstriction with decreased perfusion, ischemia, and subsequent vasogenic edema [26]. According to a recent article by Bartynski and along with the previously described immunogenic theory, a complex underlying “systemic process” could be present in the majority of patients with PRES with similar underlying biologic features that lead to T-cell/endothelial cell activation and result in vasoconstriction and brain and systemic hypoperfusion [26].
Our study found basal ganglia involvement in 30% of patients with hypertension at least unilateral in comparison to none of the patients without hypertension. The majority of hypertensive patients with basal ganglia involvement suffered from preeclampsia–eclampsia (60%), and statistical evaluation showed a tendency toward involvement of the basal ganglia in these patients compared to patients without preeclampsia–eclampsia (p = 0.066). The predilection for basal ganglia involvement in patients with preeclampsia–eclampsia has been described in previous studies. In the largest study on 18 patients with preeclampsia–eclampsia and PRES by Demirtas et al., basal ganglia involvement was observed in 10/18 (55.5%) patients [32]. In further studies focusing on PRES and preeclampsia–eclampsia, the basal ganglia were affected in between 15% and 80% of patients, respectively [33–35]. In another study by McKinney et al., including among others cases with PRES and preeclampsia–eclampsia, basal ganglia involvement was seen in 11.8% of patients and hypertension has been observed in all of them [2].
In this series, basal ganglia involvement was present in three patients apart from preeclampsia–eclampsia; namely, in a female patient with an allergic shock (#14), and in a female patient (#22) and a male patient (#30) with acute renal failure. The pons and the thalamic region were simultaneously involved with the basal ganglia in six (66%) and five (56%) patients, respectively.
The predilection for involvement of the basal ganglia in patients with PRES and preeclampsia–eclampsia remains unclear. Circulating endothelial toxins, as well as antibodies against the endothelium have been associated with endothelial damage in patients with preeclampsia–eclampsia [13, 36]. Compared to the cortical gray matter, the basal ganglia consist of a different microvascular anatomy with a higher number of non-anastomotic vessels and capillary beds [37] and may therefore be more susceptible to insults from toxins. A similar endothelial activation could have been present in our two patients with renal failure due to uremic toxins, and in our patient with anaphylaxis due to circulating antigen–antibody complexes.
In our study, significantly more brain regions were affected in patients with preeclampsia–eclampsia compared to patients with PRES and other predisposing factors (p = 0.046). These findings may indicate a more severe brain involvement in patients with preeclampsia–eclampsia. However, taking into account the extent of disease within the affected brain regions, there was no significant difference between patients with and without preeclampsia–eclampsia. In addition, all patients with preeclampsia–eclampsia completely recovered after antihypertensive and/or anticonvulsive treatment, whereas six patients without preeclampsia–eclampsia, including two patients with parenchymal hemorrhage, had residual neurologic deficits at the time of the hospital dismissal.
In one patient with severe hypertension, a small area of restricted diffusion was present on DWI in the left cerebellar hemisphere, indicating a recent ischemic infarct. In all other patients, even when extensive vasogenic edema was present on the initial MRI, no progression to cytotoxic edema was seen on follow-up images. The incidence of restricted diffusion is remarkably low (<1%), compared to a previous study that reported progression to infarction in 17.3% [2]. We observed areas of cortical DWI hyperintensity with normal or slightly elevated ADC values in 23% of our patients on the initial MRI; all had hypertensive blood pressure levels. Despite previous reports indicating a worse outcome in patients with this constellation of DWI findings and ADC values, which has been referred to as “pseudonormalization” [3], the clinical outcome in our patients did not differ according to the DWI abnormalities. Hemorrhagic complications were present in six patients with PRES and hypertensive conditions (20%) and consisted of intracerebral hemorrhage in five, and subarachnoid hemorrhage in one patient. The overall incidence of hemorrhage in our patients is similar to a recent study that found hemorrhage in 17.1% of PRES cases [2]; however, in contrast to our study, subarachnoid hemorrhage was more common than parenchymal hemorrhage in this previous study.
