Abstract
Purpose
The purpose of this study was to evaluate how total cholesterol (TC) concentration in subjects treated with statins predicts myocardial infarction (MI) risk in the absence of low density lipoprotein cholesterol (LDL-C) measurement in clinical trials and in the setting of usual care.
Methods
A systematic review of published English language randomised clinical trials comparing statins with placebo that reported TC changes in subjects with or without prior MI between 1993 and 2008 was carried out using Medline, the Cochrane Library, Web of Science and the ISI Web of Knowledge. In addition, a cohort study of MI patients who had at least two TC measurements in Tayside, Scotland, between 1989 and 2002 was performed. The main outcome was TC concentration changes and risk of subsequent MI.
Results
In the meta-analyses of secondary and primary prevention trials statins decreased TC by 1.54 mmol/L and 1.37 mmol/L versus placebo. Statin-associated TC reduction translated into a risk reduction of 18% per mmol (RR 0.82; 95%CI 0.72–0.93) for secondary prevention and 24% per mmol (RR 0.76; 95%CI 0.62–0.93) for primary prevention. In the cohort study, statin use reduced TC by 0.98 mmol/L compared with non statin-use. Statin use was associated with a 28% reduction (adjusted HR 0.72; 95%CI 0.51–0.98) for recurrent MI.
Conclusions
Total cholesterol measurements can be used with confidence in the absence of LDL measurements to make decisions about statin drug introduction or titration. Randomised trials of statin therapy had good external validity and cholesterol changes and outcomes in trials were comparable to those observed in the setting of usual care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The benefits of lowering cholesterol concentrations with statins in both primary and secondary prevention of coronary heart disease (CHD) have been demonstrated in many studies, which have focussed on the reduction of low density lipoprotein cholesterol (LDL-C) and reductions in cardiovascular disease and all-cause mortality [1–11]. However, in clinical practice clinicians usually base treatment decisions on total cholesterol concentration (TC) ± high density lipoprotein (HDL-C) measurements. We recently performed a population-based study to evaluate the effectiveness of lipid-lowering treatment in the setting of normal care [12]. We observed a net reduction of 1.27 mmol/L in TC concentration in the general population (reduction of 1.65 mmol/L in the treated cohort minus reduction of 0.38 mmol/L in the non-treated cohort), compared with a fall of 1.2 mmol/L seen after 3 years in the Heart Protection Study [1]. We wished to extrapolate this change in total cholesterol to an expected risk reduction, but were surprised to find few data on the relationship between statin-induced reduction in total cholesterol and prevention of subsequent events. Therefore, we performed a meta-analysis and a population-based cohort study to observe how well statin-associated TC changes predict myocardial infarction (MI) risk and to compare the outcomes between the settings of normal care and clinical trials.
Materials and methods
Meta-analysis
Eligibility criteria
-
1.
Randomised controlled trials (RCTs) comparing statins with placebo that evaluated changes in serum cholesterol concentration in subjects with or without MI were eligible.
-
2.
We included only RCTs of at least 4 weeks’ duration.
-
3.
Studies reported on the following outcomes: changes in serum cholesterol concentration, risk of fatal and/or non-fatal MI, and/or death from MI. We excluded studies without information on cholesterol concentrations at baseline and follow-up.
Search strategy
All potentially relevant studies were identified from the electronic databases (Medline, the Cochrane Library, the Web of Science, and the ISI Web of Knowledge). The initial search covered literature published or reported in full in the English language between January 1993 and February 2008 inclusive. Duplication of searching was used. The key search words were lipid-lowering treatment, HMG-CoA reductase inhibitor, statin, pravastatin, simvastatin, atorvastatin, lovastatin, cerivastatin, fluvastatin, cholesterol levels, cholesterol concentrations, TC, LDL, low density lipoprotein, HDL, high density lipoprotein, MI, and coronary heart disease. The title and abstract of studies identified in the computerised search were scanned to exclude any that were clearly irrelevant. The full text of the remaining articles was read to determine whether they contained information on the topic of interest.
Data extraction
The following information was sought from each article: author identification, geographic location of the study, published journal and year, data source, study population, sample size, population characteristics (age mean [SD] or range, sex, race, baseline health characteristics), use of other MI drugs (ACE inhibitors, anticoagulants, antiplatelets, β-blockers), definitions of MI diagnosis, method of data collection, total number of patients in the treatment and placebo/no treatment groups, type and dose of statins (when reported), duration of treatment, baseline and follow-up cholesterol concentrations (TC, LDL-C, HDL-C, TG [triglycerides]), lipid levels change in treated vs placebo/no treatment groups, number and risk of fatal and/or non-fatal MI, risk ratios of MI, death from MI, missing data owing to withdrawal of subjects, and loss to follow-up.
Statistical analysis
For cholesterol concentrations, the weighted mean difference with 95% confidence intervals was calculated by using the values of baseline and follow-up. Differences were calculated as the sum of the differences in the individual studies, weighted by the individual variances for each study. A pooled relative risk with 95% confidence intervals was calculated for dichotomous data (fatal or/and non-fatal MI) by using the Mantel–Haenszel fixed effects model and/or the DerSimonian–Laird random effects model [13]. To determine the presence of heterogeneity across included studies, the Cochrane’s χ2 test (Q-statistics) was used. Meanwhile, inspection of the graphical display was used to examine the heterogeneity. The fixed and random effects models were separately used regarding heterogeneity among the studies.
