Abstract
Purpose
A meta-analysis was performed to evaluate the correlation between single-nucleotide polymorphisms (SNPs) and risk of statin-induced myopathy (SIM).
Methods
We retrieved the studies published on SIM until April 2019 from the PubMed, Embase, and Cochrane Library databases. We collected data from 32 studies that analyzed 10 SNPs in five genes and included 21,692 individuals and nine statins.
Results
The analysis of the heterozygous (p = 0.017), homozygous (p = 0.002), dominant (p = 0.005), and recessive models (p = 0.009) of SLCO1B1 rs4149056 showed that this SNP increases the risk of SIM. Conversely, heterozygous (p = 0.048) and dominant models (p = 0.030) of SLCO1B1 rs4363657 demonstrated that this SNP is associated with a reduced risk of SIM. Moreover, an increased risk of SIM was predicted for carriers of the rs4149056 C allele among simvastatin-treated patients, whereas carriers of the GATM rs9806699 A allele among rosuvastatin-treated patients had a lower risk of SIM.
Conclusion
The meta-analysis revealed that the rs4149056 and rs4363657 SNPs in SLCO1B1 and the rs9806699 SNP in GATM are correlated with the risk of SIM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Statins act as inhibitors of the enzyme 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase, thereby competitively inhibiting the synthesis of endogenous cholesterol. Although modern proprotein convertase subtilisin/kexin type 9 (PCSK9) serine protease inhibitors can also be used to lower serum lipid levels, statins are still widely used in clinical treatment, since they are well-tolerated and improve the condition of patients with cardiovascular disease [1]. However, the prolonged use of statins may result in statin-induced myopathy (SIM), myalgia, and life-threatening rhabdomyolysis. The clinical manifestations of SIM include acute or chronic muscle pain, myasthenia, and elevated levels of creatine kinase (CK) in asymptomatic patients. The potential pathogenic mechanism underlying the emergence of SIM includes cholesterol deficiency, decreased stability and permeability of the myocyte membrane, coenzyme Q10 deficiency leading to dysfunctional mitochondrial respiration and energy generation in myocytes, and decreased synthesis of isozymes resulting in enhanced risk of muscle toxicity [2, 3]. However, the occurrence of SIM varies among individuals depending on drug tolerance, underlying health conditions, and genetic factors. On average, SIM affects 1 in 1000 patients undergoing statin treatment. As a consequence, SIM is the major reason for non-adherence to and/or discontinuation of statin treatment, which results in adverse cardiovascular outcomes [4].
The genetic factors associated with SIM have been widely studied. In particular, single-nucleotide polymorphisms (SNPs) in some genes have been reported to affect SIM incidence. For instance, SNP-dependent dysfunction of solute carrier organic anion transporter family member 1B1 (SLCO1B1 or OATP1B1), a major transporter of statins involved in drug detoxification in the liver, is one of the factors influencing the specific efficacy and side effects of statins in different individuals. Additionally, SNPs in genes involved in drug metabolism, such as cytochrome P450 family genes (CYPs), COQ2, and ABCB1, have been reported to be associated with SIM [5]. However, these studies are limited and still inconclusive.
Our previous meta-analysis indicated that the SLCO1B1 T521C polymorphism is correlated with a markedly higher risk of SIM, especially upon treatment with simvastatin, rosuvastatin, and cerivastatin [6]. Moreover, the results of other meta-analyses were consistent with our findings [7]. However, another meta-analysis revealed that COQ2 rs4693075 is not correlated with SIM [8]. Similarly, another study reported that there was no significant correlation between the ABCB1 C3435T polymorphism and SIM, but that SIM risk was increased in patients using statins for longer than 5 months [9]. Most of these meta-analyses focused on one or two SNPs and used a random-effect or fixed-effect model according to the results of a homogeneity test. To overcome such limitations, in this study, we employed a mixed-effects model that could decompose the random error term into the corresponding level of the hierarchical structure. Furthermore, this model allowed to examine factors affecting the heterogeneity among the considered studies. Therefore, to comprehensively analyze current evidence of the correlation between genetic polymorphisms and the risk of developing SIM upon treatment with various statin types, we systematically screened the literature to include all reported genetic polymorphisms related to SIM and different types of statins.
