Abstract
Introduction
Patient reporting of adverse drug reactions (ADRs) to spontaneous reporting systems can make a valuable contribution to pharmacovigilance. However, the implementation and promotion of patient reporting systems (PRSs) differ worldwide.
Objective
The objective of the study was to describe attitudes toward PRSs, and progress toward implementing such systems among national competent authorities participating in the World Health Organization Programme for International Drug Monitoring.
Methods
A web-based questionnaire was constructed based on qualitative interviews, and distributed through SurveyMonkey® to all countries listed on the World Health Organization Programme for International Drug Monitoring (n = 178) during November and December of 2015. Data were analyzed using descriptive statistics and Chi-square tests.
Results
A total of 143 valid questionnaires were received from 141 countries (79.2 %). A spontaneous reporting system for both healthcare professionals and patients was present in 58 countries (41.1 %). An official PRS to report ADRs directly was implemented in 44 countries (31.2 %) and in a pilot stage in five countries (3.5 %). Patients were not allowed to report in 34 countries (24.1 %). The reasons for not having an official PRS were mainly a lack of resources/budget (56.5 %) or a lack of information/education for patients (56.5 %). When analyzing the attitudes among the respondents toward a PRS, most acknowledge that the general public contributes to the detection or strength of drug safety signals (82.2 % agree or strongly agree) and with information that is not present in healthcare professional reports (80.7 % agree or strongly agree). For respondents, giving feedback to patients could be an incentive for patients to report more (80.8 % agree or strongly agree). To be able to further PRSs, guidelines on promoting a PRS efficiently to the general public (87.4 % agree or strongly agree), training courses/conferences (86.7 % agree or strongly agree), or a public list of Lareb’s scientific publications (86.7 % agree or strongly agree) were the support measures most well accepted by the respondents.
Conclusions
Most countries accept ADR reports from patients by an official reporting system designed for patients or through the existing system for healthcare professionals. The main reasons for not having a PRS is financial restraints and a lack of information/education of patients. Attitudes toward a PRS are positive, but some countries fear that they will not be able to handle an increase in reports.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Most countries accept adverse drug reaction reports from the general public. |
The lack of resources/budget and the lack of information/education for patients are highlighted as the major obstacles to the implementation of patient reporting systems. |
Guidelines on implementing, promoting, and developing patient reporting systems as well as training are seen as useful tools to improve pharmacovigilance systems worldwide. |
1 Introduction
Patients are important contributors to pharmacovigilance through active reporting of adverse drug reactions (ADRs). Initially, patient reporting was described as a means to decrease under-reporting rates as a result of substantial under-reporting by healthcare professionals (HCPs). Targeting patients as reporters might help to increase reporting rates, which in turn might speed up the detection of ADRs. Moreover, since then, studies have shown that the contribution of patient reporting to pharmacovigilance goes beyond a quantitative contribution. Patient reports have brought a new dimension to pharmacovigilance [1, 2]. Patient reports of ADRs provide a valuable contribution to the detection of signals in addition to HCP reports and may give a new perspective on ADRs by directly reporting on their experiences without the HCP filtering out which ADR and information are relevant enough to report. Views on what information is important to report may vary between patients as with HCPs [1, 3]. They can also widen our knowledge on ADRs by providing information about the impact on daily life and circumstances of use, contributing to increased knowledge of the nature of ADRs in daily practice.
Beginning in the 1960s, countries such as USA, Canada, Australia, and New Zealand began accepting ADR reports from all reporters, including patients [4]. More recently, an increasing number of countries encourage the general public to report ADRs directly [5–8]. In Europe, allowing patients to report ADRs directly to the national competent authorities was seen by the European Commission as a way to improve pharmacovigilance and strengthen spontaneous reporting systems [9, 10].
In recent years, more and more national competent authorities worldwide have implemented systems to receive ADR reports from patients. However, a general awareness that patients can report ADRs remains low in most countries [8, 11–15]. This may be owing to the fact that patient reporting is not actively promoted across countries as a result of insufficient resources to support publicity campaigns and/or inadequate infrastructure to handle an increased reporting volume. In some countries, media attention about certain ADRs has increased awareness and reporting from the general public in a positive way [8, 16].
1.1 World Health Organization Collaborating Centre
On an international level, the World Health Organization (WHO) Programme for International Drug Monitoring promotes pharmacovigilance through the facilitation of the exchange of information, policies, guidelines, and other normative activities between countries and support countries in their pharmacovigilance activities [17]. As of February 2016, the WHO Programme for International Drug Monitoring had 123 full members and 28 associate members.
For providing support in the field of pharmacovigilance, the WHO appointed four Collaborating Centers (CCs) to help with these tasks. The Netherlands Pharmacovigilance Centre Lareb was appointed as a WHO CC for Pharmacovigilance in Education and Patient Reporting in 2013. One of the focal areas for Lareb as a WHO CC is to improve the processes and the scientific evaluation of patient reports and provide support to other members of the WHO Programme for International Drug Monitoring in setting up, running, and analyzing data from patient reports.
