Abstract
Purpose
Underreporting is a major limitation of spontaneous reporting systems for suspected adverse drug reactions (ADRs). Several interventions to increase the ADR reporting rate have been proposed, but their efficacy remains poorly investigated.
Methods
This was a questionnaire study aimed at assessing the knowledge, attitudes, and behavior of general practitioners (GPs) regarding ADR reporting and at evaluating whether a monthly e-mail-based newsletter on drug safety could affect the rate and the quality of the ADR reports submitted by these GPs. Three local health authorities (LHAs) of the Emilia–Romagna region were chosen on the basis of their ADR reporting rate during the period preceding the study: Rimini (high), Ferrara (average), and Piacenza (low reporting rate). All GPs (n = 737) associated with these three LHAs were recruited. The pooled number of ADR reports sent by GPs in the remaining seven LHAs of the region was used as controls. The study covered a period of 3 years and was divided into: (1) identification of the reasons leading to underreporting through a questionnaire (Phase I); (2) the intervention, i.e., sending a newsletter for a 10-month period (Phase II); (3) evaluation of the intervention outcomes during the 10 months following the period in which the newsletter had been received (Phase III).
Results
Among GPs involved, 22.8 % returned the questionnaire. Over 94 % of the respondents considered the spontaneous reporting of suspected ADRs to be part of their professional obligations, but only 6.5 % had submitted at least one report in the previous 6 months. Following the completion of Phase II, the overall number of reports coming from the LHAs subjected to the intervention rose by 49.2 % compared to 2009, while the number of reports coming from the control LHAs increased by 8.8 %. Rimini and Piacenza showed a 200 % increase in the number of ADR reports submitted by GPs, while the number of ADR reported submitted by the control group decreased by 25.5 %. In 2011, the number of overall ADRs reports from the LHAs subjected to the intervention decreased by 6.8 %; this decrease reached 50.0 % of the GPs. Control HLAs showed an overall decline of 4.3 %, while the total number of ADRs from GPs increased by 63.3 %. Ferrara was excluded from the analysis due to confounding factors.
Conclusions
The periodic e-mail update on the safety of drugs represents an effective and inexpensive way to raise the awareness of GPs on the importance of spontaneous ADR reporting. Since the outcome of the intervention seemed to disappear after the intervention was stopped, there appears to be a need to adopt a policy of regular updates and educational strategies for health professionals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spontaneous reporting systems for (suspected) adverse drug reactions (ADRs) represents the cornerstone of the post-marketing surveillance of drug safety and is crucial for rapid signal detection. Such systems consist of the voluntary submission of (suspected) ADR reports by doctors, pharmacists, and other healthcare workers to local and national regulatory authorities. Due to the spontaneous character of the ADR reporting, the method has several limitations [1], the most notable of which is underreporting [2]. Underreporting reduces sensitivity because it underestimates the frequency and thereby the impact of a given ADR. In addition, it renders the system more vulnerable to selective reporting, which may introduce a serious bias [3]. Underreporting is a serious drawback of the pharmacovigilance system for several reasons, most of which have been described by Inman [4] and include complacency, i.e., the belief that very serious ADRs are well documented by the time a drug is marketed; insecurity, i.e., the belief that it is nearly impossible to determine whether a drug is responsible for a particular adverse reaction, diffidence; i.e., the belief that reporting an ADR should only be done if there is certainty that it is related to the use of a particular drug; indifference, i.e., the belief that a single case that an individual physician might observe could not contribute to medical knowledge; ignorance, i.e., the belief that it is only necessary to report serious or unexpected ADRs. Lack of time to complete the form diagnosis has also been forwarded as a factor associated with underreporting [5].
Accumulating evidence shows a significant and widespread underreporting of ADRs [6]. In a study conducted in Sweden and focused on serious and potentially fatal adverse events, the overall rate of underreporting during a period of 5 years was found to be 86 % [7]. An interesting review aimed at estimating the extent of underreporting of ADRs identified a median underreporting rate of 94 % across 37 studies [6].
Several interventions to increase ADR reporting have been proposed, including education, access to report forms in combination with verbal reminders and the distribution of a drug-safety bulletin, and detailed drug-specific feedback to the reporting doctor [8]. Some of these methods are time consuming and are associated with a considerable economic burden. Moreover, their effects may fade over time. Consequently, there is an urgent need for an easily managed but continuously up-dated method to improve ADR reporting without too much additional cost [9].
