Abstract
Background
In the UK, clinicians usually make treatment decisions based on total cholesterol (TC) at the same time supplemented with high-density lipoprotein cholesterol (HDL-C) measurements. We evaluated statin-associated TC concentration change and its impact on cardiovascular (CV) risk reduction in diabetic patients in the setting of usual care.
Methods
In a population-based cohort study using a record-linkage database in Tayside, Scotland. we studied 6,697 diabetic patients who had at least two separate TC measurements between 1993 and 2007. Patients were categorized into statin-exposed and statin-unexposed groups according to statin use status during the follow-up. The main outcomes were TC concentration change from baseline, CV events, and all-cause mortality during the follow-up. Multivariate Cox regression models with a time-dependent variable for statins were employed to assess outcome risk.
Results
Statin-associated TC concentrations decreased by 1.64 mmol/L (28%) in patients without CV disease (CVD) (5,984) and 1.19 mmol/L (23%) in patients with CVD (713) from 5.90 mmol/L and 5.20 mmol/L at baselines, respectively. Statin use reduced incident and recurrent CV events by 39% and 41%, respectively [adjusted hazard ratio (HR) 0.61, 95% confidence interval (CI) 0.57–0.66; 0.59 95% CI 0.47–0.76) per millimole of TC reduction. For all-cause mortality, the adjusted HRs were 0.39 (95% CI 0.32–0.47) in primary prevention and 0.58 (95% CI 0.42–0.80) in secondary prevention.
Conclusion
Statin use was as effective in diabetic patients in the setting of usual care, as in the clinical trials, in both primary and secondary prevention. TC changes can be used as a measure of statin efficacy in the absence of low-density lipoprotein cholesterol (LDL-C) in diabetic patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
At least 2.8% of the world’s population (171 million) suffered from diabetes mellitus (DM) in 2000, and this number is estimated to be almost double by 2030 [1]. It is well established that diabetes is a major risk factor for cardiovascular disease (CVD), and people with diabetes are much more likely to have cardiovascular (CV) events compared with the general population [2, 3]. CVD is the main cause of death in diabetic patients, accounting for some 50% of all diabetic mortality, as well as causing significant morbidity [4]. Diabetic dyslipidemia, which is typically a low high-density lipoprotein cholesterol (HDL-C), increased triglycerides, and postprandial lipemia, is an important risk factor for subsequent CVD [5–7]. It is most frequently seen in type 2 diabetes, and even small increases in low-density lipoprotein cholesterol (LDL-C) are associated with substantial increases in CV risk [7]. Meta-analyses of clinical trials suggest that statin-related reduction of LDL-C concentration predicted proportional reductions in incident or recurrent CV events and all-cause mortality in diabetic patients [8, 9]. However, evidence is lacking on how total cholesterol (TC) decrease with statins predicts risk reduction of CV events and mortality in such patients in the usual care setting.
In the UK, clinicians usually make treatment decisions based on TC with or without HDL-C measurements. In statin trials, we show that TC reductions with lipid-lowering drugs is almost as good as LDL-C in predicting outcome [10] and that TC can be used as a reasonable measure of statin efficacy in the absence of LDL-C [11]. In the study presented here, we assessed the effectiveness of statins on TC concentrations and CV events and all-cause mortality in diabetic patients.
Methods
We performed a cohort study in Tayside, Scotland, using the Medicines Monitoring (MEMO) Unit record-linked database. The data collection methods have previously been described [12]. In brief, MEMO contains several data sets including all dispensed community prescriptions, hospital discharge data, biochemistry data, and other data. These are linked by a unique patient identifier, the Community Health Index (CHI) number. These data are anonymized for the purposes of research, as approved by the Caldicott Guardians. This project was also approved by the Tayside Committee on Research Medical Ethics.
Study population
The study population consisted of residents of Tayside who were registered with a general practitioner between January 1993 and December 2007 and remained residents in Tayside or died during the study period.
Patients
Study patients were those with a primary diagnosis of diabetes between January 1993 and December 2007 identified from Diabetes Audit and Research in Tayside Scotland (DARTS) [13]. The date of their first diagnosis of diabetes was used as the study entry date. They were divided into statin-exposed and statin-unexposed groups according to whether or not they were taking statin treatment during the follow-up. These patients also had to have at least two TC measurements and at least 30 days apart during the follow-up. The statin-exposed group included prevalent statin-exposed patients (statin use within 180 days prior to entry date) or incident statin-exposed patients (statin use after the entry date). Patients with no statin treatment during this period constituted the statin-unexposed group. Patients who were prescribed other lipid-lowering drugs after the entry date or within 180 days prior to the entry date were excluded (n = 468). Patients were also classified into primary (PP) and secondary (SP) prevention cohorts in the analysis according to whether they had established CV disease [stroke, transient ischemic attack (TIA), myocardial infarction (MI), angina, heart failure (HF)] prior to the entry date.