The purpose of this study was to describe attitudes toward patient reporting systems (PRSs), and progress toward implementing such systems among national competent authorities participating in the WHO Programme for International Drug Monitoring.
2 Methods
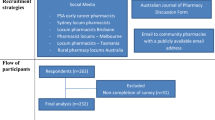
Data from qualitative interviews were used to develop a questionnaire that was sent to national pharmacovigilance centers worldwide to describe the level of development of their PRSs, investigate countries’ attitudes toward patient reporting, and to understand what type of support countries need to develop their PRSs further.
2.1 Interviews
Nine qualitative interviews were conducted. Interviews were conducted with persons from various geographical regions and with persons representing organizations who were in different stages of their implementation of patient reporting so as to get a broad view on how PRSs were implemented in the various countries and how Lareb could support them. The sample was drawn from the participants of the first Lareb Conference on Patient Reporting in 2015 [18] and the International Meyler Course in Pharmacovigilance [19] that was held before the conference in April 2015. The meeting attracted 60 participants from 21 countries discussing a range of subjects relating to patient reporting. From this group, colleagues were selected for an interview. Interviews were conducted with pharmacovigilance representatives from Japan, New Zealand, Vietnam, France, Switzerland, Ireland, Norway, Ghana, and Georgia.
A structured interview guide was constructed for the face-to-face interview (see Electronic Supplementary Material 1). The main topics of the interview were the stage of implementation of patient reporting in the countries, practical experiences, thoughts on the contribution of patient reporting to pharmacovigilance, and views on what type of support and services Lareb could provide as a WHO CC. All interviews were recorded, transcribed verbatim, and analyzed by content analysis.
2.2 Questionnaire
The questionnaire addressed a number of questions that intended to characterize the existing PRSs worldwide, regarding the level of maturity of PRSs, with maturity meaning to what extent the potential of patient-reported safety information and its role in contributing to public health protection has been implemented, the type of information collected, and how patient reports are used. For countries without a PRS, motives for not implementing it were surveyed. Whenever possible, questions were asked in a multiple-choice manner or with check-boxes options to facilitate responding to the questionnaire.
A list of quotes from the qualitative interviews was compiled in two major themes and presented as statements. The first theme contained a list of services that Lareb could provide as WHO CC for patient reporting. Next to the response options on the possible services was an ‘Other’ option along with a free text area for ‘please specify’. The second theme included statements on the general opinions on patient reporting and an open-field text to give opinions not listed.
The statement items could be rated on a five-point Likert scale (strongly agree to strongly disagree) where the middle position was labeled ‘neutral’ to reflect a neutral position, and not an inability to answer the question. A “Not relevant” option was also added to all the statements. The questionnaire (see Electronic Supplementary Material 2) was created and distributed using SurveyMonkey® (Palo Alto, CA, USA).
2.3 Study Population
The target population comprised the national pharmacovigilance centers participating in the WHO Programme for International Drug Monitoring. A contact list was provided by the Uppsala Monitoring Centre. The contact list was analyzed and for each country, the National Head Center (NHC) and the Focal Person (FP) and Technical Person (TP) were identified to be surveyed. When the NHC, FP, or TP were not available, other contacts were selected. A total of 178 countries were identified, including 123 full member countries, 28 associate members, and 27 other countries that are not members of the WHO Programme. All 178 countries were invited to take part in the survey. The response rate was calculated based on the number of the countries included, so only one answer was required from each country.
2.4 Sending the Questionnaire
The web-based survey was first tested in a small group of field testers (n = 10, colleagues from Lareb and the Uppsala Monitoring Centre) and subsequently sent to the selected respondents on November 9, 2015 with SurveyMonkey®. Two and four weeks later (on November 23, 2015 and December 7, 2015), a reminder was sent to all non-respondent countries and those who had provided incomplete answers. After that, two personal reminders were sent to non-respondent countries to obtain more answers. The collection of responses ended on December 21, 2015. The link in the invitation e-mail was uniquely tied to the survey and the respondent’s e-mail address. Therefore, the message could not be forwarded by respondents, and only one response per e-mail address was allowed. This also implied that random surfers on the Internet could not reach the online survey [20].
2.5 Data Analysis
For data analysis, if multiple answers from the same national center per country were obtained, these were compared and merged, if possible. The answer of the head of the organization was preferably selected if answers between respondents from the same organization varied. However, for the examples on signal detection, all quotes were taken into account. When questionnaires from the highest ranking person in the organization were incomplete, but another colleague from the same center filled in the remaining questions, these answers were used to get a complete response for that country. If two or more answers were received from the same institution and none were from the Head of the institution, the answer from the TP or FP were selected for analysis.When only an incomplete answer was received, the answers to the questions that were completed were included in the analysis.
