Abstract
Since the introduction of new oral anticoagulants (NOACs), besides vitamin-K antagonists, an additional option for stroke prevention of patients with atrial fibrillation (AF) is available. The objective of this study was to assess AF patients’ preferences with regard to the attributes of these different treatment options. We conducted a multicenter study among randomly selected physicians. Preferences were assessed by computer-assisted telephone interviews. We used a discrete-choice-experiment (DCE) with four convenience-related treatment dependent attributes (need of bridging: yes/no, interactions with food/nutrition: yes/no, need of INR controls/dose adjustment: yes/no; frequency of intake: once/twice daily) and one comparator attribute (distance to practitioner: <1 km/>15 km). Preferences measured in the interviews were analyzed descriptively and based on a conditional logit regression model. A total of 486 AF patients (age: 73.9 ± 8.2 years; 43.2 % female; mean CHA2DS2-VASc: 3.7 ± 1.6; current medication: 48.1 % rivaroxaban, 51.9 % VKA) could be interviewed. Regardless of type of medication, patients significantly preferred the attribute levels (in order of patients’ importance) “once daily intake” (Level: once = 1 vs. twice = 0; Coefficient = 0.615; p < 0.001), “bridging necessary” (yes = 1 vs. no = 0; −0.558; p < 0.001), “distance to practitioner of ≤1 km (>15 km = 0 vs. ≤1 km = 1; 0.494; p < 0.001), “interactions with food/nutrition” (yes = 1 vs. no = 0; −0.332; p < 0.001) and “need of INR controls/dose adjustment” (yes = 1 vs. no = 0; −0.127; p < 0.001). In our analyses, “once daily frequency of intake” was the most important OAC-attribute for patients’ choice followed by “no bridging necessary” and “no interactions with food/nutrition”. Thus, patients with AF seem to prefer treatment options which are easier to administer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Atrial fibrillation (AF) is the most common cardiac disorder with a prevalence of 1–3 % in the general population [1–7]. Incidence and prevalence of AF are expected to increase in most countries in the next years [5–8]. AF-patients have been reported to be at high risk for debilitating clinical sequelae, such as heart failure and thromboembolic events [8, 9]. Especially the risk of ischemic strokes is up to fivefold higher than in the general population [6, 8–10]. Current AF-guidelines recommend assessment of thromboembolic event/stroke risk and, given a certain risk exists in a patient, recommend long term anticoagulation treatment [7, 11]. As instruments to assess AF-patients’ stroke risk, the CHADS2-score [12] or the CHA2DS2-VASc-score have been recommended [13]. Based on these, patients with a CHADS2/CHA2DS2-VASc score ≥2 are at high risk for stroke and should, consequently, receive oral anticoagulation (OAC), patients with a score of 1 may receive an OAC treatment [7, 11].
For several decades, vitamin-K-antagonists (VKAs) have been the only OAC treatment option for AF patients. However, VKAs do have well-known weaknesses, including necessary dosing adjustments in conjunction with regular INR value monitoring, drug/food interactions or the need of periprocedural interruption (bridging), which may be associated with a substantial burden to patients [14]. That may also be one of the explanations for the high percentage of patients still not treated by OAC despite its well-known benefits [15–17].
Novel oral anticoagulants (NOACs) are a relatively new additional option for stroke prevention of AF patients which are at least as effective/safe as VKA treatment [18–20]. However, former studies indicate that there may exist a difference in patient perception with regard to the mentioned treatment options [14, 21, 22]. This is of particular importance because, inherently, every treatment should be centred on the patient. Moreover, clinical guidelines recommend to take into account an AF patient’s view and preference when deciding on the options of OAC therapy [7, 11, 23]. It is therefore necessary to collect reliable and valid data on patients’ preferences when providing treatments. This is most relevant in the long-term treatment for chronic diseases like AF because patient preferences may influence the long-term adherence of patients and, consequently, the real-world effectiveness of a treatment. Moreover, prescribing treatments patients prefer may also generally strengthen the relationship between the physician and the patient.
