Abstract
Subarachnoid hemorrhage (SAH) is not an unusual disease in an elderly population. The clinical outcome has improved over time. It has been suggested that elderly SAH patients would benefit from endovascular aneurysm treatment. The aim of this study was to evaluate technical results and clinical outcome in a series of elderly SAH-patients treated with endovascular coil embolization. Sixty-two patients (≥ 65 years) presenting with aneurysmal SAH underwent early endovascular coil embolization at Uppsala University Hospital between September 1996 and December 2000. In all 62 cases included in the study, endovascular coil embolization was considered the first line of treatment. Admission variables, specific information on technical success, degree of occlusion and procedural complications, and outcome figures were recorded. Clinical grade on admission was Hunt and Hess (H&H) I–II in 39%, H&H III in 27% and H&H IV–V in 34% of the patients. The proportion of posterior circulation aneurysms was 24%. Coil embolization was successfully completed in 94%. The degree of occlusion of the treated aneurysm was complete occlusion in 56%, neck remnant in 21%, residual filling in 11%, other remnant in 5% and not treated in 6%. The rate of procedural complications was 11%. Outcome after 6 months was favorable in 41%, severe disability in 36% and poor in 22%. Favorable outcome was achieved in 57% of the H&H I–II patients, 47% of the H&H III patients and 17% of the H&H IV–V patients. Endovascular aneurysm treatment can be performed in elderly patients with SAH with a high level of technical success, acceptable aneurysm occlusion results, an acceptable rate of procedural complications and fair outcome results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Subarachnoid hemorrhage (SAH) from a ruptured cerebral aneurysm is not an unusual disease in old age, and the proportion of elderly patients in the population is substantial and increasing. We have previously demonstrated how changes in referral patterns and more active management of elderly patients with SAH improve outcome even in these patients [1], who for many years were excluded from active treatment and aneurysm repair because of their advanced age alone.
Since the appearance of the Guglielmi detachable coils (GDC) in 1990 [2], the technical advances in this field have been tremendous, and the use of endovascular aneurysm treatment is increasing. It has been suggested that elderly SAH-patients would benefit from endovascular aneurysm treatment, since it is less invasive than craniotomy and should thus inflict less secondary injury to the vulnerable aged brain [3, 4]. Two studies with a small number of patients aged 70 years or older have shown favorable results [5, 6]. Good outcome was reported in one study comparing patients 65 years or older with younger patients [7]. Recently, the results of the first large multicenter randomized study—The International Subarachnoid Aneurysm Trial (ISAT)—showed significantly better outcome overall after endovascular treatment compared with surgery [8]. The results of endovascular aneurysm treatment in elderly patients in particular remain to be evaluated in a large series of patients.
At the Uppsala Neurovascular Center, endovascular coil embolization was introduced in September 1996. A team of vascular neurosurgeons and interventional neuroradiologists collaborate closely in deciding which treatment is feasible for each ruptured aneurysm. The ambition is to treat the patient at an early stage, irrespective of age and neurological state. Regardless of aneurysm repair strategy, all patients are treated according to the same protocols for neurointensive care treatment of SAH [9].
The aim of this study was to investigate how elderly patients tolerate and benefit from aneurysm treatment with endovascular coil embolization after SAH. Specific aims were to evaluate clinical outcome at 6 months after aneurysm rupture, as well as the frequency of procedural complications and the degree of occlusion of the target aneurysm at the time of intervention.
Materials and methods
The selection criteria for this study were: (1) spontaneous SAH between September 1996 and December 2000, (2) age 65 years or older at time of SAH, (3) aneurysm rupture as the cause of SAH, (4) endovascular aneurysm treatment chosen as the first line of treatment, and (5) that aneurysm repair treatment was given at the acute stage after hemorrhage (within 3 weeks of aneurysm rupture)[10]. The diagnosis of ruptured aneurysm was made with cerebral panangiography. All patients were managed according to modern neurointensive care principles [9]. A vascular neurosurgeon and an interventional neuroradiologist made the selection of patients for endovascular coil embolization. The location and configuration of the aneurysm and the patient’s clinical condition affected the choice of treatment. If it was judged that both endovascular and neurosurgical aneurysm treatment was feasible, endovascular coil embolization was the preferred treatment.