Descriptive statistics provided an overview of the countries needs and opinions about patient reporting. A Pearson Chi-square (χ 2) test was performed to detect significant differences between countries that accept patient reports and those who do not. The χ 2 test for trend was also calculated (depicted as the linear-by-linear association in the SPSS® output). Significance was based on a two-sided χ 2-test and significance was set at p < 0.05.
Because the data were measured at the ordinal level (Likert scale), Spearman’s correlation coefficient (r) was used in this analysis. In this study, a correlation was considered strong if r > 0.7, moderate if r > 0.4 and <0.7, and weak if r < 0.4 [21] Data were analyzed using the statistical SPSS® Statistics Version 22 software (IBM Corporation, Armonk, NY, USA).
3 Results
3.1 Response Rate
One hundred and seventy-eight countries were invited to take part in the survey. The questionnaire was sent to 942 individual respondents via email. That means that one center could receive multiple questionnaires. Three hundred and twenty persons on the contact list were deemed to be the ‘most important’ contacts. These were the heads of the organizations (152) and the FPs and TPs. Other persons on the list were contacts for the WHO Drug Monitoring Programme without a specific function. The response rate for NHCs (64 of 152) or NHCs and FPs, TPs grouped together (130 of 320) was significantly higher than for the ‘other’ contacts (64 of 622) on the list (two-sided Pearson χ 2; p < 0.01). In total, 194 answers from 141 countries were collected (see Electronic Supplementary Material 3). Multiple answers from the same organization were compared, the response from the NHC was preferably selected. Incomplete questionnaires per country were merged to obtain a complete set of answers per country. In two countries with answers from more than one institution responsible for collecting ADRs (n = 2), both answers were selected for analysis. Answers from a total of 141 countries representing 143 organizations were selected for analysis, of which 137 were complete and 6 incomplete.
The response rate was calculated based on the number of countries that answered the questionnaire. The final response rate was 79.2 % (n = 141). According to the United Nations (UN), there are 193 recognized countries, [22] in which 170 were surveyed. The questionnaire was also sent to eight territories that are not recognized by the UN. We obtained 137 countries answers (71.0 %) from UN recognized countries and 4 answers from other territories. The relative responses rates were calculated based on the WHO Programme for International Drug Monitoring membership status. The results are presented in Table 1.
3.1.1 Implementation of Patient Reporting Systems and Practical Experiences
Results show that an ‘official reporting system’ for patients had been implemented in 31.2 % (n = 44) of the countries who responded to the survey. A trial/pilot PRS is under implementation in five countries. These reporting schemes work with dedicated reporting forms for patients.
In addition, reporting systems used by both HCPs and patients, without a special system designed for patients, were present in 41.1 % (n = 58) of the responding countries. Patients were not allowed to report in 34 countries (24.1 %). The lack of an official PRS was mainly owing to a lack of resources/budget (56.5 %, n = 52) and a lack of information/education for patients (56.5 %, n = 52). A minority of countries considered it a political decision not to implement PRS (10.9 %) or because they “don’t feel that patient reports are helpful for pharmacovigilance” (4.3 %). Other reasons stated include those patients could report within the existing spontaneous reporting systems (7.6 %) and patient reports need medical confirmation of ADRs reported (4.3 %) (Tables 2, 3).
According to the answers to the questionnaires, official PRSs started first in USA (1969), Republic of Korea (1988), Australia (1990), the Netherlands (2003), Morocco (2003), Denmark (2003), and Zanzibar (2003). However, some countries stated that they received reports from patients since the creation of their systems, and other countries stated they did not adapt their systems to have an official system for patients to report, but received reports from patients anyway. For the 49 countries that had an official PRS or a PRS in the trial stage, only 30.6 % (n = 15) stated that they had it for more than 5 years.
The countries receiving the highest percentage of patient reports in 2014 are USA (n = 823,813, 63.9 %), Canada (approximately 19,500, 30 %), Denmark (n = 1820, 28 %), the Netherlands (n = 4393, 20.2 %), and Morocco (n = 556, 19.5 %). A total of 75 countries have fewer than 50 reports from patients or do not have information about the number of patient reports collected. Although some reporting systems collect data worldwide, the values of reports submitted by the countries could come from other countries, and not only by domestic reports.
E-mail and telephone are the most used methods for patients to report, both in 63.9 % (n = 69) of the countries. Other frequently used methods include paper reporting forms, specially designed for patients (n = 33, 30.6 %) or a paper form designed for both HCPs and patients (n = 58, 53.7 %). The means of reporting used to collect reports from patients are summarized in Table 4.
PRSs mainly collect ADRs on prescribed medicines (n = 100, 92.6 %), over-the-counter medication (n = 87, 80.6 %), vaccines (n = 80, 74.1 %), and medication errors (n = 73, 67.6 %). Some countries also collect ADRs on herbal treatments (n = 67, 62 %), ADRs related to the off-label use of medicines (n = 67, 62 %), counterfeit products (n = 57, 52.8), and vitamins and food supplements (n = 52, 48.1 %). Information about harm related to the use of cosmetics (n = 5, 4.6 %), medical devices (n = 2, 1.9 %), chemical products (n = 2, 1.9 %), and unregistered products (n = 1, 0.9 %) are also being collected.
