Abstract
Purpose
The aim of this study was to describe persistence with vitamin K antagonist (VKA) treatment in German atrial fibrillation (AF) patients and to identify factors which may be associated with early discontinuation of VKA therapy.
Methods
We did a retrospective cohort study based on an anonymized German claims dataset with VKA treatment-naïve AF patients, who received at least one VKA prescription. VKA therapy discontinuation was defined as a gap >180 days.
Results
We identified 38,076 VKA patients who started a VKA therapy (mean age 76.13 years; 56.08% female; mean CHA2DS2-VASc-Score 4.49; mean Charlson Comorbidity Index (CCI) 3.91). After four quarters since start of VKA treatment, 14,889 (39.10%) of observed patients had discontinued their VKA treatment (after eight quarters: 54.61%). Mean time until treatment discontinuation was 390.55 days. Risk of VKA discontinuation increased with the diagnosis of dementia within the first two quarters of VKA treatment [HR 1.35 (95% CI 1.29–1.40)], diagnosed alcohol or drug abuse in the baseline period [HR 1.25; 95% CI 1.18–1.33)], female gender [HR 1.08; 95% CI 1.05–1.10)], higher age (HR 1.03; 95% CI 1.03–1.03), higher CCI (HR 1.05; 95% CI 1.04–1.05), any prescription of NSAID (HR 1.07; 95% CI 1.04–1.10), and number of surgeries in the first two quarters of VKA treatment (HR 1.05; 95% CI 1.04–1.05). At least one yearly visit to a cardiologist since start of VKA treatment decreased the risk of non-persistence [HR 0.90; 95% CI 0.88–0.93] and a cancer diagnosis in the baseline period (HR 0.92; 95% CI 0.89–0.96).
Conclusion
Non-persistence related to VKA therapy is common in AF patients. Older more comorbid female patients as well as patients who face surgeries and who do not visit a cardiologist regularly face a higher therapy discontinuation risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Atrial fibrillation (AF) is the most common significant cardiac rhythm disorder [1]. It is associated with substantial lethality from stroke and thromboembolism [1,2,3,4]. Oral anticoagulation (OAC) with either vitamin K antagonists (VKAs) or non-VKA oral anticoagulants (NOACs) is recommended by guidelines for patients with a moderate to high risk of stroke [5,6,7,8].
Despite the established benefits of using OAC in AF patients, OAC medication remains under-used [9,10,11,12]. A systematic review found that almost 90% of included studies showed an OAC under-use, i.e., less than 70% of the patients that were eligible for OAC treatment received OAC [9]. Two recent German claim-based data analyses concluded that, based on AF patients clearly indicated for OAC use both in terms of existing stroke risk and non-existence of factors disfavoring OAC use, about 40% of the observed patients did not receive an OAC [13, 14]. OAC under-use was associated with an increased stroke risk in these studies [10, 13, 14].
A substantial part of OAC under-use in real-world treatment practice remains unexplained [14]. Specifically, it is unknown which percentage of OAC non-use AF patients are OAC therapy-naive patients and which percentage started an OAC therapy earlier, but discontinued it for whatever reason. This information may have far-reaching consequences. An OAC treatment-naive patient generally eligible for OAC could receive any available OAC agent, whereas patients having discontinued a treatment with one of the agent classes (i.e., VKAs or NOACs) may only receive other agent classes.
Available data on persistence with OAC therapy, specifically VKA therapy, which are mainly based on US claims data analyses, reported warfarin discontinuation rates of 30–40% after 12 months and as high as >50% after 24 months in newly treated AF patients [12, 15,16,17]. Recent bleeding seemed to be a predictor for discontinuation of warfarin therapy [16]. Data for Europe are much less conclusive. A Danish analysis reported a VKA discontinuation rate of >30% after 500 days [18] with higher discontinuation rates among patients with Eastern/African origin. A UK analysis determined a 1-year persistence of 70% for warfarin and 50% for aspirin with a trend of increasing persistence with warfarin with age and with CHADS2-Score [19], whereas recently published European registry data showed a high VKA continuation rate of 84% after 12 months [20]. Finally, it is unknown whether a high percentage of European AF patients discontinue their VKA therapy early.