Patient characteristics, such as sex, age, time of SAH, time of admission, neurological grade according to Hunt and Hess [11] (H&H) and Fisher grade [12] were collected from the neurovascular database established at the neurointensive care unit.
Procedural reports from all GDC-treated aneurysms during the specified time were reviewed for information about lesion(s) treated, technical success, time of aneurysm repair, angiographic degree of occlusion and procedural complications. The angiographic degree of occlusion was based on the final angiogram during the embolization procedure and categorized into five groups on the basis of the location of the possible remnant: complete occlusion, neck remnant, residual filling, other remnant and not treated. The term “neck remnant” was used when the neck of the aneurysm could not be packed with coils, and “residual filling” refers to the aneurysm not being densely packed. “Other remnant” refers to an aneurysm remnant that could not be otherwise classified.
Procedural complications during endovascular treatment were registered as aneurysm rupture, unintentional parent artery occlusion, other artery occlusion due to thrombo-embolism, coil migration and intraluminal coil protrusion. The use of thrombolytic agents, intra-arterial papaverin injection and angioplasty during the treatment procedure was also recorded, as well as the use of a protective balloon when coiling wide-necked aneurysms with the re-modeling technique [13].
Data on clinical outcome at 6 months after SAH were obtained from written structured interviews with the patients or their close relatives, and classified according to the Glasgow Outcome Scale (GOS) [14].
In the statistical analyses GOS scores were grouped as favorable (good recovery and moderate disability), severe disability or poor (vegetative state or dead).
The Pearson χ2-test was used in the univariate analyses. All variables were categorical in the univariate analyses. A p value less than 0.05 was considered statistically significant.
A multivariate logistic regression model was fitted with favorable outcome as the dependent variable. The initial model fit contained admission variables (H&H grade, age and Fisher score) and treatment variables (use of ventriculostomy, treatment day, aneurysm location and occurrence of any procedural complication) as explanatory variables. All variables were categorical except age and treatment day, which were continuous. Variables were removed in a backward elimination manner based on the p value. The final model included admission and treatment variables that were considered statistically significant (p<0.05) or marginally significant (0.05<p<0.10). All statistical analyses were conducted using commercially available software [StatSoft (2001) STATISTICA (data analysis software system), version 6. www.statsoft.com].
Results
Sixty-two patients (16 male, 46 female) fulfilled the inclusion criteria of this investigation. During the same period, 166 elderly patients (≥ 65 years) were admitted with SAH; 138 were investigated with cerebral panangiography, which demonstrated an aneurysmal origin in 111 cases. Eleven patients with ruptured aneurysms were treated conservatively, 37 received surgical aneurysm treatment, and 1 was initially treated conservatively and embolized 50 days after the SAH. Characteristics of the study patients are summarized in Table 1. The mean age was 71.5 years (range 65–81 years). The mean day of admission was 1.4 days after clinical presentation (range 0―14 days). Twenty-four patients (39%) were in good neurological condition (H&H I–II) on admission, 17 (27%) were drowsy or confused (H&H III) and 21 (34%) were in poor neurological condition (H&H IV–V). The amount of subarachnoid blood on the diagnostic CT according to Fisher’s scale was grade 1 in 3 patients (5%), grade 2 in 6 (10%), grade 3 in 18 (29%) and grade 4 in 35 (56%). Thirty-two patients (52%) had intraventricular hemorrhage (IVH), and 10 (16%) had intracerebral hematoma (ICH) in addition to the SAH (Table 1). The distribution of ruptured aneurysms was 47 (76%) in the anterior circulation and 15 (24%) in the posterior circulation (Table 2).