Methods
Data source, search strategy, and study selection
This study was conducted according to the Meta-analysis of Observational Studies in Epidemiology (MOOSE) guidelines [10]. Two authors searched the literature through the PubMed, Embase, and Cochrane Library databases for studies published in English from inception to April 2019. The following terms were used in the search strategy: statin, statins, myalgia, myopathy, muscle injury, muscle pain myalgias, rhabdomyolysis, myotoxicity, polymorphism, SNP, genetic, mutation, variation, allelic, allele, and genotype. The details of the search strategy in PubMed are shown in Table S1. The reference lists of the retrieved studies and relevant reviews were also manually searched to obtain potentially new eligible studies.
Studies were included in the meta-analysis if they belonged to one of the following categories: (1) Case-control or cohort studies comparing patients developing SIM and patients exhibiting statin tolerance (no myopathy) after statin treatment; (2) studies assessing the correlation between genetic polymorphisms and risk of SIM; and (3) studies reporting the frequencies of specific alleles or the effect sizes of individual genotypes between SIM cases and controls. The exclusion criteria for the meta-analysis were set as follows: (1) Studies designed as case series; (2) studies not involving SIM; (3) studies using the healthy population as control group; (4) studies not involving SNPs; and (5) studies that did not report allelic frequencies or effect sizes. Additionally, reviews, case reports, and family genetic studies were excluded.
Data extraction and quality assessment
Two authors independently extracted the following data from the studies included in the meta-analysis: first author’s name, publication year, study location, study design, sample size and age, purpose of steroid treatment, types of statins employed, and genes of interest. The Newcastle-Ottawa Scale (NOS) was used to evaluate the quality of the included studies [11]. Through the NOS, it is possible to assign a rating to a study according to its scores in the following three categories: selection (four items, four stars), comparability (one item, two stars), and exposure (three items, three stars). The study quality was assessed by two authors, and any disagreement was resolved by another author after perusal of the original article.
Statistical analysis
Deviations of allele frequencies from Hardy-Weinberg equilibrium (HWE) were tested to assess the consistency of allele frequencies between subgroups of the included population [12]. Correlation analysis was performed using five genetic models: allelic (M vs W), dominant (MM + WM vs WW), recessive (MM vs WM + WW), heterozygous (WM vs WW), and homozygous (MM vs WW), where W represents the major (wild-type) allele and M represents the minor (mutant-type) allele [13]. The odds ratio (OR) and its 95% confidence interval (CI) were calculated to estimate pooled effect sizes, while heterogeneity across the included studies was assessed by I2 statistic. A random-effect model was applied to calculate the pooled effect size when I2 ≥ 50%, otherwise fixed-effect models were used. Subgroup analyses were performed with respect to the country-specific population if data were obtained from more than three studies. In addition, a meta-analysis using a mixed-effects model was conducted to assess the potential impacts of specific types of statins and SNPs on the risk of developing SIM. Publication biases for the investigated SNPs were assessed using two-tailed Egger’s and Begg’s tests. A p value of 0.05 was considered a threshold for statistical significance. The STATA software (version 10.0; Stata Corporation College Station, TX, USA) was employed for all statistical analyses in this study.
Results
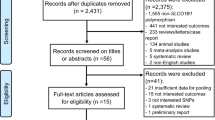
In total, 1457 studies were identified from the various databases. Among these, 1379 studies were excluded after screening of the title and abstract. The full text of the remaining 78 articles was then examined. During the full-text screening process, the following number of studies were excluded based on the following exclusion criteria: case-control studies not related to SIM (n = 22); studies lacking data on the number of SNP carriers or on effect size in each group (n = 7); studies that used the healthy population as control group (n = 6); reviews (n = 6); case reports (n = 2); conference articles (n = 2); and duplicated research (n = 1). Finally, 32 studies examining a total of 21,692 patients undergoing statin treatment were included in our analysis [14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45] (Table 1, Fig. 1).
The studies included in the meta-analysis were published between 2005 and 2018. Additionally, the test populations in these studies were from Europe and North America. All studies were designed as case-control studies, except for one retrospective study [38]. The average age of the patients was generally between 50 and 70 years. However, three studies did not specify the age of the patients [24,25,26]. The statins used in these studies were mainly simvastatin, rosuvastatin, pravastatin, atorvastatin, lovastatin, fluvastatin, pitavastatin, and cerivastatin. The NOS scores of the included studies were 7–9 points. Hence, the overall quality of the considered observational studies was ideal for our meta-analysis (Table 1).