Patient reports are used in signal detection (n = 69, 64.5 %), and are used to gain insight and knowledge about the impact of the ADR on daily life (n = 56, 52.3). However, some countries also collect reports but do not use them actively (n = 30, 28 %). Countries were asked in an open question if they had any examples on how patient reports were useful in their country in identifying drug safety issues (for example, a signal on an ADR, identifying counterfeit drugs or quality issues, additional information on the impact on quality of life). There were 73 answers to this question. Some striking quotes are given below:
“In 2009 we received many cases from patients regarding Eltroxin®. It showed up that the MAH had made some changes to the excipients that influenced the bioavailability and therefore caused signs of either increased or decreased hormone levels in the blood. Recently, we received many patient reports regarding HPV vaccine.” (Denmark) This signal was published by the Danish Medicines Agency in 2010 [23]. A similar quote on this topic, “Eltroxin®—Change of thyroid medication manufacturing plant.” (New Zealand), was published in 2009 [24]. |
“Report of the abuse of benzydamine hydrochloride leading to serious crisis; hallucinations and delusions that led to a suicide attempt. This has resulted in the cancellation of the drug registration for benzydamine hydrochloride for systemic use.” (Brazil) This signal was published in 2009 [25]. |
“Yes, a few years ago, about 4 patients in different health facilities had reactions to chloramphenicol injection, leading to the death of one. We had to withdraw the injection from all our health facilities, and we stopped procuring the same injection from the supplier. We were able to identify breaches of contract by the supplier, where the approved manufacturer outsourced production of some of our medicines to unapproved manufacturers within the same country” (Fiji) |
“Yes, the case of dextromethorphan in 2013, with 59 intoxicated patients, the signal was started with 4 reports.” (Paraguay) This signal was published in the Drug Alerts by the WHO in 2013 [26]. |
“There was a report regarding necrosis at the site of injection of diclofenac which is a rare ADR and after analyzing the case we found an error in the technique used.” (Iraq) The signal was published as an abstract in the ISOP Congress 2011 [27]. |
“Discovery of counterfeit Human albumin and discovery of medication errors with rabies vaccine.” (Egypt) |
“Red yeast rice causing muscle ache, similar ADR that patient experienced while on lovastatin treatment. Suspected the product was adulterated with lovastatin/statin. The product been tested and found a trace of lovastatin, but the amount is too low, which is, definitely, not due to the adulteration. The same test been done with the other red yeast rice containing product and found out all of the products contains a trace of lovastatin but in a small amount. With that result, all product containing red yeast rice must ensure that the amount of lovastatin in the product must be less than 1 % w/w, and all the product must carry a warning label that this product contains naturally occurring lovastatin.” (Malaysia) |
3.1.2 Opinions on Patient Reporting in General and World Health Organization Collaborating Centre Services that Could Support Countries
When analyzing the attitudes among the respondents toward PRS, most acknowledge that the general public contributes to the detection or strength of drug safety signals (82.2 % agree or strongly agree) and provides information that is not present in HCP reports (80.7 % agree or strongly agree). For respondents, giving feedback to patients could be an incentive for patients to report more (80.8 % agree or strongly agree). However, they also claim that promoting and handling patient reports will require extra resources (63.7 % agree or strongly agree), and are more labor intensive than HCP reports (60.7 % agree or strongly agree).
To investigate if there are differences in opinions about patient reporting between countries who accept patient reports and countries that currently do not accept patient reports, the χ 2 test was performed on the statements in Table 5. The χ 2 test did not show any significant differences. The χ 2 test was repeated, and in this analysis, the “disagree” and “strongly disagree” categories were merged to one variable and the “agree” and “strongly agree” categories. This analysis showed differences between those countries who accept and do not accept patient reports, “Having an implemented patient reporting system requires more additional resources than a system for healthcare professionals” (χ 2; p = 0.04) and “Patient reports are more difficult to code than healthcare professional reports” (χ 2; p = 0.03). Centers who accept patient reports agreed with this less often, which in the authors’ view shows that there are some false beliefs about PRSs, which are dispelled as the systems are being implemented. However, there was no trend for this statement based on the type of system implemented (T value >0.05).
In an open question, countries were asked on their general opinion on the value of direct patient reporting to pharmacovigilance. A total of 97 answers were obtained and analyzed. Most of them show positive views and advantages on patient reporting (n = 85); however, there are some responses that show some drawbacks of patient reporting (n = 19), such as the lack of knowledge of patients, the lack of resources of the competent authority to deal with patient reports, the lack of accuracy of the reports that requires them to be medically confirmed, and the difficulty in implementing a PRS.