Consequently, based on an analysis of a large longitudinal claim-based dataset delivered by a German health insurance fund, the aim of this study was to describe persistence with VKA treatment in German AF patients and to identify patient- and treatment-related factors which may be associated with early discontinuation of VKA therapy.
Methods
Sample
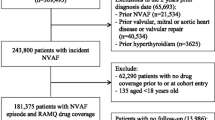
We did a retrospective analysis of an anonymized claims dataset which was provided by a German statutory health insurance fund (AOK PLUS) currently insuring three million people or more than 4% of the insured population by statute in Germany. It covered the years 2010 to first half of 2014. The database included information on patients’ demographics, outpatient treatment (diagnosis codes and visits to GP’s/specialists), inpatient treatment (dates, main diagnoses, procedures, length of stay), and claims filled for prescription medications.
Study population
A patient was included in our analysis if at least two outpatient or one inpatient diagnosis of AF were recorded in the inclusion period between July 2010 and December 2011 (ICD10-Code I48.1). For all patients, the minimum follow-up period was defined to be 2.5 years (until 30/06/2014), only in case of death this period was shorter. Patients aged 18 years or older and continuously insured between January 2010 and June 2014 were included; death during that period did not lead to exclusion of a patient.
We identified all AF patients who started their VKA treatment by filling a VKA prescription in the same quarter of the first observed AF diagnosis or, alternatively, at least in one of the three subsequent quarters. Incident VKA use was defined as at least one filled VKA prescription (Anatomical Therapeutic Chemical Classification (ATC)-code B01AA) without any VKA prescriptions in the previous two quarters (“newly treated” patients: NT patients). In a sensitivity analysis, we defined a period of four quarters without any previous VKA prescription to be an incident VKA prescription (“NT patients (2)”). Date of the first observed VKA prescription was defined as the index date, the two quarters before the index date were defined as baseline period.
Analysis of VKA therapy discontinuation
We investigated VKA treatment persistence in AF patients who started treatment between July 2010 and December 2011. The daily prescribed dosage of a VKA therapy is not available in German claims data. In accordance with previous analyses [13, 14], we assumed that the defined daily dosage (DDD) as defined by the WHO [21] is a proxy for the prescribed daily dosage. VKA treatment was considered as discontinued when an AF patient did not refill a VKA prescription within 180 days from the end of the last expected drug coverage date of the last observed prescription. This 180 days’ gap is a very conservative approach. It was used in previous analyses and reflects the wide variance in dosage and the possibility that VKA may be used at low dosages [22, 23].
In a sensitivity analysis, the 180 days’ gap, which was always measured from the end of the last expected drug coverage, was changed to (1) 90 days, (2) a gap that was at least equal in size of the drug coverage days provided by the last prescription, and (3) a gap that was at least equal twice in size of the drug coverage days provided by the last prescription. Patients who discontinued their VKA treatment because of death were not considered as non-persistent.
The cumulative probability of VKA discontinuation over time was plotted using the Kaplan-Meier (KM) method; death of patients led to censoring of patients. Different KM probability curves were plotted for male/female patients and patients with a high/low CHA2DS2-VASc-Score. This score always referred to inpatient/outpatient diagnoses observed in the preceding two quarters before the index date (baseline period). KM curves were compared to each other using log-rank tests.
Finally, for all newly treated non-persistent VKA patients with a minimum follow-up of 1 year after VKA discontinuation date, we assessed further anticoagulation treatment until the end of the observational period.
Assessment of factors associated with VKA discontinuation
A multivariate Cox proportional hazard model was used to determine factors associated with VKA discontinuation; results were presented as hazard ratios (HRs). As independent predictors, we included the following: age, gender, the CHA2DS2-VASc-Score, the Charlson Comorbidity Index (CCI) [24], the number of prescribed medications (excluding any antithrombotic agents) during VKA treatment, any prescription of NSAIDs during VKA treatment, existence of intracranial and/or gastrointestinal bleedings, dementia, risk of falling, any documented cancer disease, alcohol/drug abuse, observed inpatient surgeries during VKA treatment, and visits to cardiologists during VKA treatment (Supplemental Table A).
We used a backward stepwise elimination to determine the most significant factors associated with VKA discontinuation probabilities. Regression terms at a significance level of p > 0.10 were successively eliminated. The model was adjusted for age, gender, and adjusted CHA2DS2-Vasc-Score (Supplemental Table A). A significance level of 0.05 was chosen for analysis.