However, little is known about patients’ preferences with regard to OAC therapy for AF patients. Most of the former studies assessed patient views on the differences of a VKA compared to an ASS therapy [24–26]. Only one known previous study directly addressed the attributes of a VKA therapy versus a NOAC therapy [21]. However, it included hypothetical trade-off safety/efficacy profiles of these drugs which do not correspond with the choices physicians face in real-life practice. Moreover, it included a small sample of respondents from the general public instead of AF patients only. As a result, in this study respondents preferred those treatments with a better safety/efficacy profile; the role of the other patient-related properties associated with the treatment options could rarely be assessed because this experiment was dominated by efficacy/safety differences between the compared drugs [21]. Thus, data about AF patient preferences with regard to “convenience attributes” are urgently needed to facilitate the choice of OAC agents when agents are similar in terms of efficacy/safety.
Consequently, using a discrete choice experiment (DCE) design, the objective of this analysis was to assess AF patient preferences in OAC treatment and to define properties of an ideal OAC treatment from the AF patients’ perspective.
Methods
Study sample
We conducted a multicenter study among randomly selected general practitioners (GPs), outpatient specialists in internal medicine (IMs) and outpatient cardiology clinics (OCCs) in Germany. Study centers were asked to include patients consecutively according to predefined inclusion criteria as well as to obtain patients’ informed consent. Patients were eligible for study inclusion if they (a) suffered from non-valvular atrial fibrillation, (b) were at least 18 years old, (c) were able to conduct a 20 min phone interview in German language, (d) didn’t participate in another anticoagulation related study within the last 3 months, and (e) received continuous AF-related OAC therapy with either VKAs (group 1) or rivaroxaban (group 2) for at least 3 months before date of study inclusion. Sample size calculation was based on a minimum of 250 study participants in each of the two groups [27]. The study was approved by the ethics committee of the University of Greifswald, Germany.
Data collection
Basic socio-demographic and clinical characteristics of patients were documented at inclusion date by the treating physicians according to a case report form (CRF). After receiving the informed consent, patients were surveyed on the basis of a computer assisted telephone interview by trained interviewers. In addition to the DCE-related questions, patients’ AF related symptoms following the EHRA-score [8], their current health-related quality of life as measured by the SF12 [28], and some additional questions concerning patients’ social circumstances were asked (supplementary table A).
Discrete choice experiment
To assess patients’ preferences, we conducted a discrete choice experiment (DCE) as part of the phone interview. DCEs are increasingly used in health economics to address a wide range of health policy issues related to preferences of different stakeholders [29]. The main reason to apply a technique like a DCE is that simply asking patients to rate treatment-related attributes will generally yield no substantial information. Patients will state in such a survey that they want all the benefits and none of the indirect/direct costs [29]. Instead, a choice experiment like a DCE requires that patients be forced to make a trade-off between two or more options, and choosing, as it is the case in reality, between treatment options that may be associated with utility-increasing and utility-decreasing attribute levels [30].
The basic assumption of a DCE is that rational individuals will always choose the alternative with the higher level of expected utility. In this framework, patients assess the utility that is associated with a treatment option from its attributes or levels of attributes, which can be the efficacy/safety relation, but also other treatment-specific properties like frequency of intake, necessary monitoring associated with the treatment etc. Specifically, in a DCE patients are asked to make a number of stated preference choices in deciding between at least two alternative treatment options. Each of these treatment options can be characterized by specific levels of attributes. Afterwards, data obtained from respondent’s stated preferences can be analyzed using multifactor regression models, mainly logit and/or probit models [29, 30]. If the specified attributes are significantly related to respondents’ choices, results should show how the average patient’s utility is affected by changes in the levels of attributes.
Our DCE was done in two stages: first, in a qualitative study, the DCE questionnaire was developed. In a second step, after a pre-test with 10 patients, a quantitative study to elicit patient preferences was conducted.