Some quotes on the importance of patient reporting in pharmacovigilance are given below:
“It should be our priority that the patients would be the first line of data capture. Patient reporting is very important because the patients can provide real information in real time, and they know the ADRs better than anybody.” (Mexico) |
“The patient always has a real concern about an ADR, so his/her report is very important to develop signals and to improve knowledge about safety but drug use, also the patient always is going to report anything wrong with the medication, so we could have reports not only about ADR but medication errors, quality problems, among others. Is very useful and important the direct patient report in a country.” (Cuba) |
“Direct patient reporting is very important in monitoring the safety of drug products being made available in the market including those purchased online.” (Philippines) |
“It is important to hear the patient’s voice being the one who actually experienced the reaction.” (Kuwait) |
“Patient reporting ADRs has an added value in pharmacovigilance in the way that allowing patients to report gives us an idea about the burden of ADRs to patients and how this impact their daily life/activities. Also, patients report more details about ADRs than HCPs and sometime about concomitant medication, medical history, lifestyle, etc., details useful for evaluation. We have little experience with patient reporting but in the future we expect more ADRs from patients, taking into account that NAMMD organized meetings with Patient Associations representatives on ADR reporting and pharmacovigilance.” (Romania) |
“Direct patient reporting is important especially since some patients fail to inform their healthcare provider when they experience adverse drug reactions (they just stop taking the medication), so the ADR is never documented.” (St. Vincent and the Grenadines) |
“Patient reporting provides the patient experience as an independent perspective from those of health professionals, and it is important because under-reporting by health professionals. A patient can potentially provide much more detail and clearer descriptions of their experiences than health professionals when reporting suspected ADRs. The combination of reports from healthcare professionals with first-hand information from the patients increases chances to identify new safety issues.” (Zimbabwe) |
“Reports from patients can provide information about the reality of the impact of the problem on the quality of life and also in adherence to drug treatments. In addition, there is a tendency for reports of patients are more free from conflicts of interest.” (Brazil) |
However, some respondents also mention the difficulties of working with direct patient reporting in their country:
“In our country, most of the people cannot write. Even if they can do it, I not sure that a patient can describe the ADR correctly. I think describing clinical signs is for a health professional.” (Senegal) |
“It is an important aspect of reporting, but it has been noticed that even through reporting to physicians the picture of what is being reported is confused and affected by many factors that the receiving physician could be unaware of such as psychiatric and family issues. What is being reported by patients is not scientifically reliable but for sure it could be filtered and revised by the receiving physician which is very cumbersome and add to the already existing workload.” (Bahrain) |
“We understand that useful safety information can be obtained through patient reporting. However, we are not promoting patient reporting extensively as we do not have enough human resource at our centre.” (Namibia) |
“Number of patient reports is arising every year (2014—213, 2015—392), patients are very motivated to report as ADRs are influenced their life. Their reports are not so accurate but often very detailed (more than these from HCPs), sometimes it is quite hard to recognize and code ADR properly. We appreciate all patient reports because they sometimes contain very important information which was not sent by HCPs (they do not consider it as relevant or related—but it is showed in some time that it is really related).” (Czech Republic) |
Table 6 shows the response to the question: “To support you in your daily work, what type of services could Lareb provide as WHO Collaborating Center for patient reporting?” To be able to further PRSs, guidelines on promoting a PRS efficiently to the general public (87.4 % agree or strongly agree), training courses/conferences (86.7 % agree or strongly agree), or a public list of Lareb’s scientific publications (86.7 % agree or strongly agree) are the support measures most well accepted by the respondents.
Countries were also asked in an open-ended question for other ideas; for instance, developing tools such as mobile apps for patient reporting that can be customized by countries, a summit for interactions between agencies that have already implemented and succeeded and those in the process, assistance on how to assess the impact of the number of reports in a low-resource team, and networking of ideas. In addition, ideas for support in strengthening pharmacovigilance, in general, were given.
4 Discussion
Direct patient reporting is accepted in a growing number of countries. This questionnaire, based on qualitative interviews, and sent to an extensive list of countries worldwide provides important insights into the status of patient reporting. With this questionnaire, we have gained new information on how patient reporting is used in pharmacovigilance and what type of information/signals patient reporting contribute to. This is useful information, not only for the pharmacovigilance community but also to show patients themselves how their reports can make a difference. It is also important to receive first-hand information about the difficulties in some countries, for instance, owing to illiteracy in the community.
Viewing the answers in this questionnaire, there is room for improvement of PRSs. As a WHO Collaborating Centre, the Netherlands Pharmacovigilance Centre Lareb wants to serve as a platform for knowledge transfer by providing training, conducting research, and developing best practice for staff active in pharmacovigilance, both at national centers as well as in academia. These activities will hopefully help to develop pharmacovigilance further and increase the awareness of ADRs and the reporting thereof. Because it is important to hear from colleagues themselves worldwide as to what their experiences with patient reporting are and what support would be appreciated, this questionnaire was conducted. Conferences/training courses and guidelines on promoting a PRS efficiently to the general public were seen as the most useful support activities that could be organized or developed.