Coil embolization of the target aneurysm was completed in 58 (94%) of 62 patients. The endovascular procedures were carried out by three interventional neuroradiologists (G.G., 50 patients; S.S., 10; M.T., 2) In 6 patients, additional non-ruptured aneurysms were also embolized during the same procedure (3 MCA, 1 SCA, 1 ICA, 1 AComA). In three cases, the target aneurysm was not successfully catheterized and, in 1 case, the target aneurysm anatomy was re-evaluated during the procedure and found unsuitable for endovascular treatment and the procedures were discontinued (Table 2, Table 3). These 4 patients later underwent surgical aneurysm repair and were not included in the outcome analysis (Table 4).
The endovascular procedure was performed within 3 days after aneurysm rupture in 44 patients (71%), on days 4 to 10 in 13 patients (21%) and later than 10 days after aneurysm rupture in 5 patients (8%) (mean 3.6 days, range 1–18 days) (Table 3). The angiographic degree of occlusion of the target aneurysm is shown in Table 3. Seven procedural complications were noted (Table 3). During 11 procedures, the re-modeling technique with a protective balloon was used, and in 1 patient an intraluminal stent was placed in the vertebral artery before coiling of a PICA aneurysm. In 1 patient with thrombo-embolism and artery occlusion during the treatment procedure, an intra-arterial thrombolytic agent was used. Intra-arterial papaverin injections were used in 2 patients in whom vasospasm was encountered during the treatment procedure.
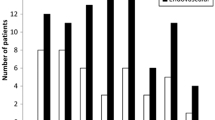
Overall outcome 6 months after the SAH was good recovery in 21 patients (36%), moderate disability in 3 (5%), severe disability in 21 (36%) and death in 13 (22%). None remained in a persistent vegetative state. Clinical outcome in relation to Hunt and Hess grade on admission, age, Fisher grade, intraventricular hemorrhage, intracerebral hematoma, use of ventriculostomy, day of treatment, aneurysm location and occurrence of any procedural complication is outlined in Table 4.
In the univariate analysis, the patients with a good clinical grade on admission (H&H I–II) had better outcomes than the patients with a poor clinical grade on admission did (H&H IV–V) (Table 4; p<0.05). The patients who were treated for aneurysms in the ICA–PComA territory had more favorable outcomes and less severe disabilities than the patients treated for aneurysms in the A1–AComA–A2 territory (Table 4; p<0.01). There was a trend toward worse outcome in patients with Fisher grade 3 and 4 and in patients with MCA aneurysms. Also, there was a trend toward better outcome in patients who suffered from a procedural complication and in patients who were treated at a later stage after the SAH. However, these numerical differences were not statistically significant. There was no observed difference in outcome depending on age, or presence of IVH or ICH.
The results of the final multivariate logistic regression analysis are shown in Table 5. A Fisher grade of 1 or 2 on diagnostic CT was associated with a greater probability of a favorable outcome (p=0.021). The later the treatment day, the greater was the chance of having a favorable outcome (p=0.060). This finding was, however, only marginally significant.
Discussion
In our previous study of elderly patients with SAH treated between 1981 and 1998, we demonstrated a gradual change toward more active treatment and improved outcome in conjunction with the introduction of neurointensive care [1]. Shortly after endovascular therapy was established as a routine therapy at our center, it became the first line of treatment for aneurysm repair. A particularly quick change in treatment policy occurred for elderly SAH patients after reports of successful endovascular treatment [5] with less surgical trauma. It was desirable to evaluate the tolerance and benefit of endovascular aneurysm treatment specifically in elderly SAH patients. In this paper we report a series of 62 elderly patients treated endovascularly for ruptured intracranial aneurysms during the first 4 years when this treatment modality was the first line of treatment. During this period, neurosurgical aneurysm treatment was preferred in only one third of the elderly patients (37/111). Endovascular coil embolization of a ruptured aneurysm was successfully completed as intended in 58 of 62 elderly patients. Only 4 procedures (6%) were terminated because of technical inaccessibility.