In the qualitative part, an expert board of clinical as well as health-economic experts discussed which attributes/attribute levels should be included in the DCE. Based on seven potential attributes, finally four treatment-dependent attributes (levels in brackets) were included: (i) need of bridging (yes/no), (ii) interactions with food/nutrition (yes/no), (iii) need of regular INR/blood controls and subsequent dose adjustment (yes/no), and (iv) frequency of intake (once/twice daily). The attributes were described according to the details in the summary of product characteristics of available VKA/NOAC treatments [31, 32]. Even though that the NOACs so far tested in clinical trials have all shown non-inferiority compared with VKAs, with better safety, consistently limiting the number of intracranial hemorrhage [18–20], efficacy/safety of the treatments as attributes were not included because the efficacy and safety profile of each respective OAC also depends on the clinical features of the patient and these attributes could not be generalized to all patient populations equally and were thus deemed for the purposes of the implemented DCE not to be adequate.
To be able to express patients’ overall utility in terms of a comprehensible unity, we added (v) distance to treating practitioner as additional DCE attribute (1 km/15 km distance). We decided against out-of-pocket costs because German patients are not used to substantial co-payments. As for every attribute two levels were assigned, this resulted in 64 (26) possible treatment combinations.
As outlined, patients were asked to choose between two treatment options in a series of choices. The standard software SPSS was used to create a fractional factorial design that reduced the required number of choice sets to ten, including eight design and two holdout sets. Finally, we used the shifted-design technique to allocate alternative attribute levels to create the choice sets [26].
The choice sets were graphically visualized and printed; as an example of one of the ten choice sets, see Fig. 1. Preliminary to the phone interview, the sets were sent to the participating patients by mail so that patients had all the choice sets available in a physical form.
Example of a used discrete-choice set: The figure shows an example of the visualization of the applied choice sets. Both options include the same attributes “need of bridging while undergoing surgery”, “need of INR controls by regular blood tests and subsequent dose adjustment”, “interactions with diet/nutrition or alcohol”, “frequency of dosing” and “distance to prescribing practitioner” but differ with regard to attribute levels (fold over design). Patients were asked to decide between option A or B (without opt out)
The pre-test included 10 patients. The aim was to make sure that patients understood the choices they were facing and to ensure content validity, i.e. the accuracy of the attributes and attribute levels. Based on this, the final questionnaire did not require any changes in comparison to the pre-tested version.
Analyses
Choice data were modelled using a random utility maximization framework. In a conditional logit regression model, effects of different attribute levels on the probability of a patient’s decision to choose the specific alternative were estimated. All in all, eleven different models were estimated for all patients (model 1), patients treated with rivaroxaban or VKAs (models 2/3), male/female patients (models 4/5), older/younger patients (using a threshold of 70 years; models 6/7), patients with low/high physical health-related quality of life (median threshold of a SF 12-physical summary score PSC = 41.1; models 8/9), and patients with low/high mental health-related quality of life (median threshold of a SF 12 mental health summary score MSC = 56.0; models 10/11).
In an additional analysis, utility values attributable to each attribute level were estimated using a conditional logit regression model. Based on this, marginal willingness to accept a given distance to a practitioner if a specific treatment with a more favorable attribute level could be received was calculated. Finally, in the mentioned patient groups, relative importance of each attribute for the overall decision for/against an OAC treatment option was calculated.
For quantitative variables, mean, median and standard deviation were reported. For non-metric parameters, the number of patients within a specific category was presented as percentage (%). If a patient did not respond to all 10 choice questions and to all other questions in the questionnaire, the patient was entirely excluded from the dataset. So, no data imputation was conducted. Potential statistical differences were tested for significance using Pearson’s Chi Squared test for nominal variables and Mann–Whitneys’ U test for continuous variables. All analyses were performed using IBM’s SPSS 20.0 software.