In this study, we comprehensively analyzed the following SNPs: rs4149056, rs2306283, and rs4363657 in SLCO1B1; rs1045642 and rs2231142 in ABCB1; rs4693075 in COQ2; rs776746 in CYP3A5; and rs9806699, rs1719247, and rs1346268 in GATM. Each of these SNPs was examined in more than three studies included in the analysis. The effect of each SNP on SIM in each model is summarized in Table S2. For this analysis, we did not distinguish the effects of statins based on their type.
The analysis of heterozygous (OR: 1.51; 95% CI: 1.08–2.13; p = 0.017), homozygous (OR: 2.65; 95% CI: 1.43–4.92; p = 0.002), dominant (OR: 1.63; 95% CI: 1.16–2.29; p = 0.005), and recessive models (OR: 2.19; 95% CI: 1.33–3.61; p = 0.009) of SLCO1B1 rs4149056 showed that this SNP is associated with an increased risk of SIM. However, there was no significant correlation between this mutation and risk of SIM in the allelic model (OR: 1.34; 95% CI: 0.98–1.83; p = 0.069). On the contrary, the analysis of heterozygous (OR: 0.87; 95% CI: 0.76–1.00; p = 0.048) and dominant models (OR: 0.87; 95% CI: 0.76–0.99; p = 0.030) of SLCO1B1 rs4363657 revealed that the presence of the C allele decreases the risk of SIM. There were no other significant correlations between SNPs and the risk of SIM (Table 2). In addition, subgroup analysis of the UK and US populations revealed that heterogeneity was not reduced with respect to the general population. However, we observed a significant correlation between rs4149056 and the risk of SIM in the UK population, whereas no significant correlation was found in the US population. Subgroup analysis was not performed for the other SLCO1B1 SNPs because of the limited number of studies that reported these SNPs in each country (Table 2).
Due to the complexity of population characteristics in each included study, we analyzed the impact of different statin types and genetic polymorphisms on the risk of SIM using a mixed-effects model. In this analysis, we mainly included studies examining the effects of simvastatin, rosuvastatin, and atorvastatin. The other types of statins were not included as the respective studies did not separately report the results relative to those statins. The results of the analysis based on statin type are reported in Table 3. Within the simvastatin-treated population, the carriers of the mutation (TC/CC) responsible for the SLCO1B1 rs4149056 SNP exhibited a greater risk of SIM when compared to the wild-type population (OR: 3.10; 95% CI: 2.11–4.55; p < 0.001). Similar results were obtained when analyses were conducted separately for heterozygote (TC) carriers vs wild-type population (OR: 2.80; 95% CI: 1.81–4.31; p < 0.001) and homozygote (CC) carriers vs wild-type population (OR: 9.27; 95% CI: 4.04–21.22; p < 0.001). Interestingly, the rs4149056 SNP in heterozygote carriers within the rosuvastatin-treated population was associated with a reduced risk of SIM (OR: 0.82; 95% CI: 0.70–0.95; p = 0.012) (Table 3). However, this may be due to the greater heterogeneity and to the smaller number of studies dealing with these factors. In particular, this significant correlation could be biased towards the study conducted by Bai et al. [14], which included a large number of individuals carrying the rs4149056 SNP in the rosuvastatin-treated population. Additionally, GATM rs9806699 (mutant A allele) carriers within the rosuvastatin-treated population exhibited a lower risk of SIM when compared to the wild-type population (OR: 0.37; 95% CI: 0.17–0.78; p = 0.009). Similar results were obtained when the analyses were conducted separately for heterozygote carriers vs wild-type population (OR: 0.36; 95% CI: 0.17–0.76; p = 0.007) and homozygote carriers vs wild-type population (OR: 0.36; 95% CI: 0.18–0.72; p = 0.004) (Table 3).
Discussion
This study analyzed the correlation between genetic polymorphisms and risk of SIM within the statin-treated population using SNPs that had been reported in more than three studies. The analysis included 10 SNPs in five genes. Additionally, we performed a subgroup analysis in different populations and analyzed the impact of different statin types and genetic polymorphisms on the risk of SIM. The summary OR of the heterozygous, homozygous, dominant, and recessive models indicated a positive correlation between the nonsynonymous rs4149056 mutation in SLCO1B1 and SIM incidence. Conversely, the rs4363657 SNP, which exhibited nearly complete linkage disequilibrium with the rs4149056 SNP [39], was correlated with reduced SIM incidence in the heterozygous and dominant models. On the contrary, the rs1045642 SNP in ABCB1; the rs4693075 SNP in COQ2; the rs776746 SNP in CYP3A5; and the rs9806699, rs1719247, and rs1346268 SNPs in GATM were not correlated with the risk of SIM when the effects of all statins were analyzed together. However, when the analysis was stratified based on statin type, we observed that rs4149056 C carriers within the simvastatin-treated population presented an increased risk of SIM when compared to that within the wild-type population. Furthermore, GATM rs9806699 A carriers within the rosuvastatin-treated population exhibited a reduced risk of SIM. These findings could provide useful indications for the treatment of individuals carrying certain genetic polymorphisms with specific statins, in order to avoid excessive SIM risk.