Total cholesterol measurements
Serum TC measurements were obtained from the regional biochemistry database. Baseline TC concentration was that measured on the nearest date to the entry date. This date was in the range of within 1 year before or within 30 days after the entry date. Follow-up TC concentration met the following criteria: (1) on or within 180 days prior to the CV admission; (2) the last available TC measurement during follow-up in patients without the CV admission; (3) at least 30 days after statin treatment in the statin-exposed group.
Outcome variables
The primary study outcome was TC concentration change from baseline, and secondary outcomes were incident or recurrent Antiplatelet Trialist’s Collaboration (APTC) events and all-cause mortality during the follow-up. We used the APTC endpoint of nonfatal MI [International Classification of Disease (ICD9), ninth revision: 410; and tenth revision (ICD10): I21] [14], nonfatal stroke (ICD9: 431, 434.9, 436; ICD10: I61, I63, I64), or death from vascular causes (ICD9: 390–459; ICD10: I00–I99) as primary CV endpoints. These were ascertained from the Scottish Morbidity Record 1 (SMR01) data according to the ICD9 or ICD10 codes. CV admission occurred at least 30 days after statin treatment in the statin-exposed group or after the entry date in the statin-unexposed group. Patients having CV admissions within 30 days of statin treatment initiation were excluded from the study. All-cause mortality data were obtained from the General Register Office for Scotland. The same criteria of TC measurement for CV outcome were applied to the all-cause mortality outcome.
Statistical analysis
A sample-size calculation showed that this population-based study had at least a power of 90% at the 5% level of significance to detect a difference of 10% in TC level and a 50% risk reduction in CVD outcome between the statin-exposed and statin-unexposed groups. Data are summarized as mean [standard deviation (SD)] for continuous variables and numbers of patients (percentage) for categorical variables. To examine differences in baseline characteristics between groups, χ2 and t tests were performed. TC concentration changes were calculated as baseline TC concentration minus follow-up TC concentration. A Cox regression model with a time-dependent variable of statin exposure was constructed to analyze the time to APTC event and its components and separately for all-cause mortality and adjusted for potential confounders. Data are expressed as hazard ratios (HR) with 95% confidence intervals (CI). The Cox model assumptions were checked before the analysis. Covariates were age at study entry; gender; socioeconomic status; comorbidities of renal failure, angina, TIA or HF; and use of medications during the follow-up, including analgesics; nonsteroidal anti-inflammatory drugs (NSAIDs); corticosteroids; drugs used to treat diabetes; positive inotropic drugs, diuretics, antiarrhythmic drugs, beta-adrenoceptor-blocking drugs for CVD; drugs such as nitrates and calcium-channel blockers for treating hypertension and heart failure ; other antianginal drugs; anticoagulants; and antiplatelets. The Scottish Index of Multiple Deprivation (SIMD) was used as a measure of socioeconomic status [15]. Sensitivity analyses were performed in patients who had at least two HDL-C concentration measurements or by excluding prevalent statin-exposed patients. In order to control for potential immortal time bias, we conducted an analysis in which patients entered the study on the date of their first cholesterol measurement (a second TC measurement was no longer considered a requirement for entry into the sensitivity analysis cohort). All analyses were carried out using SAS version 9.1. All p values were two-sided.
Results
Primary prevention
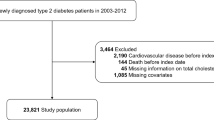
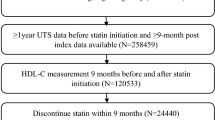
The PP cohort consisted of 5,984 diabetes patients (4,101 in the statin-exposed group and 1,883 in the statin-unexposed group) (Fig. 1); 397 patients who were prescribed other lipid-lowering drugs after the entry date or within 180 days prior to the entry date were excluded from the cohort. Patients in the statin-exposed group were more likely to be older; be female; have higher baseline TC concentration; use more analgesics, drugs in diabetes treatment, corticosteroids, NSAIDs, and CV drugs; and had higher rates of angina, TIA, or HF than those in the statin-unexposed group (Table 1). Statin-associated TC concentration fell by 1.64 mmol/L (95% CI 1.61–1.69) (28%) from baseline of 5.90 mmol/L (SD 1.26) to follow-up concentrations of 4.26 mmol/L (SD 0.92), and this effect was similar regardless of gender (Fig. 2a). TC concentration also fell by approximately 6% in the statin-unexposed group. In the statin-exposed group, 198 patients were prevalent statin users and 3,903 incident statin users. TC reduced by 20% in the prevalent users and 28% in the incident users, with baselines of 5.37 mmol/L (SD 1.48) and 5.93 mmol/L (SD 1.24), respectively.