4.1 Strengths and Limitations of the Study
4.1.1 Participation in the Study
The major strength of this study is the high response rate of 79.2 % in comparison with other similar studies [6, 28]. The survey covers countries from all continents. The target population was the national pharmacovigilance centers participating in the WHO Programme for International Drug Monitoring. However, we also included associate members of the programme and some non-members that were on the contact list from the Uppsala Monitoring Centre. The rationale for doing so is that the member status is likely related to the maturity of the pharmacovigilance system in that country. The main asset of the WHO Drug Monitoring Programme is its database of ADR case reports submitted by the participating countries. A country will be regarded as an associate member country from the time the formal membership application is received. In a procedure, the associated member will have to provide evidence that they can submit quality information to the WHO database [29]. Non-members on the contact list likely do not have the technical opportunities (yet) to join the WHO Drug Monitoring Programme. However, including them could provide some valuable answers from developing countries that we did not want to miss. Hence, they were included.
The support and services that may arise through this study can help countries to implement pharmacovigilance practices that allow patients to have an active involvement in pharmacovigilance. Despite the high response rate, a limitation of the study is that we did not receive answers from Russia and China, whose populations represent approximately 20.77 % of the world’s total population.
4.1.2 Respondent Characteristics
The questionnaire was based on qualitative interviews. It was a convenience sample drawn from the participants of a conference on patient reporting in pharmacovigilance, taking into account geographic spread and maturity of their pharmacovigilance system. Because the sample for the interview was small, there was a possibility to add free text in the questionnaire if respondents had suggestions or ideas that did not come forth in the interviews and therefore were not included in the questionnaire.
Another potential limitation was related to the role of the respondents in the pharmacovigilance centers. In each center, if possible, the national head of the organization was surveyed; however, his/her view could be potentially different from the views of other staff. It was not possible to reach all the national heads of the organizations for confirmation of the results in the case of another colleague filling in the questionnaire.
Social interaction between the interviewer and respondent can also lead to respondents taking social norms into account when responding, resulting in social desirability bias. Respondents often give the ‘most correct’ answer rather than the real or valid answer to the surveyed questions. Personal contacts made between the authors and the respondents may have caused social desirability bias.
4.1.3 Construction of the Questionnaire
The questionnaire was developed based on information from qualitative interviews, which could be viewed as another strength of the study. The statements in the questionnaire were based on qualitative interviews aiming to increase the validity of the survey—respondents’ words and phrases were used for writing the closed-ended statements. As a result, the relevance and comprehension of the quantitative survey are enhanced, thereby improving the validity of study findings [30]. Furthermore, to avoid invalid data, an odd-numbered scale for rating the statements is chosen. When respondents were truly neutral on a topic, they were not forced to any side [31].
The final questionnaire version, based on interviews, was pre-tested to understand major drawbacks and improvements to the questionnaire. During pre-testing, respondents mentioned that a few statements were confusing, these were rewritten to provide a more easy understanding of the questionnaire. Despite this, in the data analysis, the authors could observe that the wording of the questionnaire was not 100 % optimal, as certain participants were confused by the answer options. For example, the distinction between a system that can be used by patients only vs. one that can be used by both HCPs and patients was not clear. Our idea was that if a country has a ‘PRS’ next to their HCP reporting system it did not only mean that patients can report, but that the system is tailor made for patients including designated reporting forms, patient reporting activities aimed at patients, and information provided by the pharmacovigilance center in layperson’s language. However, from the responses to the questionnaire we saw that this wording was confusing to some respondents. This is a limitation of the study.
4.2 Further Developments in Patient Reporting in Pharmacovigilance
With this questionnaire, we have tried to shed more light on the level of development of PRSs worldwide and the attitudes toward patient reporting. A secondary objective was to understand what type of support countries need to develop their PRSs further. In 2015, the first Lareb Conference on Patient Reporting was organized in the Netherlands. The meeting attracted 60 participants from 21 countries discussing a range of subjects relating to patient reporting. From the interviews with participants, but also from the questionnaire, such conferences and training courses specifically on patient reporting seem to fulfill a need.
Two years ago, the Monitoring Medicines Project aimed to strengthening patient reporting in pharmacovigilance, among other goals. This project led to the development of a guideline on starting a PRS and multiple publications [8, 32–34]. Commissioned by the Monitoring Medicines Project, the Uppsala Monitoring Centre led the design and development of a web-based ADR reporting tool intended for use by patients [33].
In September 2014, a 3-year project called WEB-RADR was launched. WEB-RADR’s mission is to develop new ways of using technologies and channels of communication for pharmacovigilance purposes. WEB-RADR is currently working in two key outcomes, including a mobile phone app for the reporting of suspected ADRs to European Union regulators, providing a platform for direct and instant ADR reporting for patients and HCPs, and a means for regulators to communicate back to these stakeholders the latest pharmacovigilance information. New technical tools for data mining publicly available data shared on social media websites are also under development, which will enable more reliable mining of social media data, allowing national competent authorities to detect, extract, and analyze potential ADRs reported in unstructured free text by social media users [35, 36].