The effect of the rs4149056 SNP in SLCO1B1 on the risk of SIM was consistent with previous meta-analyses [6, 7], although this was not confirmed by the allelic model. This could depend on the fact that, compared with the other models, our allelic model included three more studies from Saudi Arabia, the USA, and Italy [16, 33, 37]. However, these three studies did not report the frequencies of each genotype and hence were not considered in the other models. Moreover, subgroup analysis revealed no significant correlation between rs4149056 and SIM risk in the US population, which was included in our allelic model and in the study reported by Marciante et al. [33]. This study also included a large sample size (n = 917) in which the experimental group was treated with cerivastatin, whereas the control group was treated with lovastatin, simvastatin, atorvastatin, and pravastatin. Additionally, less than 1% of patients received cerivastatin. Therefore, the non-significant correlation that we observed may be due to the small number of studies included in the analysis and to the unbalanced experimental setup of the study conducted by Marciante et al. [33]. Moreover, the effect of the SLCO1B1 rs4149056 SNP on the risk of SIM varied according to the statin type. This phenomenon could be due to SNP-dependent altered transport activity of the organic anionic transporter SLCO1B1, possibly mediating the absorption of statins in hepatocytes [39, 46, 47].
Interestingly, the GATM rs9806699 A carriers within the rosuvastatin-treated population protected against the risk of SIM. This may be due to the involvement of the GATM gene in the energy metabolism of skeletal muscles [48]. Indeed, the A allele of GATM has been correlated with lower expression of GATM, which is responsible for creatine synthesis and thus provides a major energy source in skeletal muscles [24]. Therefore, the GATM A allele could induce attenuation of cellular metabolism and, consequently, diminish the energy-storing capacity of myocytes [24]. However, the cases in which GATM rs9806699 A carrier patients were treated with other types of statins were not addressed in this meta-analysis, since data were obtained from less than three studies.
In summary, our meta-analysis revealed that the 10 SNPs in five genes and nine statin types are correlated with the risk of SIM. However, subgroup analysis based on the country-specific population was conducted only for the rs4149056 SNP of SLCO1B1. On the contrary, stratified analyses based on the statin type were performed only for the rs4149056 and rs2306283 SNPs of SLCO1B1, the rs776746 SNP of CYP3A5, the rs3892097 SNP of CYP2D6, and the rs9806699 SNP of GATM, since a smaller number of studies investigated the remaining SNPs and those results needed further verification.
This meta-analysis is characterized by several strengths: (1) This meta-analysis provides comprehensive analysis of SNPs reported in more than three studies associated with the risk of SIM; (2) the results of a mixed-effects model were calculated to avoid random error; and (3) the analysis was based on a large sample size, and therefore, the results of this meta-analysis are more robust than those of each individual study. However, there are also several limitations in this meta-analysis. Indeed, this analysis was conducted at the study level, but not at the individual level, and did not include non-English literature, possibly resulting in data insufficiency. Furthermore, a mixed-effects model was used in this study, and hence, the effects of country location, patient’s clinical status, drug dose, and follow-up time on the outcome of statin treatment are still unclear. Moreover, since the analyses of this study were conducted on SNPs reported in more than three studies related to SIM, some key SNPs may have been overlooked if they had not been studied extensively. In addition, stratified analysis was conducted based on the country-specific population since most studies did not report the specific ethnic background of the patients. Finally, the results of stratified analyses were not conclusive because of the small number of included studies relative to numerous subgroups. Therefore, our study was mainly limited by the number of studies available at the time of analysis.
In conclusion, the rs4149056 SNP of the SLCO1B1 gene is correlated with an increased risk of SIM. On the contrary, the heterozygous and dominant models of SLCO1B1 rs4363657 showed that this SNP may protect against the risk of SIM. Additionally, the correlation of SLCO1B1 rs4149056 and GATM rs9806699 with the risk of SIM may depend on the use of simvastatin and rosuvastatin, respectively. A large-scale study should be conducted in the future to verify these findings and evaluate whether these correlations are influenced by the genetic or physiological characteristics of the patient.