Seizures were more frequent in patients with PRES and hypertension (75%) compared to patients without hypertension (33%). In addition, seizures were seen more frequently in patients with thalamic/basal ganglia involvement (91%) than in those without (53%). None of the normotensive patients complained about visual disturbances or headaches raising the possibility that these two symptoms are directly related to high blood pressure and not secondary to brain edema.
We have found elevated LDH and creatinine levels in patients with and without hypertension. High LDH levels are suggestive of microangiopathic hemolysis due to endothelial dysfunction and have been previously described in patients with PRES, in particular in association with preeclampsia–eclampsia [32, 33]. In our study, elevated creatinine levels have been found not only in patients with acute and chronic renal failure, but also in four patients apart from these risk factors. The observation of elevated LDH and creatinine levels suggests evolving multiple organ dysfunction coincident with the development of PRES and is consistent with the findings of a previous study in patients with PRES and infection, sepsis, and shock [5].
Due to its retrospective character and the heterogeneous sample of patients, our study has limitations. In some patients, several predisposing factors, such as hypertension, renal failure, and immunosuppressant drug therapy, were present simultaneously; however, to compare the MR appearance, a distribution to certain risk groups had to be performed, and to avoid selection bias, the objective criteria of presence/absence of hypertension (according to the WHO guidelines) and preeclampsia–eclampsia were chosen. Compared to other studies on PRES, we have a relatively high proportion of patients with preeclampsia–eclampsia. This could be explained by the fact that our hospital is a reference center for complications during pregnancy. In addition, due to the intense cooperation between the department of radiology and the department of obstetrics in our hospital, also cases with mild neurologic symptoms underwent MRI immediately and some of them showed only mild signs of PRES on MRI which might have been missed if they had delayed imaging.
Conclusion
In patients with PRES and preeclampsia–eclampsia, involvement of the basal ganglia was more common and significantly more brain regions were involved compared to patients with PRES and other risk factors. Apart from these findings, our study did not indicate any significant difference in the MRI appearance of patients with PRES, particularly when patients with PRES seen in association with hypertension were compared to non-hypertensive patients with PRES.
References
Hinchey J, Chaves C, Appignani B, Breen J, Pao L, Wang A, Pessin MS, Lamy C, Mas JL, Caplan LR (1996) A reversible posterior leukoencephalopathy syndrome. N Engl J Med 334:494–500. doi:10.1056/NEJM199602223340803
McKinney AM, Short J, Truwit CL, McKinney ZJ, Kozak OS, SantaCruz KS, Teksam M (2007) Posterior reversible encephalopathy syndrome: incidence of atypical regions of involvement and imaging findings. AJR Am J Roentgenol 189:904–912. doi:10.2214/AJR.07.2024
Covarrubias DJ, Luetmer PH, Campeau NG (2002) Posterior reversible encephalopathy syndrome: prognostic utility of quantitative diffusion-weighted MR images. AJNR Am J Neuroradiol 23:1038–1048
Bartynski WS, Boardman JF (2007) Distinct imaging patterns and lesion distribution in posterior reversible encephalopathy syndrome. AJNR Am J Neuroradiol 28:1320–1327. doi:10.3174/ajnr.A0549