Observational study
This study was carried out in Tayside, Scotland by using the Medicines Monitoring Unit database. The data collection methods for this database have previously been described [14]. This population-based, record-linkage database contains several datasets, including all dispensed community prescriptions, hospital discharge data, biochemistry results, and other data, which are linked by a unique patient identifier, the Community Health Index (CHI).
Study population and subjects
The study population consisted of residents of Tayside who were registered with a general practitioner between January 1989 and December 2002, and remained resident in Tayside until December 2002 or died during the study period. Patients who were discharged from hospitals after their first MI entered the study. Patients who were discharged in 1998 were excluded because of the incomplete records about statin use in 1998. All MI patients had at least two different TC concentration measurements at entry and at the end of follow-up study. Patients were categorised into two groups according to whether or not they were undergoing statin treatment. Patients who were prescribed a statin after or within 30 days prior to the first discharge from hospital after MI were enrolled in the statin-treated cohort; and those who had never used statins were included in the non-statin-treated cohort. Patients who used other lipid-lowering drugs were excluded from the non-statin-treated group.
TC measurements
Serum measurements of TC between 1989 and 2002 were recorded in the biochemistry database. Baseline TC concentrations were the concentrations measured on or before the date of the first MI in the group that did not undergo statin treatment. Baseline TC was that measured prior to first statin use in the statin-exposed group. Follow-up TC concentrations were the concentrations measured on the dates of re-hospitalisation for MI or within 6 months of these dates in patients with recurrent MI, or the last available measurement in patients without recurrent MI. Follow-up TC concentrations for patients who were followed up to death were the last available TC measurements prior to death.
Outcome variables
The outcomes of the study were TC concentration changes, recurrent MI events and all-cause mortality during the follow-up period. A diagnosis of MI was ascertained from the hospital discharge diagnosis data in the Scottish Morbidity Record coded by primary International Classification of Disease codes (ICD9 and ICD10). Recurrent MI events were excluded from the analysis if the duration between recurrent MI and statin treatment was less than 2 months in the statin-treated cohort; and the duration between recurrent MI and incident MI was less than 2 months in the non-statin-treated cohort. Similar exclusion criteria applied to the all-cause mortality outcome.
Statistical analysis
Total cholesterol changes were calculated as TC at the baseline minus TC at the end of follow-up with results expressed as means (SD). The Cox regression model was used to assess the benefit of statins on recurrent MI or all-cause mortality. The covariates were age at entry, sex, social deprivation category, TC change, and use of drugs (angiotensin converting enzyme inhibitors, anticoagulants, antiplatelet agents, α-blockers, ß-blockers, bronchodilators, calcium channel blockers, cardiac glycosides, diuretics, disease-modifying antirheumatic drugs, nitrates, and hypoglycaemic drugs) during the follow-up period.
Statistical analyses were carried out using SPSS (version 15.0) and Statsdirect.
Results
Meta-analysis
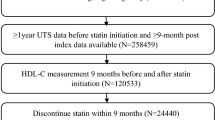
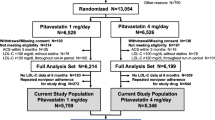
The literature search identified 1,263 articles, of which we excluded 1,232 for the reasons listed in the flow chart (Fig. 1). Full text assessment of the remaining 31 potentially relevant articles resulted in identification of 21 eligible RCTs involving 50,412 participants (25,287 in the primary prevention studies and 25,125 in the secondary prevention studies).
Trial characteristics
The mean or median follow-up ranged from 0.5 to 6.1 years. All studies used a fixed drug dose (generally 40 mg/day of pravastatin, 20 or 40 mg/day of simvastatin or lovastatin, and 40 mg/day of fluvastatin). On average, participants were 60 years old and 15% of them were women (Table 1).
In the 14 secondary prevention studies, patients were randomised to statin treatment or placebo: pravastatin (7 trials and 15,769 participants) [5, 8, 15–19], simvastatin (3 trials and 5,825 participants) [20–22], lovastatin (2 trials and 601 participants) [23, 24], and fluvastatin (2 trials and 794 participants) [25, 26]. The lipid concentrations in both groups were measured and reported in all trials at baseline and the end of follow-up. (Table 2) Nine of the 14 trials provided recurrent MI data. The mean TC, LDL-C, HDL-C and TG levels at baseline ranged from 4.85 to 7.41 mmol/L, 3.15 to 5.08 mmol/L, 0.90 to 1.36 mmol/L and 1.42 to 2.12 mmol/L respectively, and the weighted means in the treated groups were 5.91 mmol/L (SD, 0.15), 3.50 mmol/L (SD, 0.10), 1.02 mmol/L (SD, 0.03) and 1.64 mmol/L (SD, 0.05) respectively in the 14 studies.