Data Availability
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
References
Savarese G, Gotto AM, Jr., Paolillo S, D’Amore C, Losco T, Musella F, Scala O, Marciano C, Ruggiero D, Marsico F, De Luca G, Trimarco B, Perrone-Filardi P (2013) Benefits of statins in elderly subjects without established cardiovascular disease: a meta-analysis. Journal of the American College of Cardiology 62 (22):2090-2099. doi:https://doi.org/10.1016/j.jacc.2013.07.069
Vrablik M, Zlatohlavek L, Stulc T, Adamkova V, Prusikova M, Schwarzova L, Hubacek JA, Ceska R (2014) Statin-associated myopathy: from genetic predisposition to clinical management. Physiol Res 63(Suppl 3):S327–S334
Stalenhoef A (2015) Coenzyme Q10 and statin-related myopathy. Drug Ther Bull 53(5):54–56. https://doi.org/10.1136/dtb.2015.5.0325
Stroes ES, Thompson PD, Corsini A, Vladutiu GD, Raal FJ, Ray KK, Roden M, Stein E, Tokgozoglu L, Nordestgaard BG, Bruckert E, De Backer G, Krauss RM, Laufs U, Santos RD, Hegele RA, Hovingh GK, Leiter LA, Mach F, Marz W, Newman CB, Wiklund O, Jacobson TA, Catapano AL, Chapman MJ, Ginsberg HN, European Atherosclerosis Society Consensus P (2015) Statin-associated muscle symptoms: impact on statin therapy-European Atherosclerosis Society Consensus Panel Statement on Assessment, Aetiology and Management. European heart journal 36 (17):1012-1022. doi:https://doi.org/10.1093/eurheartj/ehv043
Needham M, Mastaglia FL (2014) Statin myotoxicity: a review of genetic susceptibility factors. Neuromuscul Disord 24(1):4–15. https://doi.org/10.1016/j.nmd.2013.09.011
Xiang Q, Chen SQ, Ma LY, Hu K, Zhang Z, Mu GY, Xie QF, Zhang XD, Cui YM (2018) Association between SLCO1B1 T521C polymorphism and risk of statin-induced myopathy: a meta-analysis. Pharmacogenomics J 18(6):721–729. https://doi.org/10.1038/s41397-018-0054-0
Hou Q, Li S, Li L, Li Y, Sun X, Tian H (2015) Association between SLCO1B1 gene T521C polymorphism and statin-related myopathy risk: a meta-analysis of case-control studies. Medicine 94(37):e1268. https://doi.org/10.1097/MD.0000000000001268
Canestaro WJ, Austin MA, Thummel KE (2014) Genetic factors affecting statin concentrations and subsequent myopathy: a HuGENet systematic review. Genet Med 16(11):810–819. https://doi.org/10.1038/gim.2014.41
Su J, Xu H, Yang J, Yu Q, Yang S, Zhang J, Yao Q, Zhu Y, Luo Y, Ji L, Zheng Y, Yu J (2015) ABCB1 C3435T polymorphism and the lipid-lowering response in hypercholesterolemic patients on statins: a meta-analysis. Lipids Health Dis 14:122. https://doi.org/10.1186/s12944-015-0114-2
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. Jama 283(15):2008–2012. https://doi.org/10.1001/jama.283.15.2008
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605. https://doi.org/10.1007/s10654-010-9491-z
Chen J, Chatterjee N (2007) Exploiting Hardy-Weinberg equilibrium for efficient screening of single SNP associations from case-control studies. Hum Hered 63(3-4):196–204. https://doi.org/10.1159/000099996
Areeshi MY, Mandal RK, Panda AK, Bisht SC, Haque S (2013) CD14 -159 C>T gene polymorphism with increased risk of tuberculosis: evidence from a meta-analysis. PloS one 8(5):e64747. https://doi.org/10.1371/journal.pone.0064747
Bai X, Zhang B, Wang P, Wang GL, Li JL, Wen DS, Long XZ, Sun HS, Liu YB, Huang M, Zhong SL (2019) Effects of SLCO1B1 and GATM gene variants on rosuvastatin-induced myopathy are unrelated to high plasma exposure of rosuvastatin and its metabolites. Acta Pharmacol Sin 40(4):492–499. https://doi.org/10.1038/s41401-018-0013-y