According to the current rules for ADR reporting in Italy, it is mandatory for healthcare professionals to report suspected serious and unexpected (i.e., not labeled in the Summary of Product Characteristics) ADRs to the regulatory authority. All ADRs related to vaccines and to the use of new drugs should also be reported. Despite these regulations, underreporting is a serious limitation to pharmacovigilance in Italy due to the passive of the system—i.e., the final decision to submit an ADR report ultimately depends solely on the attitude of the healthcare professional to report that suspected ADR [10].
The Emilia–Romagna Region of Italy is noted for its high spontaneous ADR reporting rate in Italy, together with the Lombardy, Veneto, and Tuscany regions. In the Emilia–Romagna region, most reports come from hospital doctors, whereas general practitioners (GPs) as a class of doctors make the lowest contribution to the system. The attitudes of Italian medical practitioners to ADR reporting have been investigated by Cosentino et al. by means of a postal questionnaire [11]. However, to the best of our knowledge, no published studies have evaluated whether sending a newsletter containing update information on drug safety to GPs on a regular basis would improve the rate at which GPs would submit ADR reports.
The aim of the study reported here was to assess the knowledge, attitudes and reporting behavior of GPs and to evaluate whether an e-mail-based monthly drug safety newsletter sent to GPs would affect the reporting of ADRs and the quality of the ADR reports among the GPs in three local health authorities (LHAs) representative of the Emilia–Romagna region.
Methods
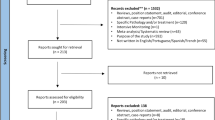
Our study covered a period of 3 years and was divided into three main phases: (1) identification of the reasons for the underreporting by the targeted doctors (Phase I); (2) intervention period (Phase II); (3) evaluation of the intervention outcomes during the first 10 months following the intervention period (Phase III) (Fig. 1).
Three LHAs were selected based on the following criteria: (1) representative of a high, average, and low number of reports submitted per 100,000 inhabitants with respect to the regional value; (2) similar number of inhabitants and doctors; (3) located in the northern, central, and southern part of the region, respectively. These three LHAs were Piacenza (northern, 3.2 reports per 100,000 inhabitants, low reporting), Ferrara (central, 10.2, average reporting), and Rimini (southern, 16.0, high reporting). All GPs in these three LHAs were recruited (n = 737). The pooled number of ADR reports from the remaining seven LHAs of the region were used as controls.
Data were collected from the official Italian spontaneous ADR reporting database, which contains all reports of suspected adverse reactions from drugs and from vaccines since 1988. About 90 % of all reports come from healthcare professionals while the remaining are sent by citizens or have been reported in the literature.
All of the participating GPs were sent a personally addressed letter of invitation and a questionnaire on October 2009. After 1 month, a reminder letter and a second copy of the questionnaire were mailed to all participating GPs. The closing date for inclusion of the data on the completed questionnaire in our study was January 2010.
The questionnaire consisted of 22 items organized in two parts. In part 1, the GP was requested to provide personal information (such as date of birth, sex, nationality, etc.) and professional information (including medical specialization and status). Part 2 comprised 14 questions that focused on collecting information on the knowledge and attitudes of the GP concerning spontaneous ADR reporting and the use of the voluntary reporting system during the last 6 months. In particular, question 16 asked why the GP failed to report ADRs, taking into account also Inman’s “seven deadly sins” (see Introduction) [4].
In question 14, respondents were also asked if they were interested in receiving a periodical bulletin on drug safety issues.
In Phase II of the survey (intervention period), a brief newsletter on drug safety was sent to all participants as an attachment to an e-mail, once a month for 10 months. This attachment listed the most important updates on safety information (warnings, international safety news, national and international drug bulletins, articles from the literature) as well as information on the spontaneous ADR reports sent by doctors involved in the study during the preceding months.
In Phase III (evaluation phase), the reporting rate and the quality of the completed reporting forms during the first 10 months following the intervention period (Phase II) were assessed. We performed a quality check of the reports produced in the period before, during and after our intervention. To this end, we checked for the presence of the items required to establish the causal relationship between the suspected drug and the reaction (Naranjo and World Health Organization algorithms). As highlighted by Bandekar et al. [12], the availability of such information on an ADR is relevant to the composing of a good ADR report as it enables a proper assessment of the causality of the adverse reaction, leading to the generation of an early safety signal.
Results
Phase I
Of the 737 GPs sent questionnaires, 168 (22.8 %) completed and returned the questionnaire; of these respondents, 23 % were women GPs. Physicians belonging to the LHA of Rimini were the most involved (28 %), followed by those from Ferrara (20.4 %) and Piacenza (17.1 %).