Results
Study sample
Between January and October 2014, 647 patients with non-valvular AF were included by 57 practitioners (84.2 % GPs; 14.0 % IMs; 1.8 % OCAs). Of these, 486 patients (75.1 %) with a mean age of 73.9 ± 8.2 years and a proportion of female patients of 43.2 % completed the DCE related telephone interview which took place between January and October 2014 (Table 1). When comparing finally included patients with those who were excluded, patient characteristics differed significantly with regard to age, duration of atrial fibrillation and number of patients with unknown type of AF (Table 1).
Of the final DCE participants, 234 (48.1 %) patients received a rivaroxaban treatment and 252 patients received a VKA treatment, respectively. Patients on rivaroxaban had a shorter OAC therapy experience (−2.8 years), did suffer more often from paroxysmal AF (+13 %-points) and less often from permanent AF (−15 %-points), did receive a lower number of concomitant long term medications (−0.6), did suffer less frequently from chronic heart failure (−11 %-points) within the last 5 years, suffered more often from dementia (+2.1 %-points) and had received more cardiovascular interventions within the last 24 months (+0.1 interventions).
Patients’ preferences based on the DCE
Table 2 shows the results of the conditional logit regression model, evaluating the influence of tested attribute levels on patients’ preferences. In the overall cohort of 486 patients, influence of selected attributes on preferences was statistically significant for all attributes. Generally, patients preferred the attribute levels “no bridging”, “no need of INR control/dose adjustment”, “no interactions with food/nutrition”, “once daily intake” and “low distance to practitioner <1 km”. Only the attribute “INR control/dose adjustment” was associated with inconclusive results. Treatment options with a need for INR controls/dose adjustments were less likely to be chosen as a treatment option in the whole sample as well as in the subgroups of patients treated with rivaroxaban, those aged >70 years and those having a higher mental/physical quality of life. In all other subgroups, influence of this attribute did not reach high significance, defined as p < 0.01.
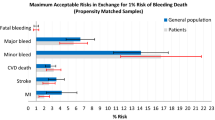
These results are reflected in the assessment of the approximate relative importance of the attributes on patients’ preferences/choices (Fig. 2), defined as percentage to which a certain attribute influenced the overall choice by patients. In the whole sample as well as in all observed subgroups except of female patients/patients treated with rivaroxaban, “INR control/dose adjustment” was the attribute with the overall lowest impact on patients’ preferences (6 % in the whole sample). Contrary to this, the attribute “frequency of intake” was the most important attribute for patients’ choices (29 % in the whole sample), followed by “need of bridging” (26 %), distance to practitioner (23 %), and “interactions with nutrition” (16 %).
Relative importance of each attribute for AF patients’ choices (whole sample and subgroups): In the whole sample, “frequency of intake” was the most important attribute for patients’ choices (29 %), followed by “need of bridging”, “distance to practitioner”, “interactions with nutrition” and “INR control/dose adjustment”
When comparing the two subgroups of patients having been treated with either rivaroxaban or VKA, patients’ preferences were generally similar: For rivaroxaban patients the order of importance of the attributes was (from most to least important attribute): “bridging” with preference for “no bridging”, “frequency of intake” with preference for “once daily”, “INR control” with preference for “no INR control”, “distance to practitioner” with preference for “<1 km distance” and “interactions with food/nutrition” with preference for “no interactions”. For VKA patients, the order was “distance to practitioner” with preference for “<1 km distance”, “frequency of intake” with preference for “once daily”, “bridging” with preference for “no bridging”, “interactions with food/nutrition” with preference for “no interactions” and “INR control/dose adjustments” with inconclusive preferences.