There has also been local promotion of direct patient ADR reporting, such as pharmacy-assisted patient reporting pilots in Italy [37, 38]. These pilots concluded that pharmacists can have an important role in promoting patient reporting and that the differences between reports by patients and HCPs indicate different points of view that can enrich spontaneous reporting.
Although the topic of patient reporting in pharmacovigilance has gained more attention in the last few years, the full potential of patient-reported safety information and its role in contributing to public health protection is yet to be realized [39]. In the early years of patient reporting, much focus was on treating patient reports in the same way that we treat HCP reports, to show that patient reports are of equal value. Our experience is that patient reports provide valuable information that HCP reports do not capture and it is important to optimize the methods for collecting, coding, and recording patient-reported information and the methodologies applied for signal detection to make the most of the information from patients, as most systems and methodologies have been designed with the information provided from HCPs in mind [39]. With patients being more and more important stakeholders in pharmacovigilance, it is also important to think about how pharmacovigilance can share the knowledge it has with this group in an open and transparent way.
5 Conclusion
About three-quarters of the countries (71 %) responding to this worldwide questionnaire allowed the general public to report ADRs directly. Favorable outcomes of patient reporting are described, such as the signal value of the reports or description of the severity of the ADRs. However, implementing and maintaining a PRS is not without its challenges as almost 64 % of respondents agreed with the statement “Having an implemented patient reporting system requires more additional resources than a system for healthcare professionals”. Lack of resources, staff, and the education level of the population are drawbacks for some countries to implement or to optimize PRS. The general opinions on patient reporting show that many centers agree that these reports can add value to pharmacovigilance. The questionnaire responses also provided new insights into how Lareb, as a WHO CC, can support countries seeking to implement PRSs moving forward and support other colleagues working with patient reports.
References
Härmark L, van Hunsel F, Grundmark B. ADR reporting by the general public: lessons learnt from the Dutch and Swedish systems. Drug Saf. 2015;38(4):337–47.
Blenkinsopp A, Wilkie P, Wang M, Routledge PA. Patient reporting of suspected adverse drug reactions: a review of published literature and international experience. Br J Clin Pharmacol. 2007;63(2):148–56.
van Hunsel F, Talsma A, van Puijenbroek E, et al. The proportion of patient reports of suspected ADRs to signal detection in the Netherlands: case-control study. Pharmacoepidemiol Drug Saf. 2011;20(3):286–91.
Ahmad SR. Comment on:“adverse drug reaction reporting by patients: an overview of fifty countries”. Drug Saf. 2015;38(1):109–10.
Margraff F, Bertram D. Authors’ reply to Ahmad SR:“adverse drug reaction reporting by patients: an overview of fifty countries”. Drug Saf. 2015;38(1):111.
Margraff F, Bertram D. Adverse drug reaction reporting by patients: an overview of fifty countries. Drug Saf. 2014;37(6):409–19.
Herxheimer A, Crombag M, Alves TL. Direct patient reporting of adverse drug reactions: a fifteen-country survey and literature review. Amsterdam: Health Action International (HAI) Europe; 2010 (Paper Series Reference 01–2010/05). http://haieurope.org/wp-content/uploads/2010/12/10-May-2010-Report-Direct-patient-reporting-of-adversedrug-reactions.pdf.
van Hunsel F, Härmark L, Pal S, et al. Experiences with adverse drug reaction reporting by patients. Drug Saf. 2012;35(1):45–60.
EC. Directive 2010/84/EU of the European Parliament and of the Council of 15 December 2010 amending, as regards pharmacovigilance. Directive 2001/83/EC on the Community code relating to medicinal products for human us [online]. http://ec.europa.eu/health/files/eudralex/vol-1/dir_2010_84/dir_2010_84_en.pdf. Accessed 30 May 2016.
Borg J-J, Aislaitner G, Pirozynski M, Mifsud S. Strengthening and rationalizing pharmacovigilance in the EU: where is Europe heading to? Drug Saf. 2011;34(3):187–97.
Matos C, van Hunsel F, Joaquim J. Are consumers ready to take part in the pharmacovigilance system? A Portuguese preliminary study concerning ADR reporting. Eur J Clin Pharmacol. 2015;71(7):883–90.
McLernon DJ, Bond CM, Lee AJ, et al. Patient views and experiences of making adverse drug reaction reports to the Yellow Card Scheme in the UK. Pharmacoepidemiol Drug Saf. 2011;20(5):523–31.
Robertson J, Newby DA, Robertson J. Low awareness of adverse drug reaction reporting systems: a consumer survey. Med J Aust. 2013;199(10):684–6.
Jha N, Rathore DS, Shankar PR, et al. Need for involving consumers in Nepal’s pharmacovigilance system. Australas Med J. 2014;7(4):191–5.