Bakar NS, Neely D, Avery P, Brown C, Daly AK, Kamali F (2018) Genetic and clinical factors are associated with statin-related myotoxicity of moderate severity: a case-control study. Clinical pharmacology and therapeutics 104(1):178–187. https://doi.org/10.1002/cpt.887
Alghalyini B, El Shamieh S, Salami A, Visvikis Siest S, Fakhoury HM, Fakhoury R (2018) Effect of SLCO1B1 gene polymorphisms and vitamin D on statin-induced myopathy. Drug Metab Pers Ther 33(1):41–47. https://doi.org/10.1515/dmpt-2017-0030
KS M, Maroteau C, Veluchamy A, Tornio A, Tavendale R, Carr F, Abelega NU, Carr D, Bloch K, Hallberg P, Yue QY, Pearson ER, Colhoun HM, Morris AD, Dow E, George J, Pirmohamed M, Ridker PM, ASF D, Alfirevic A, Wadelius M, Maitland-van der Zee AH, Chasman DI, CNA P, Consortium P-A (2017) A common missense variant of LILRB5 is associated with statin intolerance and myalgia. European heart journal 38(48):3569–3575. https://doi.org/10.1093/eurheartj/ehx467
Liu JE, Liu XY, Chen S, Zhang Y, Cai LY, Yang M, Lai WH, Ren B, Zhong SL (2017) SLCO1B1 521T > C polymorphism associated with rosuvastatin-induced myotoxicity in Chinese coronary artery disease patients: a nested case-control study. Eur J Clin Pharmacol 73(11):1409–1416. https://doi.org/10.1007/s00228-017-2318-z
Hubacek JA, Adamkova V, Zlatohlavek L, Steiner-Mrazova L, Vrablik M (2017) COQ2 polymorphisms are not associated with increased risk of statin-induced myalgia/myopathy in the Czech population. Drug Metab Pers Ther 32(4):177–182. https://doi.org/10.1515/dmpt-2017-0027
Ovesjo ML, Skilving I, Bergman P, Rane A, Ekstrom L, Bjorkhem-Bergman L (2016) Low vitamin D levels and genetic polymorphism in the vitamin D receptor are associated with increased risk of statin-induced myopathy. Basic Clin Pharmacol Toxicol 118(3):214–218. https://doi.org/10.1111/bcpt.12482
Khine H, Yuet WC, Adams-Huet B, Ahmad Z (2016) Statin-associated muscle symptoms and SLCO1B1 rs4149056 genotype in patients with familial hypercholesterolemia. Am Heart J 179:1–9. https://doi.org/10.1016/j.ahj.2016.05.015
Luzum JA, Kitzmiller JP, Isackson PJ, Ma C, Medina MW, Dauki AM, Mikulik EB, Ochs-Balcom HM, Vladutiu GD (2015) GATM polymorphism associated with the risk for statin-induced myopathy does not replicate in case-control analysis of 715 dyslipidemic individuals. Cell Metab 21(4):622–627. https://doi.org/10.1016/j.cmet.2015.03.003
Hubacek JA, Dlouha D, Adamkova V, Zlatohlavek L, Viklicky O, Hruba P, Ceska R, Vrablik M (2015) SLCO1B1 polymorphism is not associated with risk of statin-induced myalgia/myopathy in a Czech population. Med Sci Monit 21:1454–1459. https://doi.org/10.12659/MSM.893007
Mangravite LM, Engelhardt BE, Medina MW, Smith JD, Brown CD, Chasman DI, Mecham BH, Howie B, Shim H, Naidoo D, Feng Q, Rieder MJ, Chen YD, Rotter JI, Ridker PM, Hopewell JC, Parish S, Armitage J, Collins R, Wilke RA, Nickerson DA, Stephens M, Krauss RM (2013) A statin-dependent QTL for GATM expression is associated with statin-induced myopathy. Nature 502(7471):377–380. https://doi.org/10.1038/nature12508
Carr DF, Alfirevic A, Johnson R, Chinoy H, van Staa T, Pirmohamed M (2014) GATM gene variants and statin myopathy risk. Nature 513(7518):E1. https://doi.org/10.1038/nature13628
Floyd JS, Bis JC, Brody JA, Heckbert SR, Rice K, Psaty BM (2014) GATM locus does not replicate in rhabdomyolysis study. Nature 513(7518):E1–E3. https://doi.org/10.1038/nature13629
Ferrari M, Guasti L, Maresca A, Mirabile M, Contini S, Grandi AM, Marino F, Cosentino M (2014) Association between statin-induced creatine kinase elevation and genetic polymorphisms in SLCO1B1, ABCB1 and ABCG2. Eur J Clin Pharmacol 70(5):539–547. https://doi.org/10.1007/s00228-014-1661-6