Results
Sample characteristics
We identified 61,646 AF patients that were treated with VKAs, 38,076 (61.77%) of these patients did not receive any VKA prescription in the previous 2 quarters (NT patients) (Table 1). Mean age in the NT sample was 76.13 years and 56.08% (21,354) of the patients were female. Based on the two quarters before VKA treatment initiation (baseline period), the mean CHA2DS2-VASc-Score in this sample was 4.49 and the mean CCI was 3.91. The death rate during the observational period was 61.27 deaths per 1000 patient years (Table 1).
In the sensitivity analysis, we identified 14,168 patients (22.98%) as NT patients (2) with a duration of the pre-index period without any VKA prescriptions of 4 quarters instead of 2 quarters. The patient characteristics were similar to the standard definition of “NT patients”. The gender distribution, number of different drugs, number of surgeries, CHA2DS2-VASc-Score, and CCI were nearly identical. Patients in the “NT (2)”-sample were on average a half year younger than in the “NT”-sample (75.48 vs. 76.13 years), whereas the death rate was slightly higher (63.72 vs. 61.20 cases per 1000 patient years) (Table 1).
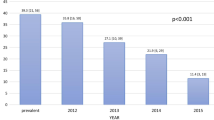
Persistence with VKA treatment
After 4 quarters since start of VKA treatment, 14,889 (39.10%) of all NT patients had discontinued their VKA treatment (base-case; minimum gap of 180 days) (Table 2). Non-persistent patients were significantly older (77.71 vs. 75.12 years, p < 0.001) and more female (59.33 vs. 54.00%) compared to the persistent patients. Furthermore, they faced a higher stroke risk indicated by the CHA2DS2-VASc-Score (2.46 vs. 2.34, p < 0.001; score excludes age and gender) and had a higher comorbidity burden as measured by the CCI (4.19 vs. 3.73, p < 0.001). Additionally, the death rate of non-persistent patients was considerably higher than in the patient group still persistent with VKA therapy after four quarters (86.74 vs. 46.20 patients per 1000 patient years, p < 0.001) (Table 2).
The sensitivity analysis based on the NT patients (2) sample showed similar results: 42.17% of the patients had discontinued their VKA treatment within the first four quarters. Just as in the base NT-definition, the non-persistent patients were older, more female, and had more comorbidities. The death rate of non-persistent patients was more than twice as high as in the patient group still persistent with VKA therapy after four quarters (95.22 vs. 42.15 patients per 1000 patient years, p < 0.001) (Table 2).
After eight quarters, 54.61% of all NT patients had discontinued their VKA treatment. This percentage rose to 66.37% in the entire follow-up period. Mean time until treatment discontinuation was 390.55 days (SD 315.57; Table 3).
In a sensitivity analysis using a minimum treatment gap of either 90 days (scenario 2), the length of the DDD of the last prescription (scenario 3), and twice the length of the DDD of the last prescription (scenario 4), percentages of NT patients who discontinued their VKA therapy after 4/8 quarters were 68.09%/82.14% (scenario 2), 64.36%/79.12% (scenario 3), and 35.15%/50.65% (scenario 4). Mean time until treatment discontinuation was 284.93 days (scenario 2; SD 275.17), 297.65 days (scenario 3; SD 280.77), and 399.07 days (scenario 4; SD 316.15) (Table 3).
Figure 1 presents the KM curves of cumulative VKA treatment continuation probabilities in different settings. The KM analysis showed a difference in VKA treatment persistence between males and females (diagram 1; higher treatment continuation rates for males, log-rank test result, p < 0.001) as well as between patients with a low (0 or 1) or high (2 or more) CHA2DS2-VASc-Score (score excluded age and gender as factors; diagram 2; log-rank test result, p < 0.001).