There were 188 APTC events in the statin-exposed group and 194 in the statin-unexposed group during the 19,067 and 6,595 person years' (PYs) follow-up, respectively. The crude incidence of APTC events per 1,000 PYs was 9.86 (95% CI 8.55-11.38) in the statin-exposed and 29.42 (95% CI 25.55-33.86) in the statin-unexposed group (Table 3). There were 71 non-fatal MI, 63 non-fatal stroke, 101 CV deaths, and 205 all-cause deaths in the statin-exposed group. Correspondingly, the figures were 65, 71, 136, and 289 in statin-unexposed group. The crude event rate for each component of APTC and the crude mortality rate are shown on Table 3. Compared with the statin-unexposed group, statin treatment had a beneficial effect on incident APTC events (adjusted HR 0.36, 95% CI 0.29-0.44). Patients who were older, used anti-arrhythmic drugs, with hospital admission of angina, TIA, or HF during the follow-up had increased risks of CVD. However, patients who were more affluent, used drugs to treat diabetes, hypertension, and heart failure, NSAIDs carried a lower risk of CVD (Table 2). Similar results were observed for each component of APTC event and all-cause mortality (Fig. 3).
Secondary prevention
There were 713 patients (514 statin-exposed and 199 statin-unexposed) with established CVD in this analysis (Fig. 1); 71 patients using other lipid-lowering drugs were excluded from the cohort. Patients in the statin-exposed group were younger, had higher baseline TC concentration, used more NSAIDs, and more CV drugs (Table 1). Figure 2b shows that there was a 23% TC reduction (1.19 mmol/L 95% CI 1.05–1.33) with statin therapy from baseline TC of 5.20 mmol/L (SD 1.36). There was an 8% TC reduction observed in the statin-unexposed group. Similar TC changes in were observed in men and women in statin-exposed (men 24%; women 21%) and statin-unexposed (men 9%; women 7%) groups (Fig. 2b). Fifty patients were prevalent statin users and 464 were incident, with TC reduction of 10% and 24% from baselines of 4.39 mmol/L (SD 1.11) and 5.29 mmol/L (SD 1.36), respectively. Recurrent CV events occurred in 99 statin-exposed and 77 statin-unexposed patients during the respective 2,218 and 624 PYs follow-up, with each crude event rate per 1,000 PYs of 44.63 (95% CI 36.65–54.35) and 123.40 (95% CI 98.70–154.28), respectively (Table 3). For individual APTC endpoint, 29 nonfatal MI, 30 nonfatal stroke, 73 CV deaths, and 106 all-cause deaths occurred in the statin-exposed group. Correspondingly, there were 28, 16, 58, and 94 events in the statin-unexposed group. Table 3 shows the crude event rate for APTC component and the crude mortality rate. Compared with statin-unexposed patients, the risk reduction was 49% for recurrent APTC events (adjusted HR 0.51, 95% CI 0.37–0.71), 62% for recurrent non-fatal MI, and 60% for CV mortality in the statin-exposed group. However, we did not observe a significant risk reduction for recurrent nonfatal stroke (Figs. 3). Older patients; use of positive inotropic drugs; and hospitalization for renal failure, angina, TIA, or HF were associated with an increased risk of CVD. In contrast, patients who were more affluent; used analgesics, hypertension, and heart failure drugs, and corticosteroids had a reduced risk of CVD (Table 2). The risk of all-cause mortality was reduced by 44% with statin use (adjusted HR 0.58, 95% CI 0.42–0.80).