Utility analyses
Table 3 shows the results of the estimation of patients’ utilities for the four product-dependent attributes. In this table, we translated negative utility associated with a higher distance to a practitioner into a “willingness to accept” this longer distance to receive a treatment with more favorabe attributes. So, this “willingness to accept” was shown as additional distance in km a patient would accept if he would receive a treatment option with more favorable, utility-increasing treatment attribute levels. Based on the whole sample, participating patients were willing to accept (compared to the less favored attribute level) an additional distance of 17.7 km if the OAC would need to be taken just once a day, an additional distance of 16.1 km to the practitioner if the OAC treatment did not need to be bridged, an additional distance of 9.6 km if the anticoagulant wouldn’t have limitations regarding nutrition/food interactions, and an additional distance of 3.7 km if no INR controls would be necessary. When transferring these findings to currently available treatment options, rivaroxaban treatment is preferred by patients. In order to get a rivaroxaban-based treatment that can be described by the tested attribute levels, patients would be willing to accept an additional distance of 29.3 km to a practitioner in comparison to a VKA treatment. Compared to a hypothetical dabigatran/apixaban treatment that needs to be administered twice a day, rivaroxaban (needs to be administered once a day) was associated with a positive utility equal to an additional distance of 17.7 km to the practitioner.
Discussion
Using a DCE design, the objective of this analysis was to assess AF patient preferences in OAC treatment and to define properties of an ideal OAC treatment from the AF patients’ perspective.
AF patients seem to prefer OAC agents which are easier to administer. As expected, in ideal terms, patients would prefer a treatment that does not need to be bridged, that is not associated with regular INR controls/dose adjustments, that has less interactions with food/nutrition and can be taken once daily.
In a conditional logit regression analysis, we could show that, from a patient’s perspective, the most important “convenience” properties of a OAC treatment are the frequency of intake, followed by the potential need of bridging, the existence of interactions with food/nutrition and the need of INR controls. Our results show that patient preferences are relatively stable among different patient groups. However, some differences could be observed. Patients with a low physical/mental quality of life are indifferent with regards to the need of INR controls, VKA-patients even prefer INR controls on a low significance level. Furthermore, relative importance of attributes is different in patients treated with either rivaroxaban or VKA. For patients treated with rivaroxaban, “bridging” and “frequency of intake” are the most important attributes whereas “distance to treating practitioner” and “frequency of intake” are the most important attributes for VKA-patients. The necessity of regular INR monitoring/physician visits in the VKA group may be responsible for a preference for short distance to physicians in that patient group.
Only one study analyzed preferences in terms of OAC treatment so far [26]. However, this study of 76 respondents belonging to the general public differed in several characteristics from our study: sample size was lower, respondents did not have to suffer from AF, were 20 years younger than in our study, interviews were done as online computer-based interviews, and clinical attributes like yearly risk of stroke (between 0 and 2.4 %), yearly risk of bleeding (between 2 and 5 %), and availability of an antidote were included. The study found the efficacy/safety parameters to be the most important ones. So, based on this study, agents with a favorable efficacy/safety profile should be prescribed, which is in line with our recommendations. However, because efficacy/safety of the different OACs depends on patients’ characteristics like comorbidities, a recommendation for a treatment based on hypothetical clinical trade-off profiles is hardly possible to be generalized for AF patients. Naturally, our results do not implicate that less effective/safe treatments should be prescribed. But in case different OAC treatment options do have a similar efficacy/safety profile in a specific patient, our approach identified attribute levels applicable to all AF patients that may influence the decision for/against a specific OAC agent. Doing so would also ensure that the prescribed treatment is in line with patients’ preferences, which may also improve the level of adherence/persistence to treatment and strengthen the patient-physician relationship.
Because of a different methodological framework, comparison of our results with more descriptive/qualitative studies addressing certain treatment attributes without taking into effect any trade-offs is difficult. Nevertheless, previous studies already reported an association between current treatment experience and preferences [33, 34]; the differences in preferences between VKA patients and rivaroxaban patients confirm that. Also, low importance of INR controls for VKA-treated AF patients’ preferences was already found in studies [21, 35]. In these studies, it was reported that some patients interpreted INR controls as reassuring because favorable INR values proved that the OAC works, while other patients experienced INR controls as inconvenient.