In our material, slightly over half (56%) of the target aneurysms were completely occluded on the end-procedural angiogram. Neck remnants were present in 20% of cases and 11% were not densely packed, which may seem disappointing. In the literature, the degree of aneurysm occlusion is reported using a variety of descriptions, which makes comparison with other series difficult; nonetheless, the frequency of complete occlusion is often reported. In a systematic review by Brilstra and co-workers aneurysm occlusion rates are reported for 509 patients of all ages with ruptured aneurysms; 51.9% of the embolized aneurysms were completely occluded [15]. In a recent randomized study comparing endovascular and neurosurgical treatment of ruptured intracranial aneurysms by Vanninen and colleagues [16], 50% total obliteration, 35% neck remnants and 6% residual filling of the aneurysm fundus were reported for 52 patients in the endovascularly treated group. Birchall and colleagues reported 46.6% complete occlusion in a study of 14 patients aged 70 years or older [6]. Sedat and co-workers reported 48.5% complete occlusion in 52 elderly patients [7]. Friedman and colleagues reported complete occlusion in 33% at time of treatment in 83 patients [17]. The main reason for partial occlusion in our material is probably that the goal in this age group was to prevent the ruptured aneurysm from re-bleeding without running too great a risk of procedural complications such as unintentional artery occlusion. It is reasonable to believe that a partly occluded aneurysm may be sufficient and satisfactory for the remainder of a patient’s expected lifespan, but a small sequela may substantially decrease the quality of life in this age group.
We found a procedural complication rate of 11%, most of which were potentially serious complications, such as aneurysm rupture, parent vessel occlusion and occlusion of other vessels due to thrombo-embolism. However, there was no increased morbidity or mortality related to procedural complications. Of the 7 patients who had a procedural complication, 1 suffered a poor outcome and 5 enjoyed a favorable outcome. Procedural complication frequencies of this order have been reported before by other groups in patients of all ages [10, 15, 17, 18, 19] and in elderly patients [6, 7]. It is generally accepted that the seriousness of a disease determines the level of risk involved with the treatment that is considered acceptable. The natural course of SAH is truly grim, with a high risk of fatal re-bleeding and delayed neurological deterioration due to vasospasm. Occlusion of the ruptured aneurysm is crucial for the further management of the patient, so an 11% risk of a procedural complication in treating high-risk elderly patients with this devastating disease may therefore be considered acceptable.
In the crude outcome analysis, 41% of the patients had a favorable outcome. The SAH mortality at 6 months was only 22%. However, 36% of all patients were severely disabled at 6 months after SAH. These outcome figures are comparable to those reported before by Sedat and colleagues [7]. In their material, of 52 endovascularly treated patients 65 years or older 48% had favorable outcome (GOS 1–2), 27% were severely disabled (GOS 3) and the mortality rate (GOS 5) was 23% at 1 year after the SAH. However, their material included a greater proportion of good-grade patients and a greater proportion of patients with a low Fisher grade. The outcome in this series compares favorably with a large multicenter study of surgically treated patients [20]. In the International Co-operative Study on the Timing of Aneurysm Surgery [20], surgically treated patients aged 70 years or older outcome was 45% favorable (GOS 1–2), 16% severe disability (GOS 3) and 39% poor (GOS 4 – 5) outcome.
The aneurysm location seems to be an important determining factor for clinical outcome. In spite of small numbers, differences in outcome depending on aneurysm location were seen; however, any interpretation should be made with caution. The highest proportion of favorable outcomes and lowest proportion of severe disabilities were seen in patients with ICA and PComA aneurysms, whereas the most severe disability was seen in patients with aneurysms on the anterior cerebral artery and anterior communicating artery. Half of the patients (3/6) with an MCA aneurysm had a poor outcome and only one enjoyed a favorable outcome, which could imply that the endovascular aneurysm treatment of MCA aneurysms is associated with higher risks. This may be due to the commonly encountered configuration of multiple branches arising adjacent to the aneurysm neck [21, 22]. Careful selection of suitable MCA aneurysms for endovascular treatment is fundamental for good results.