KM curves for percentage of persistent VKA patients during the whole observational follow-up period. The figure shows KM curves regarding the percentage of AF VKA-treatment-naive patients persistent with their VKA therapy (main scenario 1 with treatment gap >180 days as definition of non-persistence) for a sample of 38,076 patients, for different patient groups as defined by CHA2DS2-VASc-Score (0–1; 2+) and gender (male/female). Bottom-left graph shows the result of sensitivity analyses with different gap definitions (180 days (main scenario), 90 days’ gap, length of DDD gap and twice the length of DDD gap). Bottom-right graph shows the results with the alternative definition of “newly treated” patients and the different gap definitions (90 days’ gap, 180 days’ gap, length of DDD gap and twice the length of DDD gap)
From all newly treated patients (NT sample) who discontinued therapy, 12,643 could be observed for at least 1 year after date of start of VKA discontinuation. Within the first follow-up year, 6449 patients (51.01%) started a VKA therapy again, and 959 patients (7.59%) started a NOAC therapy (Dabigatran, Rivaroxaban, or Apixaban). Mean duration from VKA-discontinuation until restart was 273.25 days (SD 145.00), while mean time until start of NOAC therapy was 499.17 days (SD 336.83) (Table 4).
Factors associated with VKA treatment discontinuation
Table 5 describes results of the multivariable Cox regression analysis with regard to factors that may be associated with early VKA therapy discontinuation for all four observed scenarios. The following factors were excluded because they were not found to be statistically significant: alcohol/drug abuse two quarters after index date, risk of falling two quarters before and/or after index date, and a cancer diagnosis two quarters after index date.
The risk of VKA discontinuation increased with the diagnosis of dementia within the first two quarters of VKA treatment [scenario 1 HR 1.35 (95% CI 1.29–1.40), p < 0.001], with diagnosed alcohol or drug abuse in the baseline period [scenario 1 HR 1.25 (95% CI 1.18–1.33), p < 0.001], female gender [scenario 1 HR 1.08 (95% CI 1.05–1.10), p < 0.001], higher age (HR 1.03; 95% CI 1.03–1.03), higher CCI (HR 1.05; 95% CI 1.04–1.05), any prescription of NSAID (HR 1.07; 95% CI 1.04–1.10), and number of surgeries in the first two quarters of VKA treatment (HR 1.05; 95% CI 1.04–1.05).
At least one yearly visit to a cardiologist since start of VKA treatment decreased the risk of non-persistence [scenario 1 HR 0.90 (95% CI 0.88–0.93), p < 0.001] as well as a cancer diagnosis in the baseline period (HR 0.92; 95% CI 0.89–0.96).
The Cox-regression analyses using different treatment gap definitions (scenarios 2–4) showed similar results. In contrast to scenario 1, a higher CHA2DS2-VASc-Score (HR 0.97 in scenario 2 and 3 [95% CI 0.96–0.98]) as well as number of different prescribed agents (HR 0.98 in scenario 2 [95% CI 0.98–0.99] and HR 0.99 in scenario 3 [95% CI: 0.98–0.99]) gained significance as factors decreasing the risk of VKA therapy discontinuation (Table 5).
Discussion
Both medication adherence and persistence are known to have a high impact on real-life therapy effectiveness [12, 25, 26]. Obviously, an OAC treatment that is discontinued for whatever reason no longer protects an AF patient from the increased stroke risk that is associated with his disease. Consequently, known treatment guidelines recommend lifelong OAC in most AF patients. Any deviation from that recommendation, such as an early discontinuation of VKA therapy, puts patients at unnecessarily higher risks of a thromboembolic event. Therefore, the main aim of this study was to assess the degree of “early” non-persistence (after four and eight quarters) of VKA therapy in AF patients.
We identified a VKA discontinuation rate of 39.10/54.61% 4/8 quarters after VKA therapy start, based on a gap of at least 180 days as treatment gap definition. In our sensitivity analyses, these results were mainly confirmed. Overall, our findings are in line with some previous US and European studies [12, 17, 27, 28]. However, methodological differences between these studies (gap definition, definition of daily prescribed dosage, patient inclusion criteria, etc.) make it difficult to compare our non-persistence rates with those reported in previous publications. In line with this, reported non-persistence rates in previous studies range from 16 to 74.5% [22, 29].
On the other hand, we cannot confirm recent data from a European registry which showed a high VKA continuation rate of 84% after four quarters [20]. This number is only comparable to our percentage of patients who either continued their VKA therapy or re-started it after a treatment gap of at least 180 days. About half of the patients affected by non-persistence do not stop their treatment altogether, but re-start it after a mean of 273 days. However, such a VKA re-start is nevertheless associated with a substantial gap in drug supply. We therefore conclude that such a treatment should not be characterized as continued treatment.