However, the importance of the frequency of intake of an anticoagulant has not been analyzed so far. Our data show the high importance of this attribute for patient preferences and a clear preference for a once-daily regimen. This may also be one of explanations why once-daily regimens in other diseases have been found to be associated with a higher treatment adherence; in one review addressing cardiovascular medication, once-daily regimens were associated with a 6.9–14.0 % higher adherence compared to twice daily regimens [36].
Our findings are important for the real-life treatment of AF patients. As it was reported by Choi et al., only 24.5–36.9 % of AF patients participated on the decision about anticoagulation in advance of their treatment [37]. In contrast to that, in another study, it has been reported that 89 % of AF patients would like to be involved in decision making [38]; this is also reflected in different treatment guidelines [7, 11, 23]. Obviously, patient preferences matter. Our analysis shows that AF patients rate different OAC treatment attributes in a consistent way and associate different utilities with different attribute levels. That should be known to physicians and should be taken into account when deciding about the prescribed OAC treatment.
Limitations
We acknowledge certain limitations. First, attributes used in our study were derived based on expert opinion without qualitative assessment by patients. However, we derived our attributes from previous studies having found that these attributes are important to patients. Second, despite random selection of study centers with consecutive patient inclusion, there might be a substantial selection bias arising from physician/patient inclusion. So, physicians with an above-average treatment quality may be more willing to participate in such a study. However, we do not believe that treatment quality is a major driver of patient preferences towards alternative anticoagulants.
Third, we were only able to conduct the computer assisted phone interview for 75.1 % of initially enrolled patients leading to a potential response bias. Excluded patients were slightly younger (−0.3 years) and had a shorter duration of AF (−0.5 years). In terms of age, older patients had a strong preference for no INR controls in comparison to younger patients in our analysis (Table 2). So, we may have underestimated patients’ preferences towards a treatment without INR controls.
Fourth, we only included patients on either VKA or rivaroxaban treatment leading to exclusion of patients receiving other anticoagulants. However, the DCE is a hypothetical framework enabling patients to vote for attributes of anticoagulants they are not experienced in. That was also true for VKA-treated patients in case they evaluated attribute levels associated with rivaroxaban and vice versa.
Fifth, a DCE could be perceived as a complex way to gather information both for patients to understand and for interviewers to conduct. However, we trained interviewers intensively and supported them by visualizing choice sets as well as by a guideline on how to create a hypothetical ambience.
Sixth, the alternative attributes we have chosen are only convenience attributes. Former studies have shown that patients’ preferences are affected by efficacy and/or safety outcomes as well [21, 33, 34]. However, as outlined already, most NOACs have shown to be non-inferior to VKA treatment. Moreover, efficacy/safety of OAC with the available agents depends on patient characteristics like comorbidities [18–20]. We do not question the fact that these differences should be a major driver of the decision for/against a treatment. However, we also think that patient preferences as shown in our analysis should play a certain role, especially if a physician chooses between treatment options that are not different from each other in terms of efficacy/safety.
Conclusion
When deciding about an anticoagulation treatment, AF patients prefer treatments that can be taken once daily, that do not require any bridging in case of surgeries, and do not have interactions with food/nutrition. Frequency of intake is the most important attribute from a patient’s perspective with once daily intake preferred compared to twice daily intake. Treating physicians should take patient preferences into account as an additional factor besides clinical efficacy/safety because a treatment that is preferred by patients may also be a more effective one in a real-world environment.