Bartynski WS, Boardman JF, Zeigler ZR, Shadduck RK, Lister J (2006) Posterior reversible encephalopathy syndrome in infection, sepsis, and shock. AJNR Am J Neuroradiol 27:2179–2190
Ito Y, Arahata Y, Goto Y, Hirayama M, Nagamutsu M, Yasuda T, Yanagi T, Sobue G (1998) Cisplatin neurotoxicity presenting as reversible posterior leukoencephalopathy syndrome. AJNR Am J Neuroradiol 19:415–417
Russell MT, Nassif AS, Cacayorin ED, Awwad E, Perman W, Dunphy F (2001) Gemcitabine-associated posterior reversible encephalopathy syndrome: MR imaging and MR spectroscopy findings. Magn Reson Imaging 19:129–132. doi:10.1016/S0730-725X(01)00217-X
Kastrup O, Maschke M, Wanke I, Diener HC (2002) Posterior reversible encephalopathy syndrome due to severe hypercalcemia. J Neurol 249:1563–1566. doi:10.1007/s00415-002-0895-x
Ito Y, Niwa H, Iida T, Nagamatsu M, Yasuda T, Yanagi T, Sobue G (1997) Post-transfusion reversible posterior leukoencephalopathy syndrome with cerebral vasoconstriction. Neurology 49:1174–1175
Strandgaard S, Paulson OB (1984) Cerebral autoregulation. Stroke 15:413–416
Tamaki K, Sadoshima S, Baumbach GL, Iadecola C, Reis DJ, Heistad DD (1984) Evidence that disruption of the blood–brain barrier precedes reduction in cerebral blood flow in hypertensive encephalopathy. Hypertension 6:I75–I81
Mukherjee P, McKinstry RC (2001) Reversible posterior leukoencephalopathy syndrome: evaluation with diffusion-tensor MR imaging. Radiology 219:756–765
Rodgers GM, Taylor RN, Roberts JM (1988) Preeclampsia is associated with a serum factor cytotoxic to human endothelial cells. Am J Obstet Gynecol 159:908–914
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescent (2004) The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114:555–576. doi:10.1542/peds.114.2.S2.555
Port JD, Beauchamp NJ Jr (1998) Reversible intracerebral pathologic entities mediated by vascular autoregulatory dysfunction. Radiographics 18:353–367
Ay H, Buonanno FS, Schaefer PW, Le DA, Wang B, Gonzalez RG, Koroshetz WJ (1998) Posterior leukoencephalopathy without severe hypertension: utility of diffusion-weighted MRI. Neurology 51:1369–1376
Jansen O, Krieger D, Krieger S, Sartor K (1996) Cortical hyperintensity on proton density-weighted images: an MR sign of cyclosporine-related encephalopathy. AJNR Am J Neuroradiol 17:337–344
Rangi PS, Partridge WJ, Newlands ES, Waldman AD (2005) Posterior reversible encephalopathy syndrome: a possible late interaction between cytotoxic agents and general anaesthesia. Neuroradiology 47:586–590. doi:10.1007/s00234-005-1376-6
Benigni A, Morigi M, Perico N, Zoja C, Amuchastegui CS, Piccinelli A, Donadelli R, Remuzzi G (1992) The acute effect of FK506 and cyclosporine on endothelial cell function and renal vascular resistance. Transplantation 54:775–780. doi:10.1097/00007890-199211000-00002
Zoja C, Furci L, Ghilardi F, Zilio P, Benigni A, Remuzzi G (1986) Cyclosporin-induced endothelial cell injury. Lab Invest 55:455–462
Kochi S, Takanaga H, Matsuo H, Naito M, Tsuruo T, Sawada Y (1999) Effect of cyclosporin A or tacrolimus on the function of blood–brain barrier cells. Eur J Pharmacol 372:287–295. doi:10.1016/S0014-2999(99)00247-2
Kochi S, Takanaga H, Matsuo H, Ohtani H, Naito M, Tsuruo T, Sawada Y (2000) Induction of apoptosis in mouse brain capillary endothelial cells by cyclosporin A and tacrolimus. Life Sci 66:2255–2260. doi:10.1016/S0024-3205(00)00554-3