The mean age of the respondents (as well as of the non-respondents) was 55 years (range 41–68 years), and 74 % had graduated from medical school between 1974 and 1985 (Fig. 2).
Analysis of the returned questionnaires revealed that over 94 % of respondents considered the spontaneous reporting of ADRs to be part of their professional obligations, while approximately 60 % of them were not aware that such reports should be made even in the absence of the certainty of a causal relationship between drug and adverse reaction (Table 1). About 6.5 % (11/168) of the respondents produced at least one ADR report in the last 6 months.
Regarding question 16 (Table 2), in which GPs were asked the reasons for not reporting an ADR, 47 % of them indicated as reason as “the uncertainty that the event was caused by the drug”, while 32.7 % considered the adverse reaction “too banal to be reported”. In addition, 22 % of participants did not make reports due to a “lack of time.”
In question 18, respondents were asked about their personal knowledge of the intensive monitoring adopted by the Italian Medicines Agency (a list of new drugs periodically up-dated about which any ADR should be reported, according to Italian law 219/06). Only 48 % of the responding GPs were aware of the monitoring system. A similar fraction (47 %) believed that they did not have easy access to the ADR reporting form (Model A, which can be downloaded from the Internet site of the Italian Medicines Agency).
About 60 % of the sample were aware that in order to properly report ADRs it is necessary to consult the Summary of Product Characteristics of the medicine suspected of causing it. In addition, a majority (61 %; 102/168) correctly indicated that, in the case of drugs on the market for many years, only serious and unexpected reactions should be reported.
Among the responses concerning “other” causes for not reporting, the most frequently cited one was the lack of a quick and easy reporting system, preferably computerized.
About 10 % of respondents stated that they do not use/have regular e-mail, about 70 % expressed the wish to make the information on ADRs publicly available and about 50 % believed that the drug manufacturers’ representatives should play an important role in raising awareness of pharmacovigilance.
Finally, over 98 % of physicians declared to be interested in receiving regular information on drug safety.
Phase II
Starting on February 2010, ten issues of the newsletter (entitled “Newsletter on recent security issues of medicines—Phase II of the Regional Study on the under-reporting”) were sent to the respondents via e-mail. Together with each newsletter, we also sent the ADR reporting form.
The transmission of the newsletter was preceded by a letter to the GPs which summarized the outcomes of Phase I and presented those of Phase II together with the announcement that the newsletter would be sent by e-mail.
Phase III
The last phase of the study started in December 2010 and consisted of monitoring the trend of reporting ADRs, particularly those from GPs belonging to the LHAs involved in the study. This phase was completed at the end of November 2011.
During the analysis of the results, we excluded all data collected from the LHA of Ferrara due to a dramatic and unexpected increase (+875 %) in the number of ADR reports—from 16 reports in 2008 to 156 in 2009. The main reasons for this increase were the implementation of two other local interventions: (1) a project of monitoring the ADR related to the HPV vaccine; (2) two courses on pharmacovigilance addressed to all healthcare professionals of that LHA. Consequently, the final analysis was performed by comparing the number of reports obtained from the LHAs of Rimini and Piacenza (LHAs of intervention), taking the number of reports from the remaining LHAs as controls.
In 2010, an important increase in the number of reports (49.2 %) was observed in Rimini and Piacenza, from 63 reports in 2009 to 94 in 2010; in comparison, the remaining LHAs (controls) showed a more modest increase (8.8 %) (Table 3). With regard to the reports of GPs, the increase was 200 % for Rimini and Piacenza while in the controls there was a decrease of 25.5 %. In 2011, without any intervention, there was a turnaround compared to the previous year: the number of ADRs recorded by our LHAs showed a decrease of 6.8 %, which reached 50.0 % among the GPs. As for the controls, the data showed an overall decline of 4.3 %, while the number of reports submitted by GPs increased by 63.3 %.
The number of reports concerning vaccines sent by the GPs were as follows: Phase I, two of three ADR reports (both influenza vaccine); Phase II, two of nine (one influenza and one pneumococcal vaccines); Phase III, two of six (one influenza and one rubella vaccines).
Finally, we performed a quality check of the reports. They appeared to be of high quality in all three periods, and the increased number of reports after our intervention was not at the expense of the quality of the reporting.
Discussion
The response rate of the sample of GPs involved in this study was lower than that expected, especially considering the small size of the questionnaire, which would have required only a few minutes to complete. In a similar study conducted in the Netherlands between 2004 and 2006, the response rate was 47 % [13], while Hasford and colleagues [14], studying two samples of physicians in Germany, obtained a response rate to their mail questionnaire of 51.4 and 43.9 %, respectively.