We observed a substantially higher death rate in our non-persistent patient sample. However, whether non-persistence to VKA treatment caused a higher death rate or, conversely, a significant worsening of the health situation of the patients led to discontinuation of VKA treatment is not known.
We identified some factors being associated with a higher therapy discontinuation risk (age, gender, alcohol/drug abuse, diagnosis of dementia, NSAID prescriptions, surgeries), whereas regular cardiologist visits or a previous cancer diagnosis reduced the therapy discontinuation risk. Some of these factors were also be found to be associated with VKA therapy discontinuation in earlier publications [19, 22, 29, 30]. Interestingly and well in line with our data, frequent cardiologist visits have also been shown to be associated with a lower OAC under-use probability [13]. We identified surgeries as a factor increasing the VKA discontinuation risk. A surgery is a clinically appropriate reason to interrupt VKA treatment for a limited period; typically, these days are bridged by a low-molecular weight heparin. After the surgery, therapy should be continued [31, 32]. Our results indicate that this does not always work in real-life care of patients.
The most common presumed reason to discontinue VKA treatment is a previous bleeding event [23, 33]. In our observed patient sample, 8.44% of patients experienced a bleeding event two quarters before the start of VKA treatment, whereas 8.25% experienced such an event within the first two quarters after therapy start. In our study, previous bleedings reduced the risk of VKA therapy discontinuation potentially indicating a tighter INR (international normalized ratio) control in these patients. On the other hand, a bleeding event after index date which was most probably caused by the current VKA treatment increased the discontinuation probability. Especially less severe bleeding events are typically dealt with at outpatient GP practices; here, a discontinuation of treatment might be the more often chosen option because GP may be afraid of future bleedings [34, 35].
Without having data that could confirm this hypothesis, we presume that properties of VKA agents also play a role in the substantial percentage of AF patients discontinuing this treatment. VKAs do have well-known weaknesses, including necessary dosing adjustments in conjunction with regular INR value monitoring, drug/food interactions, and the need of periprocedural interruption (bridging), which may be associated with a substantial burden to patients [14]. Furthermore, it is known that AF patients prefer treatments that are easy to administer so that a VKA therapy is less preferred and, consequently, discontinued [36, 37]. Nevertheless, it remains for future research to compare the persistence of a VKA treatment with that of a more preferred NOAC treatment, persistence may even differ between different NOAC agents.
Overall, our data show an urgent need for improvement of the real-world treatment of AF patients. An OAC treatment in AF patients is supposed to be implemented as lifelong treatment. Our data show that, within 1 year, already 40% of the patients experienced a treatment gap of at least 180 days. Even if about 50% of these patients restart their VKA treatment after the break again and another 8% switch to a therapy with NOACs, this result is far from being optimal.
Limitations
We acknowledge some limitations of the study. First, due to limited data availability, we could not analyze all factors potentially explaining discontinuation of VKA therapy. Mainly, not only factors, describing knowledge/beliefs of physicians/patients, but also potential difficulties with INR management and previous negative experiences with VKA which were not documented in our claims database were not included.
Second, as is usual with claim-based data studies, its weakness lies in the fact that these data were primarily collected for financial claims and not gathered specifically for research purposes. Limitations are present in both the levels of detail and precision. Several data on potentially contributing or confounding risk factors regarding VKA use, e.g., INR values, were not available. Nevertheless, and despite these weaknesses, existing investigations show that claim-based datasets can be used as valid research data [13, 19, 29]. In addition, our data are not subject to the possible patient selection biases or cluster effects that may have influenced previous investigations. In Germany, about 85% of the population are insured in public mandatory health insurances. Our data were derived from one large statutory health insurance fund. Consequently, patient selection bias is not a concern. Our data may be affected by a regional bias because our sickness funds insure patients in only two German states. However, due to the uniform health insurance system in Germany, we do not expect that this potential bias may systematically influence our study results.