Sensitivity analysis
In patients who had HDL-C measurements available (PP: 3,811 in statin-exposed and 1,690 in statin-unexposed; SP: 459 and 146, respectively) HDL-C concentration increased by 9% from 1.26mmol/L (SD 0.37) at baseline in PP and by 4% from 1.48 mmol/L (SD 0.47) in SP in the statin-exposed group. There was a comparable effect on APTC events, its components, and all-cause mortality as with patients with HDL-C measurements in both PP and SP; adjusted HRs were similar to the main results. HDL-C could be used to guide statin use as well as TC in the absence of LDL-C measurements in patients with diabetes. In the sensitivity analysis excluding prevalent statin-exposed patients, the effect of statins on TC reduction, APTC events, its components, and all-cause mortality were still consistent in both PP and SP and similar to the main findings. The effects of statins on each outcome in both PP and SP were similar to the main findings when we excluded patients who had the baseline TC measurement in the 30 days postdiabetes diagnosis. In the sensitivity analysis using the first TC measurement as the entry date and without considering the second TC measurement, results changed little compared with the findings in our main analysis (adjusted HR: APTC in PP 0.42, 95% CI 0.34–0.52; APTC in SP 0.62, 95% CI 0.44–0.87; all-cause mortality in PP 0.36, 95% CI 0.30-.45; all-cause mortality in SP 0.53, 95% CI 0.40–0.76).
APTC risk reduction per millimole cholesterol reduction
Overall, per millimole TC concentration reduction with statins was associated with 39% risk reductions in incident APTC events (adjusted HR 0.61, 95% CI 0.57–0.66) and 41% in recurrent APTC events (adjusted HR 0.59 95% CI 0.47–0.76) in patients with diabetes.
Discussion
Here we report the effectiveness of statins on TC changes among diabetic patients in the setting of usual care. When results were adjusted for TC concentration changes, the protective effect of statins was still observed on PP and SP of APTC events, nonfatal MI, CV mortality, and all-cause mortality. There was also a risk reduction of incident nonfatal stroke but not of recurrent nonfatal stroke. Compared with results obtained in our previous studies of routinely collected cholesterol data with lipid-lowering drugs in a general healthcare population (approximately 24% reduction) or in statin trial participants (with and without diabetes) (21% reduction in PP or SP) [9], we found similar TC reductions in diabetic patients. One meta-analysis of statin trials among diabetic patients showed that per millimole per liter reduction in LDL-C with statins led to a 9% proportional reduction in all-cause mortality [rate ratio (RR) 0.91, 99% CI 0.82–1.01; p = 0.02) and a 21% proportional reduction in major vascular events (RR 0.79, 99% CI 0.72–0,86) [8]. The proportional effects of statins were similar irrespective of whether there was a prior history of CVD. This study also found reductions in vascular mortality (0.87, 0.76–1.00 p = 0.008), MI or death from coronary disease (0.78, 0.69–0.87), and stroke (0.79, 0.67–0.93). Another systematic review demonstrated 21% risk reductions with lipid-lowering drugs in both incident and recurrent major coronary events in diabetic patients [9]. TC concentration showed a decrease of 15–20% in diabetic groups, which was a little smaller than that in our findings. All these meta-analyses focused on LDL-C reductions, and these reductions accounted for most of the variance in risk reductions of CVD and mortality. Although there were some differences in patient characteristics between randomized controlled trials and the real world, our study results from the trials confirmed the trial findings. This suggests that statin trials in diabetic patients had good external validity.
This population-based cohort study is the first, to our knowledge, to assess statin-associated TC concentrations in diabetic patients with and without prior CVD, and to describe how per millimole TC reductions predicted the risk reduction of incident or recurrent APTC events. Our results supplied evidence supporting the current practice of statin introduction and titration based on TC measurement in the absence of LDL-C measurements. There are several potential limitations of this study: adherence and persistence of statin treatment, statin doses, triglyceride changes, and the effects of lifestyle were not taken into consideration. However, our previous sensitivity analyses of unmeasured risk factors [16] indicate that such factors are unlikely to have a large impact on CV outcomes. We did not use time-dependent variables for other covariates in the study; however, we did not think these would significantly affect our results, as statins act mainly on TC and LDL-C concentrations and are the principle determinants of CV outcome. It is possible that other unmeasured confounders might have influenced the results. To examine the effect of any potential biases not accounted for in the study, and in accordance with the guidelines for Good Pharmacoepidemiology Practices produced by the International Society for Pharmacoepidemiology, we conducted a series of sensitivity analyses to examine the effect of varying the study population inclusion/exclusion criteria, the assumptions regarding exposure, and to control for potential bias [17]. The sensitivity analyses suggested that the main findings of our study were robust. A major strength of our study is the population-based cohort design, with complete follow-up over the study period. This approach allows a normal-care population to be studied, representing all socioeconomic groups and within a universal health care coverage scheme.
