Abstract
We report our experience in the endovascular treatment with detachable platinum coils of ruptured or symptomatic unruptured cerebral aneurysms in 61 patients aged 70–82 years. Complete occlusion was achieved in 38, subtotal in 17 and partial in one. The treatment failed in five patients. Clinical follow-up was performed in all patients for 8 months to 8 years. No bleeding occurred during the follow-up period. Outcome was favourable in 63% of the patients. When we compared the outcome of elderly patients with those of younger age endovascularly treated in the same period of time, we found a significantly higher frequency of poorer outcome in the elderly group (χ2=9.084; P=0.011). The frequency of favourable outcome in the elderly was significantly lower than in the younger group for H–H IV–V (χ2=9.299; P=0.010). The most important factor influencing the outcome was not age itself, but primary clinical condition on admission. The therapy of symptomatic aneurysms in elderly patients should not be purely conservative—a direct approach of the aneurysm should be considered. Endovascular treatment whenever possible seems to be a good alternative to surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Improvements in surgical techniques and intensive care, coupled with a progressive rise in the elderly population in Western countries, has led to a shift in the medical approach to elderly patients. Aggressive management of many conditions rather than purely conservative treatment is now more common, often with increasingly positive outcomes [1–8]. Indeed, endovascular techniques introduced in the early 1990s have changed the approach to treating subarachnoid aneurysms, allowing treatment of the malformation even in poor surgical candidates, such as some elderly patients [9–13]. In our department, we have experienced an increasingly aggressive approach to treating subarachnoid aneurysm in this group of patients in whom endovascular treatment has whenever possible become the treatment of choice. We report here our series of patients.
Methods
Three hundred and sixty-eight patients with subarachnoid aneurysms were treated by detachable platinum coils (GDC, Boston Scientific, Mass., USA) from 1994 to 2004 using the technique already described [14, 15]. In the early years, only poor surgical candidates (including elderly patients) were selected for endovascular treatment; however, more recently, the indications were expanded to include about 60% of patients. Sixty-one (18%) of the patients were between 70 and 82 years of age (mean 75, standard deviation 3), with a female predominance (female 45, male 16). Fifty-five patients presented with subarachnoid haemorrhage (SAH), with Hunt–Hess grades I–II in 20, III in 18 and IV–V in 17. Endovascular treatment was performed within 72 h from bleeding in 49 patients, while the remaining six were treated later due to poor clinical condition, which delayed admission to our department.
Four patients had isolated III nerve palsy, a further patient experienced visual disturbances and one patient had acute onset of headache.
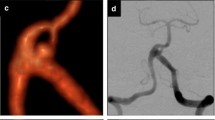
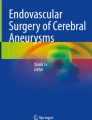
Twenty-one aneurysms were located on the anterior communicating artery, 19 on the carotid-posterior communicating artery, four on the carotid-ophthalmic segment, five on the middle cerebral artery and two on the carotid bifurcation. Twelve aneurysms were located on the posterior circulation (six basilar and six vertebral posterior-inferior cerebellar artery). Two patients had a double aneurysm of the basilar tip and of the posterior communicating artery, both treated in the same session. Fifty-one aneurysms were small (less than 1 cm) and 12 aneurysms were large.
The clinical outcome was evaluated following the criteria of Glasgow Outcome Scale (GOS): favourable outcome (good recovery = GOS 5 + moderate disability = GOS 4), severe disability (GOS 3) and poor outcome (vegetative state = GOS 2 + death = GOS 1).
Clinical follow-up was performed in all patients (8 years—8 months, mean 4.2 years) in our outpatients clinic or in some cases by telephone.
A statistical analysis with χ2 test was performed to compare the total frequency of outcome (favourable, severe disability and poor outcome) between the elderly group (70–82 years old) and the younger patients (20–70 years old) treated endovascularly in the same period of time.
Moreover, we statistically compared each single Hunt–Hess class frequency of outcome between the two age groups.
Results
Complete occlusion of the aneurysm was achieved in 38 patients (62%), subtotal (minimal filling between coils or neck remnant) in 17 (27%) and partial in one. In five cases, endovascular treatment failed. This was due to severe tortuosity of the internal carotid artery (two cases) or of vertebral artery (one case), while in an additional two cases coils could not be placed safely due to the unfavourable morphology of the aneurysm. Treatment-related complications occurred in three patients: in two this was due to ischaemia, with complete and incomplete recovery, respectively; and one patient had a minimal bleeding 3 weeks after incomplete coiling of a distal posterior inferior cerebellar artery ruptured aneurysm. The latter patient was acutely re-treated, obtaining a complete occlusion and resulting in complete recovery.
Overall outcome at clinical follow-up was favourable for 39 patients (63%), all of whom returned to normal life. Favourable outcome was positively related to the clinical condition at time of admission and was 100% for unruptured aneurysms, 90% for patients with HH grades I–II, 66% for HH grade III and 11% for HH grades IV–V (Table 1). Poor outcome and death were due to primary bleeding and systemic complications (infective, cardiovascular and pulmonary). After unsuccessful uncomplicated endovascular treatment, five patients required surgery, three had positive outcomes, while two died.