References
Ryder KM, Benjamin EJ (1999) Epidemiology and significance of atrial fibrillation. Am J Cardiol 84(9A):131R–138R
Chugh SS, Blackshear JL, Shen WK et al (2001) Epidemiology and natural history of atrial fibrillation: clinical implications. J Am Coll Cardiol 37(2):371–378
Chien KL, Su TC, Hsu HC et al (2010) Atrial fibrillation prevalence, incidence and risk of stroke and all-cause death among Chinese. Int J Cardiol 139(2):173–180
Fang MC, Go AS, Chang Y et al (2008) ATRIA Study Group. Comparison of risk stratification schemes to predict thromboembolism in people with nonvalvular atrial fibrillation. J Am Coll Cardiol 51(8):810–815
Wilke T, Groth A, Mueller S et al (2013) Incidence and prevalence of atrial fibrillation: an analysis based on 8.3 million patients. Europace 15(4):486–493
Davis RC, Hobbs FD, Kenkre JE et al (2012) Prevalence of atrial fibrillation in the general population and in high-risk groups: the ECHOES study. Europace 14:1553–1559
Camm AJ, Kirchhof P, Lip GY et al (2010) Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Eur Heart J 31:2369–2429
Kirchhof P, Auricchio A, Bax J et al (2007) Outcome parameters for trials in atrial fibrillation: executive summary. Recommendations from a consensus conference organized by the German Atrial Fibrillation Competence NETwork (AFNET) and the European Heart Rhythm Association (EHRA). Eur Heart J 28:2803–2817
Stewart S, Hart CL, Hole DJ et al (2002) A population-based study of the long-term risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/Paisley study. Am J Med 113:359–364
Friberg L, Hammar N, Rosenqvist M (2010) Stroke in paroxysmal atrial fibrillation: report from the Stockholm Cohort of Atrial Fibrillation. Eur Heart J 31:967–975
Halperin JL, Kay GN, Le Huezey JY et al (2011) ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation 123:e269–e367
Gage BF, Waterman AD, Shannon W et al (2001) Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA 285(22):2864–2870
Lip GY, Nieuwlaat R, Pisters R et al (2010) Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the Euro Heart Survey on atrial fibrillation. Chest 137:263–272
Fumagalli S, Cardini F, Roberts AT et al (2014) Psychological effects of treatment with new oral anticoagulants in elderly patients with atrial fibrillation: a preliminary report. Aging Clin Exp Res
Ogilvie IM, Newton N, Welner SA et al (2010) Underuse of oral anticoagulants in atrial fibrillation: a systematic review. Am J Med 123(7):638–645
Wilke T, Groth A, Pfannkuche M et al (2014) Real life anticoagulation treatment of patients with atrial fibrillation in Germany: extent and causes of anticoagulant under-use. J Thromb Thrombol
Wilke T, Groth A, Mueller S et al (2012) Oral anticoagulation use by patients with atrial fibrillation in Germany. Adherence to guidelines, causes of anticoagulation under-use and its clinical outcomes, based on claims-data of 183,448 patients. Thromb Haemost 107(6):1053–1065
Connolly SJ, Ezekowitz MD, Yusuf S et al (2009) Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 361(12):1139–1151
Patel MR, Mahaffey KW, Garg J et al (2011) Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med 365(10):883–891
Granger CB, Alexander JH, McMurray JJ et al (2011) Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med 365(11):981–992
Ghijben P, Lancsar E, Zavarsek S (2014) Preferences for oral anticoagulants in atrial fibrillation: a best-best discrete choice experiment. Pharmacoeconomics 32(11):1115–1127
Bakhai A, Sandberg A, Mittendorf T et al (2013) Patient perspective on the management of atrial fibrillation in five European countries. BMC Cardiovasc Disord 13:108
Jones C, Pollit V, Fitzmaurice D et al (2014) The management of atrial fibrillation: summary of updated NICE guidance. BMJ 348:g3655
Man-Son-Hing M, Gage BF, Montgomery AA et al (2005) Preference-based antithrombotic therapy in atrial fibrillation: implications for clinical decision making. Med Decis Making 25(5):548–559