In conclusion, statin-associated per millimole TC reduction translated into 39% reductions both in incident and recurrent APTC events in diabetic patients. There was a protective effect on incident and recurrent nonfatal MI and incident nonfatal stroke. Use of statins significantly improved all-cause and CV survival in both PP and SP. Statins were at least as effective in diabetic patients in usual care as in the clinical trials for both primary and secondary prevention. TC changes can also be considered a reasonable measure of statin efficacy in the absence of LDL-C measurement in diabetic patients.
References
Wild S, Roglic G, Green A, Sicree R, King H (May 2004) Global prevalence of diabetes: estimates for 2000 and projections for 2030. Diabetes Care 27(5):1047–53
Grundy SM, Benjamin IJ, Burke GL, Chait A, Eckel RH, Howard BV, Mitch W, Smith SC Jr, Sowers JR (1999 Sep 7) Diabetes and cardiovascular disease: a statement for healthcare professionals from the American Heart Association. Circulation 100(10):1134–46
Haffner SM, Lehto S, Rönnemaa T, Pyörälä K, Laakso M (1998 Jul 23) Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med 339(4):229–34
Morrish NJ, Wang SL, Stevens LK, Fuller JH, keen H (2001) Mortality and causes of death in the WHO Multinational Study of Vascular Disease in Diabetes. Diabetologia 44(2):S14–S21
Haffner SM (1998 Jan) Management of dyslipidemia in adults with diabetes. American Diabetes Association Diabetes Care 21(1):179–82
Goldberg IJ (2001) Clinical review 124: Diabetic dyslipidemia: causes and consequences. J Clin Endocrinol Metab 86(3):965–71
Taskinen MR (2002 May) Diabetic dyslipidemia. Atheroscler Suppl 3(1):47–51
Cholesterol Treatment Trialists' (CTT) Collaborators (2008 Jan 12) Efficacy of cholesterol-lowering therapy in 18,686 people with diabetes in 14 randomised trials of statins: a meta-analysis. Lancet 371(9607):117–25
Costa J, Borges M, David C, Vaz Carneiro A (2006 May 13) Efficacy of lipid lowering drug treatment for diabetic and non-diabetic patients: meta-analysis of randomised controlled trials. BMJ 332(7550):1115–24
Murphy MJ, Wei L, Watson AD, MacDonald TM (2008 Apr) 'Real-life' reduction in cholesterol with statins, 1993 to 2002. Br J Clin Pharmacol 65(4):587–92
Sheng X, Wei L, Murphy MJ, MacDonald TM (2009 Nov) Statins and total (not LDL) cholesterol concentration and outcome of myocardial infarction: results from a meta-analysis and an observational study. Eur J Clin Pharmacol 65(11):1071–80
Wei L, Parkinson J, Macdonald TM (2005) The Tayside Medicines Monitoring Unit (MEMO). In: Strom BL (ed) Pharmacoepidemiology, 4th edn. Wiley, Chichester, pp 323–336
Morris AD, Boyle DI, MacAlpine R, Emslie-Smith A, Jung RT, Newton RW, MacDonald TM (1997 Aug 30) The diabetes audit and research in Tayside Scotland (DARTS) study: electronic record linkage to create a diabetes register. DARTS/MEMO Collaboration BMJ 315(7107):524–8
Classification of Diseases, Functioning, and Disability. http://www.cdc.gov/nchs/icd.htm (accessed 06 Jan 2011)
Scottish Index of Multiple Deprivation. www.scotland.gov.uk/topics/statistics/SIMD (accessed 06 Jan 2011).
Wei L, MacDonald TM, Walker BR (2004) Taking glucocorticoids by prescription is associated with subsequent cardiovascular disease. Ann Intern Med 141:764–70
International Society for Pharmacoepidemiology. Guidelines for Good Pharmacoepidemiology Practices Available from: http://www.pharmacoepi.org/resources/guidelines_08027.cfm. (accessed on 20 Dec 2011)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sheng, X., Murphy, M.J., MacDonald, T.M. et al. Effect of statins on total cholesterol concentrations and cardiovascular outcomes in patients with diabetes mellitus: a population-based cohort study. Eur J Clin Pharmacol 68, 1201–1208 (2012). https://doi.org/10.1007/s00228-012-1234-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-012-1234-5