Third, the grace periods we defined in determining non-persistence (180 days as main scenario, 90 days as sensitivity analysis in scenario 2) are in accordance with practice documented in the adherence and persistence literature [16, 22, 23, 38]. We used 180 days as main scenario, because it is a relatively conservative estimate that expresses the possibility of prescribing a very low VKA dosage that may be common in elderly VKA patients. With a gap of 90 days, we additionally generated a tighter approach in a sensitivity analysis. To address a potential limitation due to fixed periods, we analyzed non-persistence in another two sensitivity scenarios with more flexible grace periods: the same number of days’ coverage of the last prescription (DDD) (scenario 3) and twice the coverage of the last prescription (2*DDD) (scenario 4). The results confirmed our previous results: discontinuation rates in the different scenarios were even higher than in the main analysis.
Fourth, our definition of VKA treatment-naive patients (two quarters’ grace period without any VKA prescriptions) may over-estimate the number of these patients, because some patients may have received VKA prescriptions at earlier points in time. Therefore, we conducted a sensitivity analysis with a four quarters’ pre-index period. The patient characteristics and results for the persistence analysis were comparable to the standard definition (see Tables 1 and 2).
Conclusions
Non-persistence related to VKA therapy is common in AF patients. Older more comorbid patients as well as patients who receive NSAIDs and who do not visit a cardiologist regularly face a higher therapy discontinuation risk. These patient groups should receive special attention regarding their VKA treatment.
References
Heeringa J, van der Kuip DAM, Hofman A et al (2006) Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam study. Eur Heart J 27(8):949–953. doi:10.1093/eurheartj/ehi825
Schnabel RB, Sullivan LM, Levy D et al (2009) Development of a risk score for atrial fibrillation (Framingham Heart Study): a community-based cohort study. Lancet 373(9665):739–745. doi:10.1016/S0140-6736(09)60443-8
Fang MC, Go AS, Chang Y et al (2008) Comparison of risk stratification schemes to predict thromboembolism in people with nonvalvular atrial fibrillation. J Am Coll Cardiol 51(8):810–815. doi:10.1016/j.jacc.2007.09.065
Lip GYH, Laroche C, Ioachim PM et al (2014) Prognosis and treatment of atrial fibrillation patients by European cardiologists: one year follow-up of the EURObservational Research Programme-Atrial Fibrillation General Registry Pilot Phase (EORP-AF Pilot registry). Eur Heart J 35(47):3365–3376. doi:10.1093/eurheartj/ehu374
Fuster V, Ryden LE, Cannom DS et al (2011) 2011 ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation 123(10):e269–e367. doi:10.1161/CIR.0b013e318214876d
Lip GYH, Rudolf M, Kakar P (2007) Management of atrial fibrillation: the NICE guidelines. Int J Clin Pract 61(1):9–11. doi:10.1111/j.1742-1241.2006.01151.x
You JJ, Singer DE, Howard PA et al (2012) Antithrombotic therapy for atrial fibrillation: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141(2 Suppl):75. doi:10.1378/chest.11-2304
Kirchhof P, Benussi S, Kotecha D et al (2016) 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J 37(38):2893–2962. doi:10.1093/eurheartj/ehw210
Nieuwlaat R, Capucci A, Lip GYH et al (2006) Antithrombotic treatment in real-life atrial fibrillation patients: a report from the Euro Heart Survey on Atrial Fibrillation. Eur Heart J 27(24):3018–3026. doi:10.1093/eurheartj/ehl015
Mohammed MA, Marshall T, Nirantharakumar K et al (2013) Patterns of warfarin use in subgroups of patients with atrial fibrillation: a cross-sectional analysis of 430 general practices in the United Kingdom. PLoS One 8(5):e61979. doi:10.1371/journal.pone.0061979
Kirchhof P, Ammentorp B, Darius H et al (2014) Management of atrial fibrillation in seven European countries after the publication of the 2010 ESC guidelines on atrial fibrillation: primary results of the PREvention oF thromboemolic events--European Registry in Atrial Fibrillation (PREFER in AF). Europace 16(1):6–14. doi:10.1093/europace/eut263