The comparison of clinical results between elderly (70–82 years) and younger patients (20–70 years) is reported in Tables 1, 2. A favourable outcome was found in 100% of patients without SAH; for grades HH I–II this was 90% in elderly and 96% in younger patients; for grade III, 66 and 87%, respectively; and for grades IV–V, 11 and 43%, respectively.
The statistical analysis showed that a worse outcome was significantly more frequent in elderly patients than in the younger group (χ2=9.084; P=0.011). Considering the Hunt–Hess I–III groups, no statistically significant differences were noted, whereas in H–H IV–V the elderly group had a significantly less favourable outcome than younger patients (χ2=9.299; P=0.010).
Discussion
In keeping with previous studies [3, 5, 16], we consider elderly patients to be those who are more than 70 years old. It may be reasonable to change not only this purely chronological definition of elderly, as well as medical attitudes towards elderly patients, given that there is a growing population of healthy elderly. Improvements in surgical techniques and neurointensive care now permit a more aggressive approach to the treatment of elderly patients with symptomatic aneurysms. Favourable outcomes have been reported previously for surgical series. Lan [5] found a favourable outcome in 57% of 44 patients older than 65 years of age. Similar results (57% of 157 elderly patients) have been reported by Johansson [4]. More recently, Ferch [17] reported favourable outcomes in 60% of over 70-year-old patients. In our series, favourable results were obtained in 63% of the patients. The clinical conditions present at admission represents the most relevant prognostic factor; in our series the majority of the patients in acceptable clinical conditions after SAH (HH I–III) or with unruptured aneurysms had favourable outcomes (37 out of 44), contrasting with patients with HH grades IV–V (two out of 17). This is in accordance with previous reports [3–5, 16–18].
The initial clinical condition is particularly important in elderly patients. Comparing the outcome of older and younger patients with the same clinical condition on admission, we found that elderly patients with grades HH I–II have a favourable outcome to younger patients. In contrast, a favourable outcome in elderly patients in poor clinical condition is much less common than in younger patients. Although previous reports have emphasised the importance of early treatment for patients in poor clinical condition [14, 15, 19, 20], the results of our series suggest that this may not apply to elderly patients [12].
Patients in good clinical condition following SAH are generally treated acutely. This study, in accordance with others [10], suggests that this should be extended also to elderly patients. Exclusion of the aneurysm allows more aggressive intensive care, both medical (triple-H) and eventually surgical (hydrocephalus). A further reason for early treatment is the increased risk of rebleeding reported in the elderly [5, 16, 21, 22], probably due to reduced elastic properties of the vessel wall and decreased responsiveness to factors responsible for spasm.
In keeping with previous studies [3, 16, 17, 23], we did not find a significant relationship between age and outcome: the clinical condition on admission rather than age is the major factor influencing the outcome.
The introduction of endovascular treatment with coils and the steady improvement of its techniques have changed the approach to cerebral aneurysms in many patients [23]. Endovascular treatment requires less brain manipulation, shorter stays in intensive care units, reduced risk of general complications and a more rapid return to a normal life—all aspects particularly relevant in elderly patients [11, 24, 25].
In addition to recent reports [1, 9, 11, 13], our study confirms that peri-procedural complications are not significantly different in younger and older patients, leading to outcomes that compare favourably with surgical series.
A critical point in the endovascular treatment is that the anatomical result may be incomplete or worsen after time. Given the lifespan of elderly patients, partial treatments (provided that they protect against early rebleeding and recanalisation), may be less relevant than in younger patients. Based on these considerations, we believe that it is reasonable to offer endovascular treatment as a first-line treatment for ruptured aneurysms in elderly patients. For unruptured aneurysms in contrast, although the risks of the endovascular treatment appear low even in the elderly, it is obvious that the reduced lifespan will also reduce the absolute rupture risk of the aneurysm rupture [26]. Hence, conservative treatment—meaning no treatment at all—must be primarily considered.
Conclusions
Therapy of symptomatic aneurysms in the elderly should no longer be purely conservative. Treatment of the aneurysm should be considered, since positive clinical results may be obtained in many cases with low risks. The most relevant factor influencing prognosis appears to be not the age, but the clinical condition at the time of admission. Endovascular approach represents the initial-choice of treatment in many cases.
