Abstract
Atypical teratoid/ rhabdoid tumor (AT/RT) of the central nervous system is a rare, highly aggressive malignancy of infancy. Although it is reported infrequently in the literature, it has often been histologically confused with a primitive neuroectodermal tumor (PNET)/medulloblastoma (MB) but has a much worse prognosis. We present an infant with two AT/RT tumors, one suprasellar in location and the other within the vermis without evidence of tumor elsewhere. What makes this case unusual is that there were two separate lesions in different cranial compartments, with no evidence of subarachnoid seeding. In addition, the lesions had different magnetic resonance imaging (MRI) characteristics even though they were histologically the same.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
AT/RT is an aggressive, almost uniformly fatal tumor occurring mostly in children less than 2 years old with a median survival of 6–11 months [1]. Because it is a relatively rare pathological entity, it is frequently misdiagnosed as a PNET/MB. However, distinguishing these tumor types is of clinical significance because AT/RTs have been found to respond poorly to treatment regimens utilized for childhood PNETs [1]. This case report illustrates an unusual presentation of AT/RT in which the patient is found to have tumor in both the supratentorial and infratentorial compartments, without evidence of seeding, with similar histology but different radiographic findings.
Case summary
The patient was a previously-healthy 3-month-old girl who presented with a three-day history of vomiting and abnormal eye movements. On initial examination she was sleepy but arousable, with bilateral disconjugate gaze palsies. She moved all her extremities symmetrically although tone was mildly increased.
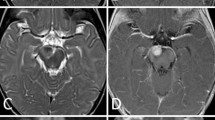
An initial CT of the head revealed solid suprasellar as well as vermian masses, with prominent hydrocephalus and acute bilateral occipital intraventricular hemorrhage. No hemorrhage was noted within either tumor. A ventriculostomy was emergently placed, whereupon the patient’s level of alertness improved. Axial MRI scans demonstrated a brightly-enhancing 1.6 cm×1.3 cm×1.2 cm suprasellar mass (Fig. 1) and a 2.0 cm×1.6 cm×1.7 cm minimally-enhancing vermian mass (Fig. 2) with acute blood in the occipital ventricles and cisterna magna. Sagittal T1-weighted MRI with gadolinium (Fig. 3) showed both suprasellar and vermian masses; the former markedly enhances, while the latter minimally enhances.
The patient underwent a posterior fossa craniotomy with complete resection of the vermian lesion, as confirmed by a post-operative MRI study of the head and spine showing no residual tumor in the vermis and no evidence of tumor elsewhere, other than in the suprasellar mass. Histological examination confirmed the diagnosis of AT/RT. As the vermian lesion was completely resected, and there was no evidence of diffuse spread of tumor, it was reasoned that the infant’s prognosis would be improved by resection of the second and separate tumor. This was performed through a pterional approach. This tumor was also found to be an AT/RT. The post-operative MRI confirmed the complete resection of both tumors.
The patient required the placement of a ventriculoperitoneal shunt three weeks after surgery. Interestingly, post-operative CSF cytology was negative for malignant cells. The patient was then started on an intensive chemotherapy regimen that first included the modified Head Start protocol (cisplatin, etopside, vincristine, cytoxan, high dose methotrexate) followed by ICE (ifosphamide, carboplatin, etopside) therapy. However, despite the aggressive treatment, the patient died 9 months after surgery from tumor recurrence.
Discussion
AT/RT of the CNS was first described as a unique entity in 1987 and since then cases have been reported infrequently in the literature [2]. In the most recent WHO brain-tumor classification, this tumor type comprises 6.7% of pediatric brain tumors in the 0–2 years group and 1.3% of tumors in the 0–17 years group [3]. However, they are often radiographically and histologically confused with PNET/MB, and the true frequency is probably underestimated [4].
In a large review of this tumor entity, 63% of cases were infratentorial, 27% were supratentorial, 8% presented with multiple lesions, and 2% were within the extramedullary cervical spinal cord [5]. Of the cases with multiple lesions, none presented with involvement of both the infratentorial and supratentorial compartments, as is the case in this report. Additionally, AT/RTs have a propensity for seeding the CSF pathways. One-third of cases presented in the review by Rorke et al. documented cytological evidence of CSF seeding. In the case presented here, however, CSF cytology was negative for malignant cells, suggesting that both tumors developed independently.
AT/RTs always contain a population of rhabdoid cells with varying amounts of primitive neuroectodermal, mesenchymal, and epithelial cells. Macroscopically, they appear as a soft, pinkish, often bulky mass containing regions of necrosis and/or hemorrhage. AT/RTs can only be reliably differentiated by employing immunohistochemistry, staining most commonly with vimentin, epithelial membrane antigen, glial fibrillary acidic protein, and smooth-muscle actin [4]. The histological distinction is crucial, since historically it has been shown to have a very poor response to multimodal therapies employed for childhood PNET.
Radiographically, AT/RTs appear very similar to PNETs. With CT, they present as a region of increased density that heterogeneously enhances with contrast, and can have both cystic and hemorrhagic components. With MRI, these tumors typically are hypointense on T1-weighted sequences but brightly enhance with the administration of gadolinium (0.1 mmol/kg). On T2-weighted sequences they are most commonly hypo- to isointense. The suprasellar mass in this particular case is the typical presentation (Figs. 1 and 3). However, the vermian mass has very different radiographic characteristics, with minimal contrast enhancement, even though the pathologies of both the lesions were the same (Figs. 2 and 3). The reason for this difference is not clear. In cases where CSF dissemination can be documented, tumors that seed can have different contrast-enhancement patterns for a period of time. However, this is unlikely to be the explanation in this case, since CSF cytology was negative. Another possible reason may be differing amounts of the various constituent tissues or necrosis within the tumor. This radiographic variation may be clinically relevant when considering the differential diagnosis on preoperative imaging.
Conclusion
AT/RT is a relatively new tumor entity that carries a very poor prognosis and is often misdiagnosed and mistreated as PNET. Because of its propensity for CSF dissemination, tumors at multiple sites have been reported. However, as our case demonstrates, there can be radiographic variations with similar histological presentations, as well as multiple intracranial tumor sites without evidence of CSF seeding.
References
Hilden JM, Watterson J, Longee DC, Moertel CL, Dunn ME, Kurtzberg J, Scheithauer BW (1998) Central nervous system atypical teratoid tumor/rhabdoid tumor: Responses to intensive therapy and review of literature. J Neurooncol 40:265–275
Lefkowitz IB, Rorke LB, Packer RJ, Sutton LN, Katnick RJ (1987) Atypical teratoid tumor of infancy: definition of an entity. Ann Neurol 22:214–222
Rickert CH, Paulus W (2001) Epidemiology of childhood nervous system tumors in childhood and adolescence based on the new WHO classification. Childs Nerv Syst 17:503–511
Burger PC, Yu I-T, Tihan T, Freidman HS, Strother DR, Kepner JL, Duffner PK, Kun LE, Perlamn EJ (1998) Atypical teratoid/rhabdoid tumor of the central nervous system. A highly malignant tumor of infancy and childhood frequently mistaken for medulloblastoma. A pediatric oncology group study. Am J Surg Pathol 28:1083–1092
Rorke LP, Packer RJ, Biegel J (1996) Central nervous system atypical teratoid/rhabdoid tumors of infancy and childhood: Definition of an entity. J Neurosurg 85:56–65
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gandhi, C.D., Krieger, M.D. & McComb, J.G. Atypical teratoid/rhabdoid tumor: an unusual presentation. Neuroradiology 46, 834–837 (2004). https://doi.org/10.1007/s00234-004-1251-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-004-1251-x