Danik JS, Chasman DI, MacFadyen JG, Nyberg F, Barratt BJ, Ridker PM (2013) Lack of association between SLCO1B1 polymorphisms and clinical myalgia following rosuvastatin therapy. Am Heart J 165(6):1008–1014. https://doi.org/10.1016/j.ahj.2013.01.025
Carr DF, O’Meara H, Jorgensen AL, Campbell J, Hobbs M, McCann G, van Staa T, Pirmohamed M (2013) SLCO1B1 genetic variant associated with statin-induced myopathy: a proof-of-concept study using the clinical practice research datalink. Clinical pharmacology and therapeutics 94(6):695–701. https://doi.org/10.1038/clpt.2013.161
Santos PC, Gagliardi AC, Miname MH, Chacra AP, Santos RD, Krieger JE, Pereira AC (2012) SLCO1B1 haplotypes are not associated with atorvastatin-induced myalgia in Brazilian patients with familial hypercholesterolemia. Eur J Clin Pharmacol 68(3):273–279. https://doi.org/10.1007/s00228-011-1125-1
Brunham LR, Lansberg PJ, Zhang L, Miao F, Carter C, Hovingh GK, Visscher H, Jukema JW, Stalenhoef AF, Ross CJ, Carleton BC, Kastelein JJ, Hayden MR (2012) Differential effect of the rs4149056 variant in SLCO1B1 on myopathy associated with simvastatin and atorvastatin. Pharmacogenomics J 12(3):233–237. https://doi.org/10.1038/tpj.2010.92
Vladutiu GD, Isackson PJ, Kaufman K, Harley JB, Cobb B, Christopher-Stine L, Wortmann RL (2011) Genetic risk for malignant hyperthermia in non-anesthesia-induced myopathies. Mol Genet Metab 104(1-2):167–173. https://doi.org/10.1016/j.ymgme.2011.07.001
Marciante KD, Durda JP, Heckbert SR, Lumley T, Rice K, McKnight B, Totah RA, Tamraz B, Kroetz DL, Fukushima H, Kaspera R, Bis JC, Glazer NL, Li G, Austin TR, Taylor KD, Rotter JI, Jaquish CE, Kwok PY, Tracy RP, Psaty BM (2011) Cerivastatin, genetic variants, and the risk of rhabdomyolysis. Pharmacogenet Genomics 21(5):280–288. https://doi.org/10.1097/FPC.0b013e328343dd7d
Isackson PJ, Ochs-Balcom HM, Ma C, Harley JB, Peltier W, Tarnopolsky M, Sripathi N, Wortmann RL, Simmons Z, Wilson JD, Smith SA, Barboi A, Fine E, Baer A, Baker S, Kaufman K, Cobb B, Kilpatrick JR, Vladutiu GD (2011) Association of common variants in the human eyes shut ortholog (EYS) with statin-induced myopathy: evidence for additional functions of EYS. Muscle & nerve 44(4):531–538. https://doi.org/10.1002/mus.22115
Hoenig MR, Walker PJ, Gurnsey C, Beadle K, Johnson L (2011) The C3435T polymorphism in ABCB1 influences atorvastatin efficacy and muscle symptoms in a high-risk vascular cohort. J Clin Lipidol 5(2):91–96. https://doi.org/10.1016/j.jacl.2011.01.001
Donnelly LA, Doney AS, Tavendale R, Lang CC, Pearson ER, Colhoun HM, McCarthy MI, Hattersley AT, Morris AD, Palmer CN (2011) Common nonsynonymous substitutions in SLCO1B1 predispose to statin intolerance in routinely treated individuals with type 2 diabetes: a go-DARTS study. Clinical pharmacology and therapeutics 89(2):210–216. https://doi.org/10.1038/clpt.2010.255
Puccetti L, Ciani F, Auteri A (2010) Genetic involvement in statins induced myopathy. Preliminary data from an observational case-control study. Atherosclerosis 211(1):28–29. https://doi.org/10.1016/j.atherosclerosis.2010.02.026
Linde R, Peng L, Desai M, Feldman D (2010) The role of vitamin D and SLCO1B1*5 gene polymorphism in statin-associated myalgias. Dermatoendocrinol 2(2):77–84. https://doi.org/10.4161/derm.2.2.13509
Search Collaborative Group, Link E, Parish S, Armitage J, Bowman L, Heath S, Matsuda F, Gut I, Lathrop M, Collins R (2008) SLCO1B1 variants and statin-induced myopathy--a genomewide study. The New England journal of medicine 359(8):789–799. https://doi.org/10.1056/NEJMoa0801936