References
Bakke SJ, Pedersen HK, Nome T, Sorteberg W, Lindegaard KF (2003) Outcome in individuals aged 70 years and more with ruptured intracranial aneurysms. Int Neuroradiol 9 [Suppl 2]:163
Fridriksson SM, Hillman J, Saveland H, Brandt L (1995) Intracranial aneurysm surgery in the 8th and 9th decades of life: impact on population-based management outcome. Neurosurgery 37:627–631
Inagawa T (1993) Management outcome in the elderly patient following subarachnoid hemorrhage. J Neurosurg 78:554–561
Johansson M, Cesarini KG, Contant CF, Persson L, Enblad P (2001) Changes in intervention and outcome in elderly patients with subarachnoid hemorrhage. Stroke 32:2845–2949
Lan Q, Ikeda H, Jimbo H, Izumiyama H, Matsumoto K (2000) Considerations on surgical treatment for elderly patients with intracranial aneurysms. Surg Neurol 53:231–238
O’Sullivan MG, Dorward N, Whittle IR, Steers AJ, Miller JD (1994) Management and long-term outcome following subarachnoid haemorrhage and intracranial aneurysm surgery in elderly patients: an audit of 199 consecutive cases. Br J Neurosurg 8:23–30
Rosenorn J, Eskesen V, Schmidt K (1987) Age as a prognostic factor after intracranial aneurysm rupture. Br J Neurosurg 1:335–341
Takeuchi J (1993) Aneurysm surgery in patients over the age of 80 years. Br J Neurosurg 7:307–309
Birchall D, Khangure M, McAuliffe W, Apsimon H, Knuckey N (2001) Endovascular management of acute subarachnoid haemorrhage in the elderly. Br J Neurosurg 15:35–38
Jain R, Deveikis J, Thompson BG (2004) Endovascular management of poor-grade aneurysmal subarachnoid hemorrhage in the geriatric population. AJNR Am J Neuroradiol 25:596–600
Johansson M, Norback O, Gal G, Cesarini KG, Tovi M, Solander S, Contant CF, Ronne-Engstrom E, Enblad P (2004) Clinical outcome after endovascular coil embolization in elderly patients with subarachnoid hemorrhage. Neuroradiology 46:385–391
Lubicz B, Leclerc X, Gauvrit JY, Lejeune JP, Pruvo JP (2004) Endovascular treatment of ruptured intracranial aneurysms in elderly people. AJNR Am J Neuroradiol 25:592–595
Sedat J, Dib M, Lonjon M, Litrico S, Von Langsdorf D, Fontaine D, Paquis P (2002) Endovascular treatment of ruptured intracranial aneurysms in patients aged 65 years and older: follow-up of 52 patients after 1 year. Stroke 33:2620–2625
Bergui M, Bradac GB (2004) Acute endovascular treatment of ruptured aneurysms in poor-grade patients. Neuroradiology 46:161–164
Bradac GB, Bergui M, Stura G, Fontanella M (2003) Acute endovascular treatment of ruptured aneurysms in poor grade patients. Riv Neuroradiol 16:1211–1212
Yano S, Hamada J, Kai Y, Todaka T, Hara T, Mizuno T, Morioka M, Ushio Y (2003) Surgical indications to maintain quality of life in elderly patients with ruptured intracranial aneurysms. Neurosurgery 52:1010–1015
Ferch R, Pasqualin A, Barone G, Pinna G, Bricolo A (2003) Surgical management of ruptured aneurysms in the eighth and ninth decades. Acta Neurochir 145:439–445
Vega-Basulto SD, Silva-Adan S, Mosquera-Betancourt G, Varela-Hernandez A (2002) Aneurysms surgery in the patients aged seventy to eighty years. Neurocirugia 13:371–377
Bracard S, Lebedinsky A, Anxionnat R, Neto JM, Audibert G, Long Y, Picard L (2002) Endovascular treatment of Hunt and Hess grades IV and V aneurysms. AJNR Am J Neuroradiol 23:953–957
Le Roux PD, Winn HR (1999) Intracranial aneurysms and subarachnoid hemorrhage management of the poor grade patient. Acta Neurochir Suppl 72:7–26
Lanzino G, Kassell NF, Germanson TP, Kongable GL, Truskowski LL, Torner JC, Jane JA (1996) Age and outcome after aneurysmal subarachnoid hemorrhage: why do older patients fare worse? J Neurosurg 85:410–418
Vogel T, Verreault R, Turcotte JF, Kiesmann M, Berthel M (2003) Intracerebral aneurysms: a review with special attention to geriatric aspects. J Gerontol A Biol Sci Med Sci 58:520–524
Molyneux A, Kerr R, Stratton I, Sandercock P, Clarke M, Shrimpton J, Holman R, International Subarachnoid Aneurysm Trial (ISAT) (2002) Collaborative Group International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet 360:1267–1274
Barker FG 2nd, Amin-Hanjani S, Butler WE, Hoh BL, Rabinov JD, Pryor JC, Ogilvy CS, Carter BS (2004) Age-dependent differences in short-term outcome after surgical or endovascular treatment of unruptured intracranial aneurysms in the United States, 1996–2000. Neurosurgery 54:18–28
Sugiyama K, Ueno J, Fujita S, Naito H, Hirota N, Kin H, Karasawa H, Ohkubo Y (2003) Treatment of ruptured cerebral aneurysms in the elderly. Riv Neuroradiol 16:1241–1244
ISUIA, Wiebers DO, Whisnant JP, Huston J 3rd, Meissner I, Brown RD Jr, Piepgras DG, Forbes GS, Thielen K, Nichols D, O’Fallon WM, Peacock J, Jaeger L, Kassell NF, Kongable-Beckman GL, Torner JC (2003) Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet 362:103–110
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bradač, G., Bergui, M. & Fontanella, M. Endovascular treatment of cerebral aneurysms in elderly patients. Neuroradiology 47, 938–941 (2005). https://doi.org/10.1007/s00234-005-1444-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-005-1444-y