Deitelzweig SB, Buysman E, Pinsky B et al (2013) Warfarin use and stroke risk among patients with nonvalvular atrial fibrillation in a large managed care population. Clin Ther 35(8):1201–1210. doi:10.1016/j.clinthera.2013.06.005
Wilke T, Groth A, Mueller S et al (2012) Oral anticoagulation use by patients with atrial fibrillation in Germany. Adherence to guidelines, causes of anticoagulation under-use and its clinical outcomes, based on claims-data of 183,448 patients. Thromb Haemost 107(6):1053–1065. doi:10.1160/TH11-11-0768
Wilke T, Groth A, Pfannkuche M et al (2015) Real life anticoagulation treatment of patients with atrial fibrillation in Germany: extent and causes of anticoagulant under-use. J Thromb Thrombolysis 40(1):97–107. doi:10.1007/s11239-014-1136-8
Zalesak M, Siu K, Francis K et al (2013) Higher persistence in newly diagnosed nonvalvular atrial fibrillation patients treated with dabigatran versus warfarin. Circ Cardiovasc Qual Outcomes 6(5):567–574. doi:10.1161/CIRCOUTCOMES.113.000192
Suh D-C, Choi JC, Schein J et al (2013) Factors associated with warfarin discontinuation, including bleeding patterns, in atrial fibrillation patients. Curr Med Res Opin 29(7):761–771. doi:10.1185/03007995.2013.795142
Song X, Sander SD, Varker H et al (2012) Patterns and predictors of use of warfarin and other common long-term medications in patients with atrial fibrillation. Am J Cardiovasc Drugs 12(4):245–253. doi:10.2165/11632540-000000000-00000
Hansen CM, Olesen JB, Hansen ML et al (2012) Initiation and persistence with warfarin therapy in atrial fibrillation according to ethnicity. Front Pharmacol 3:123. doi:10.3389/fphar.2012.00123
Gallagher AM, Rietbrock S, Plumb J et al (2008) Initiation and persistence of warfarin or aspirin in patients with chronic atrial fibrillation in general practice: do the appropriate patients receive stroke prophylaxis? J Thromb Haemost 6(9):1500–1506. doi:10.1111/j.1538-7836.2008.03059.x
Lip GYH (2011) Implications of the CHA(2)DS(2)-VASc and HAS-BLED scores for thromboprophylaxis in atrial fibrillation. Am J Med 124(2):111–114. doi:10.1016/j.amjmed.2010.05.007
WHO Collaborating Centre for Drug Statistics Methodology (2010) Guidelines for ATC classification and DDD assignment: 2011. Norwegian Institute of Public Health, Oslo
Forslund T, Wettermark B, Hjemdahl P (2016) Comparison of treatment persistence with different oral anticoagulants in patients with atrial fibrillation. Eur J Clin Pharmacol 72(3):329–338. doi:10.1007/s00228-015-1983-z
Fang MC, Go AS, Chang Y et al (2010) Warfarin discontinuation after starting warfarin for atrial fibrillation. Circ Cardiovasc Qual Outcomes 3(6):624–631. doi:10.1161/CIRCOUTCOMES.110.937680
Chae J-W, Song CS, Kim H et al (2011) Prediction of mortality in patients undergoing maintenance hemodialysis by Charlson Comorbidity Index using ICD-10 database. Nephron Clin Pract 117(4):c379–c384. doi:10.1159/000321525
Sorensen SV, Dewilde S, Singer DE et al (2009) Cost-effectiveness of warfarin: trial versus “real-world” stroke prevention in atrial fibrillation. Am Heart J 157(6):1064–1073. doi:10.1016/j.ahj.2009.03.022
Simpson SH, Eurich DT, Majumdar SR et al (2006) A meta-analysis of the association between adherence to drug therapy and mortality. BMJ 333(7557):15. doi:10.1136/bmj.38875.675486.55
Martinez C, Katholing A, Wallenhorst C et al (2016) Therapy persistence in newly diagnosed non-valvular atrial fibrillation treated with warfarin or NOAC. A cohort study. Thromb Haemost 115(1):31–39. doi:10.1160/TH15-04-0350
Casciano JP, Dotiwala ZJ, Martin BC et al (2013) The costs of warfarin underuse and nonadherence in patients with atrial fibrillation: a commercial insurer perspective. J Manag Care Pharm 19(4):302–316. doi:10.18553/jmcp.2013.19.4.302
Beyer-Westendorf J, Ehlken B, Evers T (2016) Real-world persistence and adherence to oral anticoagulation for stroke risk reduction in patients with atrial fibrillation. Europace. doi:10.1093/europace/euv421