There was a trend toward better outcome in patients with a low Fisher grade and in patients treated on days 4–10 or more than 10 days after SAH. This is also illustrated in the multivariate logistic regression analysis, where a later day of treatment was associated with favorable outcome; however, this was not statistically significant (p=0.060). This may reflect the fact that the patients who underwent endovascular coil embolization at a later stage after the SAH were subjected to a selection process, in which only patients retaining a good clinical grade at this stage were considered for treatment. The optimal timing of endovascular coil embolization of ruptured aneurysms in the elderly requires further investigation in larger series. However, it is notable that as many as 40% of patients treated before and during the “vasospasm phase” had a favorable outcome.
Comparing the results of the present series with those between 1987 and 1992 in our previous study on elderly SAH patients [1], it would appear that the introduction of endovascular aneurysm repair as the first line of treatment of ruptured aneurysms after SAH has reduced the mortality from 26% to 22%, but increased the proportion of severe disability from 11% to 36% and decreased the proportion of favorable outcome from 61% to 41%. However, a simple comparison between the functional outcome of this series of endovascularly treated elderly patients with the earlier series of elderly SAH patients is problematic for several reasons. The basic characteristics of the patients in this study are nearly consistent with those reported earlier between 1987 and 1992 in our previous study [1] (previous results in parentheses): women 74% (74%), admission within 48 h 79% (73%), percentage of good-grade patients, H&H I–II 39% (43%), Fisher grade 3–4 85% (82%) and use of ventriculostomy 56% (50%). However, there was a lower percentage of drowsy patients [H&H III 27% (38%)] and a higher percentage of patients in a poor clinical grade on admission [H&H IV–V 34% (18%)] in this series. More patients were aged 70 years or older in this series: 65% (27%). There was a higher proportion of posterior circulation aneurysms (24%) compared with our earlier study (9%), which is probably due to the better availability of endovascular treatment in this region. There is also a possibility that patients with more coexistent diseases were selected for treatment in the present series, which may have influenced the outcome negatively. Furthermore, the follow-up period was longer in the earlier study which may have contributed to a lower percentage of severely disabled patients and larger proportions of dead patients and patients achieving a favorable outcome. If the results of this series are viewed against this background, the outcomes of this series may be considered fair. A comparison between neurosurgical and endovascular aneurysm treatment in elderly patients was beyond the scope of this investigation, but may be done in a randomized study.
Conclusions
Endovascular aneurysm treatment can be performed in elderly patients with SAH with a high level of technical success, with acceptable aneurysm occlusion results, with an acceptable rate of procedural complications and with fair outcome results. Middle cerebral artery aneurysms may be less suitable for endovascular coil embolization in elderly patients. There was no clear evidence that early endovascular coil embolization should be avoided. The recently completed International Subarachnoid Aneurysm Trial [8] may contribute with further information on endovascular coil embolization in elderly SAH patients.
References
Johansson M, Cesarini KG, Contant CF, Persson L, Enblad P (2001) Changes in intervention and outcome in elderly patients with subarachnoid hemorrhage. Stroke 32:2845–2949
Guglielmi G, Vinuela F, Dion J, Duckwiler G (1991) Electrothrombosis of saccular aneurysms via endovascular approach. 2. Preliminary clinical experience. J Neurosurg 75:8–14
Ausman JI (1997) The future of neurovascular surgery. I. Intracranial aneurysms. Surg Neurol 48:98–100
Molyneux A, Kerr R (1999) International Subarachnoid Aneurysm Trial. J Neurosurg 91:352–353