One of the possible reasons for the low participation seen in our study may have been due to the concomitant emergence of the influenza pandemic and, therefore, to the involvement of doctors, particularly GPs, in the first line of care. This would have absorbed much of their energy and time (in particular, the monitoring of the tolerability of the vaccine through a simplified report form).
Adherence to our study did not appear to be related to the factor gender: the male/female ratio among the physicians involved and those responding remained almost unchanged.
Despite the low number of respondent GPs, our analysis of the returned questionnaires allowed us to draw a picture of the “lights and shadows” of physicians’ knowledge in general about the ADR reporting system. In fact, while almost all GPs reported believing that pharmacovigilance is crucial to increasing knowledge on the safety profile of drugs marketed, more than half of them did not know exactly how to report an adverse reaction, and a lesser percentage of physicians (6.5 %) sent only one report during the 6 months prior to receiving the questionnaire. The most frequently cited reasons support the notion that physicians in general lack knowledge of the system (afraid to report on the basis of an unfounded suspicion and possible criticism, uncertainty about the cause of the adverse reaction, etc.). Other reasons indicate a lack of time and the need for a faster and computerized system. This latter aspect was also addressed by the Italian Medicines Agency; however, there are some barriers, both technical and legal, which prevent the development of the system (for example, how to address the need for the signature of the reporter, which is currently required). Another aspect that should be highlighted is the lack of knowledge, by half of the sample, of the Intensive Monitoring system adopted by the Italian Medicines Agency. This likely means that the method of dissemination of this type of information, both at the central and regional level, are not efficient and widespread enough.
In Phase II, two different types of interventions were carried out, both of them with the aim of increasing the number of ADR reports. On the one hand, GPs were given the opportunity to acquire new information on the safety of medicines in a straightforward manner (the electronic newsletter); on the other hand, our sending of the reporting form has removed the pretext of lack of availability of the form, thus facilitating the reporting of ADRs. A study published in 2003 provides support for this method [8]. In fact, the authors of that study demonstrated that regular delivery of a newsletter with safety information is a tool that can increase the number of ADR reports. Furthermore, this increase was even higher when the reporting form was sent together with the safety bulletin. However, these authors noted that the intervention effect disappeared at the end of the study. Our data also confirm that frequent updates by means of a short bulletin can be an effective tool for raising the awareness of GPs for drug safety issues and for the usefulness of voluntary reporting. As expected, the intervention effect did disappear when the sending of the newsletter was discontinued, as confirmed by the decline in the number of reports made by GPs in 2011 compared to 2010. In the study period, our intervention did not significantly increase the number of ADR reports among GPs but at least it prevented their decline, which did occur in the LHAs in which the intervention was not performed.
Our study has a number of limitations. First, the response rate was poor (22.8 %), although a considerable number of physicians were involved. This small number may have caused a selection bias in the analysis. When GPs are asked to participate in a study on spontaneous ADR reporting, it is likely that only the most highly motivated ADR-reporters return the questionnaire. Secondly, there was no full control of the setting where the study was performed. In fact, other local initiatives in one of the three selected LHAs, just in the year before our intervention, caused a dramatic and transient rise in the rate of ADR reporting, which distorted its baseline level. This suggests that for a pragmatic study such as this one, conducted by an external academic institution, there should be good planning and concrete agreements with the local administrations. Thirdly, we do not know whether our intervention actually reached the target population. However, a randomized controlled study proved that an e-mail with an attachment on drug information may influence the sales of prescribed drugs and that no discrepancy between different designs of the attachment could be detected [15]. Finally, as stated by Figueiras et al. [16], “it is difficult to know exactly what the target number of ADRs, or percentage of physicians reporting ADRs, should be in the absence of information about the true number of adverse events that are occurring.”
Conclusion
Adverse drug reactions are a potential source of concern for doctors when they prescribe or recommend a drug. These ADRs are an important clinical problem, and far superior to what is actually received. Although the extent of underreporting is widely variable depending on the estimates, it is certain that the number of ADR reports is a minimum percentage of the total ADRs that actually do occur.
Our study shows that a periodic and continuous update on the safety of drugs may represent a particularly effective and inexpensive way to raise the awareness of the healthcare professionals on the importance of the spontaneous reporting of ADRs.