Gage BF, Cardinalli AB, Owens DK (1998) Cost-effectiveness of preference-based antithrombotic therapy for patients with nonvalvular atrial fibrillation. Stroke 29(6):1083–1091
Protheroe J, Fahey T, Montgomery AA et al (2000) The impact of patients’ preferences on the treatment of atrial fibrillation: observational study of patient based decision analysis. BMJ 320(7246):1380–1384
Johnson RF, Orme BK (2010) Sample size issues for conjoint analysis. Orme BK, Getting started with conjoint analysis: strategies for product design and pricing research. Research Publishers, Madison, pp 57–66
Ware JE, Kosinski M, Keller SD (1996) A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 34(3):220–233
Clark MD, Determann D, Petrou S et al (2014) Discrete choice experiments in health economics: a review of the literature. Pharmacoeconomics 32(9):883–902
Reed Johnson F, Lancsar E, Marshall D et al (2013) Constructing experimental designs for discrete-choice experiments: report of the ISPOR Conjoint Analysis Experimental Design Good Research Practices Task Force. Value Health 16(1):3–13
Hoffmann-La Roche AG (2004) Summary of product characteristics (SmPC) of Marcumar. https://www.klinikum.uni-heidelberg.de/fileadmin/medizinische_klinik/Abteilung_3/pdf/ivandic/FI_marcumar.pdf. Accessed 14 October 2013
Bayer Pharma AG (2011) Summary of product characteristics (SmPC) of Xarelto. http://www.coliquio.de/images/infocenter/upload/xarelto/Fachinfo_Xarelto_20_mg_Filmtabletten.pdf. Accessed 14 October 2013
MacLean S, Mulla S, Akl EA et al (2012) Patient values and preferences in decision making for antithrombotic therapy: a systematic review: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141(2 Suppl):e1S–e23S
Moia M, Mantovani LG, Carpenedo M et al (2013) Patient preferences and willingness to pay for different options of anticoagulant therapy. Intern Emerg Med 8(3):237–243
Borg Xuereb C, Shaw RL, Lane DA (2012) Patients’ and health professionals’ views and experiences of atrial fibrillation and oral-anticoagulant therapy: a qualitative meta-synthesis. Patient Educ Couns 88(2):330–337
Coleman CI, Roberts MS, Sobieraj DM et al (2012) Effect of dosing frequency on chronic cardiovascular disease medication adherence. Curr Med Res Opin 28(5):669–680
Choi JC, Dibonaventura MD, Kopenhafer L et al (2014) Survey of the use of warfarin and the newer anticoagulant dabigatran in patients with atrial fibrillation. Patient Prefer Adherence 8:167–177
Palacio AM, Kirolos I, Tamariz L (2015) Patient values and preferences when choosing anticoagulants. Patient Prefer Adherence 9:133–138
Acknowledgments
This study was financed by Bayer Vital GmbH, Germany.
Disclosure
Björn Böttger worked for IPAM until 31st of March 2015. Prof. Dr. Thomas Wilke has acted as consultant for different pharmaceutical companies, e.g. Novo Nordisk, Glaxo Smith Kline, Bayer, Bristol-Myers Squibb, Sanofi-Aventis. Dr. Inga-Marion Thate Waschke works for Bayer Vital GmbH, Germany. Prof. Dr. Rupert Bauersachs has acted as consultant for Boehringer Ingelheim Pharma, Bayer and Bristol-Myers Squibb. Prof. Dr. Thomas Kohlmann received consultancy fees, project funding and reimbursement of travel costs from different pharmaceutical companies, e.g. Bayer, Hexal, Lilly, Pfizer, Sanofi-Aventis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Statement of human rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
11239_2015_1263_MOESM1_ESM.pdf
Content of the conducted computer assisted phone interview: interviews were done in German; here an English translation is provided (PDF 359 kb)
Rights and permissions
About this article
Cite this article
Böttger, B., Thate-Waschke, IM., Bauersachs, R. et al. Preferences for anticoagulation therapy in atrial fibrillation: the patients’ view. J Thromb Thrombolysis 40, 406–415 (2015). https://doi.org/10.1007/s11239-015-1263-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-015-1263-x