Marsen TA, Weber F, Egink G, Suckau G, Baldamus CA (1999) Cyclosporin A induces prepro endothelin-1 gene transcription in human endothelial cells. Eur J Pharmacol 379:97–106. doi:10.1016/S0014-2999(99)00447-1
Truwit CL, Denaro CP, Lake JR, DeMarco T (1991) MR imaging of reversible cyclosporin A-induced neurotoxicity. AJNR Am J Neuroradiol 12:651–659
Badros A, Goloubeva O, Dalal JS, Can I, Thompson J, Rapoport AP, Heyman M, Akpek G, Fenton RG (2007) Neurotoxicity of bortezomib therapy in multiple myeloma: a single-center experience and review of the literature. Cancer 110:1042–1049. doi:10.1002/cncr.22921
Bartynski WS (2008) Posterior reversible encephalopathy syndrome, part 2: controversies surrounding pathophysiology of vasogenic edema. AJNR Am J Neuroradiol 29:1043–1049. doi:10.3174/ajnr.A0929
Horbinski C, Bartynski WS, Carson-Walter E, Hamilton RL, Tan HP, Cheng S (2009) Reversible Encephalopathy after Cardiac Transplantation: Histologic Evidence of Endothelial Activation, T-cell Specific Trafficking, and Vascular Endothelial Growth Factor Expression. AJNR Am J Neuroradiol. doi:10.3174/ajnr.A1311
Schoch HJ, Fischer S, Marti HH (2002) Hypoxia-induced vascular endothelial growth factor expression causes vascular leakage in the brain. Brain 125:2549–2557. doi:10.1093/brain/awf257
Bartynski WS, Boardman JF (2008) Catheter angiography, MR angiography, and MR perfusion in posterior reversible encephalopathy syndrome. AJNR Am J Neuroradiol 29:447–455. doi:10.3174/ajnr.A0839
Brubaker LM, Smith JK, Lee YZ, Lin W, Castillo M (2005) Hemodynamic and permeability changes in posterior reversible encephalopathy syndrome measured by dynamic susceptibility perfusion-weighted MR imaging. AJNR Am J Neuroradiol 26:825–830
Sundgren PC, Edvardsson B, Holtas S (2002) Serial investigation of perfusion disturbances and vasogenic oedema in hypertensive encephalopathy by diffusion and perfusion weighted imaging. Neuroradiology 44:299–304. doi:10.1007/s00234-001-0721-7
Demirtas O, Gelal F, Vidinli BD, Demirtas LO, Uluc E, Baloglu A (2005) Cranial MR imaging with clinical correlation in preeclampsia and eclampsia. Diagn Interv Radiol 11:189–194
Schwartz RB, Feske SK, Polak JF, DeGirolami U, Iaia A, Beckner KM, Bravo SM, Klufas RA, Chai RY, Repke JT (2000) Preeclampsia–eclampsia: clinical and neuroradiographic correlates and insights into the pathogenesis of hypertensive encephalopathy. Radiology 217:371–376
Watanabe Y, Mitomo M, Tokuda Y, Yoshida K, Choi S, Hosoki T, Ban C (2002) Eclamptic encephalopathy: MRI, including diffusion-weighted images. Neuroradiology 44:981–985. doi:10.1007/s00234-002-0867-y
Servillo G, Striano P, Striano S, Tortora F, Boccella P, De Robertis E, Rossano F, Briganti F, Tufano R (2003) Posterior reversible encephalopathy syndrome (PRES) in critically ill obstetric patients. Intensive Care Med 29:2323–2326. doi:10.1007/s00134-003-1901-1
Rappaport VJ, Hirata G, Yap HK, Jordan SC (1990) Anti-vascular endothelial cell antibodies in severe preeclampsia. Am J Obstet Gynecol 162:138–146
Feekes JA, Cassell MD (2006) The vascular supply of the functional compartments of the human striatum. Brain 129:2189–2201. doi:10.1093/brain/awl158
Conflict of interest statement
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mueller-Mang, C., Mang, T., Pirker, A. et al. Posterior reversible encephalopathy syndrome: do predisposing risk factors make a difference in MRI appearance?. Neuroradiology 51, 373–383 (2009). https://doi.org/10.1007/s00234-009-0504-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-009-0504-0