Since the positive effect of the intervention on the number of reports seemed to disappear when we stopped sending the newsletter by e-mail, there is a clear need to raise the awareness of regional and national healthcare authorities to the need to adopt constant educational/training initiatives for doctors and other healthcare professionals based on the critical aspects coming from the responses to our questionnaire. Other possible measures to stimulate GPs’ participation in an ADR reporting system could included organizing frequent courses on drug safety and pharmacovigilance linked to Continuing Medical Education (CME) credits, or providing financial incentives for the ADRs reported.
Although it is unrealistic to believe that the phenomenon of underreporting in pharmacovigilance can be completely removed, our study has shown that it is possible to contain it through training initiatives involving continuous scientific updates in order to raise the awareness of the importance of ADR reporting in the primary interest of the health of patients.
References
Li C, Xia J, Deng J, Chen W, Wang S, Jiang J, Chen G (2009) A web-based quantitative signal detection system on adverse drug reaction in China. Eur J Clin Pharmacol 65:729–741
van Puijenbroek E, Diemont W, van Grootheest K (2003) Application of quantitative signal detection in the Dutch spontaneous reporting system for adverse drug reactions. Drug Saf 26:293–301
Alvarez-Requejo A, Carvajal A, Begaud B, Moride Y, Vega T, Arias LH (1998) Under-reporting of adverse drug reactions. Estimate based on a spontaneous reporting scheme and a sentinel system. Eur J Clin Pharmacol 54:483–488
Inman WH (1996) Attitudes to adverse drug reaction reporting. Br J Clin Pharmacol 41:434–435
Herdeiro MT, Figueiras A, Polonia J, Gestal-Otero JJ (2005) Physicians’ attitudes and adverse drug reaction reporting: a case-control study in Portugal. Drug Saf 28:825–833
Hazell L, Shakir SA (2006) Under-reporting of adverse drug reactions: a systematic review. Drug Saf 29:385–396
Backstrom M, Mjorndal T, Dahlqvist R (2004) Under-reporting of serious adverse drug reactions in Sweden. Pharmacoepidemiol Drug Saf 13:483–487
Castel JM, Figueras A, Pedros C, Laporte JR, Capella D (2003) Stimulating adverse drug reaction reporting: effect of a drug safety bulletin and of including yellow cards in prescription pads. Drug Saf 26:1049–1055
Johansson ML, Brunlof G, Edward C, Wallerstedt SM (2009) Effects of e-mails containing ADR information and a current case report on ADR reporting rate and quality of reports. Eur J Clin Pharmacol 65:511–514
Motola D, Vargiu A, Leone R, Conforti A, Moretti U, Vaccheri A, Velo G, Montanaro N (2008) Influence of regulatory measures on the rate of spontaneous adverse drug reaction reporting in Italy. Drug Saf 31:609–616
Cosentino M, Leoni O, Banfi F, Lecchini S, Frigo G (1997) Attitudes to adverse drug reaction reporting by medical practitioners in a Northern Italian district. Pharmacol Res 35:85–88
Bandekar MS, Anwikar SR, Kshirsagar NA (2010) Quality check of spontaneous adverse drug reaction reporting forms of different countries. Pharmacoepidemiol Drug Saf 19:1181–1185
Passier A, ten Napel M, van Grootheest K, van Puijenbroek E (2009) Reporting of adverse drug reactions by general practitioners: a questionnaire-based study in the Netherlands. Drug Saf 32:851–858
Hasford J, Goettler M, Munter KH, Muller-Oerlinghausen B (2002) Physicians’ knowledge and attitudes regarding the spontaneous reporting system for adverse drug reactions. J Clin Epidemiol 55:945–950
Edward C, Himmelmann A, Wallerstedt SM (2007) Influence of an e-mail with a drug information attachment on sales of prescribed drugs: a randomized controlled study. BMC Clin Pharmacol 7:12
Figueiras A, Herdeiro MT, Polonia J, Gestal-Otero JJ (2006) An educational intervention to improve physician reporting of adverse drug reactions: a cluster-randomized controlled trial. JAMA 296:1086–1093
Acknowledgments
The study was supported by institutional funds from the Emilia–Romagna region for the developing of pharmacovigilance. We are very grateful to the Drug Policy Service, Emilia–Romagna Region Health Authority, Bologna, Italy and to the pharmacists and GPs of the participating Local Health Authorities (Ferrara, Piacenza and Rimini) for their invaluable contribution to the research.
Competing interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Biagi, C., Montanaro, N., Buccellato, E. et al. Underreporting in pharmacovigilance: an intervention for Italian GPs (Emilia–Romagna region). Eur J Clin Pharmacol 69, 237–244 (2013). https://doi.org/10.1007/s00228-012-1321-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-012-1321-7