Zuccaro P, Mombelli G, Calabresi L, Baldassarre D, Palmi I, Sirtori CR (2007) Tolerability of statins is not linked to CYP450 polymorphisms, but reduced CYP2D6 metabolism improves cholesteraemic response to simvastatin and fluvastatin. Pharmacol Res 55(4):310–317. https://doi.org/10.1016/j.phrs.2006.12.009
Oh J, Ban MR, Miskie BA, Pollex RL, Hegele RA (2007) Genetic determinants of statin intolerance. Lipids Health Dis 6:7. https://doi.org/10.1186/1476-511X-6-7
Frudakis TN, Thomas MJ, Ginjupalli SN, Handelin B, Gabriel R, Gomez HJ (2007) CYP2D6*4 polymorphism is associated with statin-induced muscle effects. Pharmacogenet Genomics 17(9):695–707. https://doi.org/10.1097/FPC.0b013e328012d0a9
Fisher NM, Meksawan K, Limprasertkul A, Isackson PJ, Pendergast DR, Vladutiu GD (2007) Statin therapy depresses total body fat oxidation in the absence of genetic limitations to fat oxidation. J Inherit Metab Dis 30(3):388–399. https://doi.org/10.1007/s10545-007-0449-6
Wilke RA, Moore JH, Burmester JK (2005) Relative impact of CYP3A genotype and concomitant medication on the severity of atorvastatin-induced muscle damage. Pharmacogenet Genomics 15(6):415–421
Fiegenbaum M, da Silveira FR, Van der Sand CR, Van der Sand LC, Ferreira ME, Pires RC, Hutz MH (2005) The role of common variants of ABCB1, CYP3A4, and CYP3A5 genes in lipid-lowering efficacy and safety of simvastatin treatment. Clinical Pharmacology and Therapeutics 78(5):551–558. https://doi.org/10.1016/j.clpt.2005.08.003
Smith NF, Figg WD, Sparreboom A (2005) Role of the liver-specific transporters OATP1B1 and OATP1B3 in governing drug elimination. Expert Opin Drug Metab Toxicol 1(3):429–445. https://doi.org/10.1517/17425255.1.3.429
Nishizato Y, Ieiri I, Suzuki H, Kimura M, Kawabata K, Hirota T, Takane H, Irie S, Kusuhara H, Urasaki Y, Urae A, Higuchi S, Otsubo K, Sugiyama Y (2003) Polymorphisms of OATP-C (SLC21A6) and OAT3 (SLC22A8) genes: consequences for pravastatin pharmacokinetics. Clinical pharmacology and therapeutics 73(6):554–565. https://doi.org/10.1016/s0009-9236(03)00060-2
Norata GD, Tibolla G, Catapano AL (2014) Statins and skeletal muscles toxicity: from clinical trials to everyday practice. Pharmacol Res 88:107–113. https://doi.org/10.1016/j.phrs.2014.04.012
Funding
This study was supported by grants from the National Key R&D Program of China (No. 2016YFC0904900), the National Natural Science Foundation (No. 81872940 and No. 81973395) of China, the Natural Science Foundation of Beijing Municipality (No. 7171012), and the National Science and Technology Major Projects for “Major New Drugs Innovation and Development” of China (No. 2017ZX09304028 and No. 2017ZX09101001).
Author information
Authors and Affiliations
Contributions
QX and XDZ wrote the manuscript; QX and YMC designed the research; QFX, KH, ZZ, LM, and JJ performed the research; GYM, ZW, and ZYL analyzed the data; ZYL and XDZ contributed new reagents/analytical tools.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethics approval
Not applicable
Consent to participate
Not applicable
Consent for publication
Not applicable
Code availability
Not applicable
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Xiang, Q., Zhang, XD., Mu, GY. et al. Correlation between single-nucleotide polymorphisms and statin-induced myopathy: a mixed-effects model meta-analysis. Eur J Clin Pharmacol 77, 569–581 (2021). https://doi.org/10.1007/s00228-020-03029-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-020-03029-1