Rowe JG, Molyneux AJ, Byrne JV, Renowden S, Aziz TZ (1996) Endovascular treatment of intracranial aneurysms: a minimally invasive approach with advantages for elderly patients. Age Ageing 25:372–376
Birchall D, Khangure M, McAuliffe W, Apsimon H, Knuckey N (2001) Endovascular management of acute subarachnoid haemorrhage in the elderly. Br J Neurosurg 15:35–38
Sedat J, Dib M, Lonjon M, Litrico S, Von Langsdorf D, Fontaine D, Paquis P (2002) Endovascular treatment of ruptured intracranial aneurysms in patients aged 65 years and older: follow-up of 52 patients after 1 year. Stroke 33:2620–2625
Molyneux A (2002) International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2,143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet 360:1267–1274
Persson L, Enblad P (1999) Neurointensive care of aneurysmal SAH. Acta Neurochir Suppl (Wien) 72:73–80
Byrne JV, Molyneux AJ, Brennan RP, Renowden SA (1995) Embolisation of recently ruptured intracranial aneurysms. J Neurol Neurosurg Psychiatry 59:616–620
Hunt W, Hess R (1968) Surgical risk as related to time of intervention in the repair of intracranial aneurysms. J Neurosurg 28:14–20
Fisher C, Kistler J, Davis J (1980) Relation of cerebral vasospasm to subarachnoid hemorrhage visualized by computerized tomographic scanning. Neurosurgery 6:1–9
Moret J, Cognard C, Weill A, Castaings L, Rey A (1997) The “remodelling technique” in the treatment of wide neck intracranial aneurysms. Angiographic results and clinical follow-up in 56 cases. Intervent Neuroradiol 3:21–35
Jennett B, Bond M (1975) Assessment of outcome after severe brain damage. Lancet i:480–484
Brilstra EH, Rinkel GJ, van der Graaf Y, van Rooij WJ, Algra A (1999) Treatment of intracranial aneurysms by embolization with coils: a systematic review. Stroke 30:470–476
Vanninen R, Koivisto T, Saari T, Hernesniemi J, Vapalahti M (1999) Ruptured intracranial aneurysms: acute endovascular treatment with electrolytically detachable coils—a prospective randomized study. Radiology 211:325–336
Friedman JA, Nichols DA, Meyer FB, Pichelmann MA, McIver JI, Toussaint LG, 3rd, Axley PL, Brown RD, Jr. (2003) Guglielmi detachable coil treatment of ruptured saccular cerebral aneurysms: retrospective review of a 10-year single-center experience. AJNR Am J Neuroradiol 24:526–533
Baltsavias GS, Byrne JV, Halsey J, Coley SC, Sohn MJ, Molyneux AJ (2000) Effects of timing of coil embolization after aneurysmal subarachnoid hemorrhage on procedural morbidity and outcomes. Neurosurgery 47:1320–1329; discussion 1329–1331
Casasco AE, Aymard A, Gobin P, Houdart E, Rogopoulos A, George B, Hodes J, Cophignon J, Merland J-J (1993) Selective endovascular treatment of 71 intracranial aneurysms with platinum coils. J Neurosurg 79:3–10
Kassell N, Torner J, Haley EJ, Jane J, Adams H, Kongable G (1990) The International Cooperative Study on the Timing of Aneurysm Surgery. 1. Overall management results. J Neurosurg 73:18–36
Debrun GM, Aletich VA, Kehrli P, Misra M, Ausman JI, Charbel F (1998) Selection of cerebral aneurysms for treatment using Guglielmi detachable coils: the preliminary University of Illinois at Chicago experience. Neurosurgery 43:1281–1295; discussion 1296–1287
Raftopoulos C, Mathurin P, Boscherini D, Billa RF, Van Boven M, Hantson P (2000) Prospective analysis of aneurysm treatment in a series of 103 consecutive patients when endovascular embolization is considered the first option. J Neurosurg 93:175–182
Acknowledgements
We thank Prof. Lennart Persson, Head of the Department of Clinical Neurosciences, for his groundbreaking work and for supporting the establishment of interventional neuroradiology in Uppsala. This study was supported by The Swedish Research Council (2002/ A0799).
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was approved by the local research ethics committee in Uppsala, Sweden (Ups Dnr 01–104)
Rights and permissions
About this article
Cite this article
Johansson, M., Norbäck, O., Gál, G. et al. Clinical outcome after endovascular coil embolization in elderly patients with subarachnoid hemorrhage. Neuroradiology 46, 385–391 (2004). https://doi.org/10.1007/s00234-004-1170-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-004-1170-x