Fortnum H, Lee AJ, Rupnik B, Avery A. Survey to assess public awareness of patient reporting of adverse drug reactions in Great Britain. J Clin Pharm Ther. 2012;37(2):161–5.
van Hunsel F, van Puijenbroek E, de Jong-van den Berg L, van Grootheest K. Media attention and the influence on the reporting odds ratio in disproportionality analysis: an example of patient reporting of statins. Pharmacoepidemiol Drug Saf. 2010;19(1):26–32.
Olsson S. The role of the WHO programme on international drug monitoring in coordinating worldwide drug safety efforts. Drug Saf. 1998;19(1):1–10.
Lareb. Conference on patient reporting. 2015. http://www.lareb.nl/whocc/Conference-on-Patient-Reporting. Accessed 13 Jul 2016.
Lareb. Netherlands Pharmacovigilance Centre Lareb training courses. 2015. http://www.lareb.nl/whocc/Training-courses?lang=en-GB. Accessed 24 Jul 2016.
SurveyMonkey. Sending surveys via email invitation. 2016. http://help.surveymonkey.com/articles/en_US/kb/Email-Invitation-Collector. Accessed 14 Jul 2016.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrance Eribaum Association; 1988.
United Nations. United Nations Member States. http://www.un.org/en/member-states/. Accessed 27 Jul 2016.
Danish Medicines Agency. The Danish Medicines Agency’s annual pharmacovigilance report 2009. Annual Report. 2010.
Faasse K, Cundy T, Petrie KJ. Thyroxine: anatomy of a health scare. BMJ. 2009;339:b5613.
Opaleye ES, Noto AR, Zv Sanchez, et al. Recreational use of benzydamine as a hallucinogen among street youth in Brazil. Rev Bras Psiquiatr. 2009;31(3):208–13.
World Health Organization. Drug Alert 129: Contaminated Dextromethorphan active pharmaceutical ingredient. 2013. http://www.who.int/medicines/publications/drugalerts/App_Drug_Alert_No_129_Paraguay_Dextro.pdf. Accessed 25 April 2016.
ISOP. 11th ISoP annual meeting “Next Stop: Istanbul—Bridging the Continents”, Istanbul, Turkey, 26–28 October, 2011. Drug Saf. 2011;34(10):883–1026.
Olsson MS, Pal SN, Stergachis A, Couper M. Pharmacovigilance activities in 55 low-and middle-income countries. Drug Saf. 2010;33(8):689–703.
Uppsalla Monitoring Center. Joining the WHO Programme for International Drug Monitoring. 2010. http://www.who.int/medicines/areas/quality_safety/safety_efficacy/Joining_the_WHO_Programme.pdf?ua=1. Accessed 24 Jul 2016.
Krause N. A comprehensive strategy for developing closed-ended survey items for use in studies of older adults. J Gerontol Ser B Psychol Sci Soc Sci. 2002;57(5):S263–74.
Sue VM, Ritter LA. Conducting online surveys. Thousand Oaks, CA: Sage Publications; 2007.
Pal SN, Olsson S, Brown EG. The Monitoring Medicines Project: a multinational pharmacovigilance and public health project. Drug Saf. 2015;38(4):319–28.
Plöen M, Wallberg M, Olsson S. User-driven development of a web-based tool for patient reporting of drug-related harm. Drug Saf. 2015;38(4):359–64.
World Health Organization. Safety monitoring of medicinal products: reporting system for the general public. Geneva: WHO; 2012.
Ghosh R, Lewis D. Aims and approaches of Web-RADR: a consortium ensuring reliable ADR reporting via mobile devices and new insights from social media. Expert Opin Drug Saf. 2015;14(12):1845–53.
Web-RADR project. https://web-radr.eu/. Accessed 30 May 2016.
Leone R, Moretti U, D’Incau P, et al. Effect of pharmacist involvement on patient reporting of adverse drug reactions: first Italian study. Drug Saf. 2013;36(4):267–76.
Parretta E, Rafaniello C, Magro L, et al. Improvement of patient adverse drug reaction reporting through a community pharmacist-based intervention in the Campania region of Italy. Expert Opin Drug Saf. 2014;13(Suppl. 1):21–9.
Härmark L, Raine J, Leufkens H, et al. Patient-reported safety information: a renaissance of pharmacovigilance? Drug Saf. 2016. doi:10.1007/s40264-016-0441-x.
Acknowledgments
The authors thank Anna Hegerius, PharmD at the Uppsala Monitoring Centre, WHO Collaborating Centre for International Drug Monitoring, Sweden for her feedback on the questionnaire.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were used to assist in the preparation of this article.
Conflicts of interest
Cristiano Matos, Linda Härmark, and Florence van Hunsel have no conflicts of interest that are directly relevant to the content of this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Matos, C., Härmark, L. & van Hunsel, F. Patient Reporting of Adverse Drug Reactions: An International Survey of National Competent Authorities’ Views and Needs. Drug Saf 39, 1105–1116 (2016). https://doi.org/10.1007/s40264-016-0453-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-016-0453-6