Bjorck F, Renlund H, Svensson PJ et al (2015) Warfarin persistence among stroke patients with atrial fibrillation. Thromb Res 136(4):744–748. doi:10.1016/j.thromres.2015.07.028
Koscielny J, Ziemer S, von Heymann C (2009) Patients with oral anticoagulation—bridging anticoagulation in the perioperative phase (Patienten unter oraler Antikoagulation—perioperatives bridging). Hamostaseologie 29(3):247–255
Siegal D, Yudin J, Kaatz S et al (2012) Periprocedural heparin bridging in patients receiving vitamin K antagonists: systematic review and meta-analysis of bleeding and thromboembolic rates. Circulation 126(13):1630–1639. doi:10.1161/CIRCULATIONAHA.112.105221
Hylek EM, Evans-Molina C, Shea C et al (2007) Major hemorrhage and tolerability of warfarin in the first year of therapy among elderly patients with atrial fibrillation. Circulation 115(21):2689–2696. doi:10.1161/CIRCULATIONAHA.106.653048
Man-Son-Hing M, Laupacis A (2003) Anticoagulant-related bleeding in older persons with atrial fibrillation: physicians’ fears often unfounded. Arch Intern Med 163(13):1580–1586. doi:10.1001/archinte.163.13.1580
Ezekowitz MD, Falk RH (2004) The increasing need for anticoagulant therapy to prevent stroke in patients with atrial fibrillation. Mayo Clin Proc 79(7):904–913. doi:10.1016/S0025-6196(11)62158-7
Wilke T, Bauer S, Mueller S et al (2016) Patient preferences for oral anticoagulation therapy in atrial Fibrillation: A Systematic Literature Review. Patient. doi:10.1007/s40271-016-0185-9
Bottger B, Thate-Waschke I-M, Bauersachs R et al (2015) Preferences for anticoagulation therapy in atrial fibrillation: the patients’ view. J Thromb Thrombolysis 40(4):406–415. doi:10.1007/s11239-015-1263-x
Lefevre C, Benhaddi H, Lacoin L et al (2015) Persistence to vitamin-K antagonists (Vka) and novel oral anticoagulants (Noacs) in non-valvular atrial fibrillation (Nvaf): an observational study using a comprehensive regional database in Catalonia, Spain. Value Health 18(7):A403. doi:10.1016/j.jval.2015.09.938
Acknowledgements
The authors would like to thank two anonymous reviewers for their valuable comments.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Contributions of authors statement
All authors made substantial contributions to all of the following: (1) the conception and design of the study, or acquisition of data, or analysis and interpretation of data; (2) drafting the article or revising it critically for important intellectual content; and (3) final approval of the version to be submitted. Specifically, the main tasks the authors were engaged in were as follows:
TW and AG: project lead, participated in writing all parts of the paper, and statistical analysis.
UM and AF: conception/design of the study, data collection, validation of database, and interpretation of results in discussion section.
MP: conception/design of the study and interpretation of results in discussion section.
Funding
The study was funded by Boehringer Ingelheim Pharma GmbH, Germany. The study design, the collection/analysis of data, and the writing of the manuscript were done independently of the funding source.
Conflict of interest
Thomas Wilke has acted as consultant for Boehringer Ingelheim Pharma, Bayer, GSK, LEO Pharma, Novartis, Sanofi-Aventis, Bristol Myers Squibb, Pfizer, and other pharmaceutical companies. Antje Groth has no conflict of interest. Matthias Pfannkuche is employed by Boehringer Ingelheim Pharma (Germany). Ulf Maywald and Andreas Fuchs work for the insurance fund that provided the study data (AOK PLUS).
Electronic supplementary material
Supplemental Table A
(DOCX 51 kb).
Supplemental Table B
(DOCX 50 kb).
Rights and permissions
About this article
Cite this article
Wilke, T., Groth, A., Fuchs, A. et al. Persistence with VKA treatment in newly treated atrial fibrillation patients: an analysis based on a large sample of 38,076 German patients. Eur J Clin Pharmacol 73, 1437–1447 (2017). https://doi.org/10.1007/s00228-017-2307-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-017-2307-2