In the 7 primary prevention studies, there were 2 trials (7,524 subjects) using lovastatin [27, 28], 2 trials (7,042 subjects) using pravastatin [29, 30], 1 trial using simvastatin [31], and 2 trials (13,143 subjects) using atorvastatin [4, 32]. The numbers of trials reporting lipid concentrations at baseline and follow-up were listed in Table 3. All trials supplied data on the incidence rate of MI. Mean TC, LDL-C, HDL-C and TG concentration at baseline ranged from 5.36 to 6.97 mmol/L, 3.04 to 4.92 mmol/L, 0.94 to 1.30 mmol/L and 1.70 to 3.60 mmol/L respectively, and the weighted means in the treated groups were 5.93 mmol/L (SD, 0.10), 3.89 mmol/L (SD, 0.07), 1.18 mmol/L (SD, 0.02) and 1.84 mmol/L (SD, 0.03) respectively. Cholesterol-weighted means at baseline in placebo groups were similar to those in the treated groups.
Trial outcomes
Cholesterol concentrations
Secondary prevention studies
Mean concentrations of TC, LDL-C, HDL-C and TG at the end of the studies for patients randomised to receive statin therapy ranged from 4.05 to 6.13 mmol/L, 2.18 to 3.72 mmol/L, 0.95 to 1.28 mmol/L and 1.28 to 1.94 mmol/L respectively, and the weighted means were 4.70 mmol/L (SD, 0.12), 2.93 mmol/L (SD, 0.07), 1.08 mmol/L (SD, 0.03), 1.47 mmol/L (SD, 0.04) respectively (Table 2). Thus, of 14 trials, the changes in TC, LDL-C, HDL-C and TG concentrations from baseline for participants receiving treatment ranged from −12% to −32%, −20% to −45%, 5% to 11%, and −7% to −22%. The weighted means of TC, LDL, HDL and TG in the placebo groups were 5.92 mmol/L (SD, 0.21), 4.09 mmol/L (SD, 0.15), 1.03 mmol/L (SD, 0.04) and 1.69 mmol/L (SD, 0.07) respectively after follow-up. The TC and the LDL-C reduction compared with the placebo groups ranged from 13 to 33% and from 21 to 46% respectively. There was an increase in HDL-C concentration with a range of 5 to 12%.
We used a random effects model to calculate the 95% CI of the weighted mean difference in TC, LDL and TG concentrations due to the significant heterogeneity of their outcomes and a fixed effect model for HDL levels due to the absence of heterogeneity of this outcome. Seven trials (3,527 patients) completely reported the means (SD) of all cholesterol levels in treated and placebo groups after follow-up. TC concentrations were significantly lower with statins than with placebo (weighted mean difference −1.54 mmol/L, 95% CI −2.64, −0.43). LDL concentrations were significantly lower with statins than with placebo (weighted mean difference −1.62 mmol/L, 95% CI −2.78, −0.45). We also found a significant reduction in TG levels with statins in comparison to placebo (weighted mean difference −0.31 mmol/L, 95% CI −0.47, −0.14). Statins increased the concentration of HDL with the weighted mean difference being 0.20 mmol/L (95% CI 0.14, 0.27; Table 4).
Primary prevention studies
The mean value of TC, LDL-C, HDL-C and TG concentrations at the end of the study in participants who received statin treatment ranged from 4.12 to 5.59 mmol/L, 2.11 to 3.64 mmol/L, 1.02 to 1.40 mmol/L and 1.29 to 1.61 mmol/L respectively, and the weighted means were 4.69 mmol/L (SD, 0.07), 2.80 mmol/L (SD, 0.05), 1.20 mmol/L (SD, 0.02) and 1.48 mmol/L (SD, 0.02) respectively (Table 3). The percentage changes after follow-up in the treated groups ranged from −17 to −28% for TC, −24 to −35% for LDL-C, 0 to 19% for HDL-C and −10 to −24% for TG. The weighted means of TC, LDL, HDL and TG in the placebo groups were 5.48 mmol/L (SD, 0.08), 3.54 mmol/L (SD, 0.06), 1.17 mmol/L (SD, 0.02) and 1.67 mmol/L (SD, 0.02) respectively after follow-up.
We used the random effects model to calculate the 95% CI of the weighted mean difference in TC, LDL-C and HDL-C due to the significant heterogeneity of their outcomes and the fixed effects model for TG concentrations due to the presence of homogeneity for this outcome. There were significant decreases in TC, LDL-C and TG in the treated groups compared with the placebo groups, with the weighted mean differences −1.37 mmol/L (95% CI −1.93 to −0.82), −1.49 mmol/L (95% CI −2.10 to −0.87) and −0.26 mmol/L (95% CI −0.29 to −0.23) respectively. There was no significant increase in HDL-C after using statins, with the weighted mean difference of 0.12 mmol/L (95% CI −0.04, 0.29).
Risks of MI
Secondary prevention studies
Nine studies reported on the combined outcome of fatal or non-fatal MI. Of the remaining studies, 2 reported coronary events (unstable angina, non-fatal MI or death from CHD), but not MI alone, and 3 studies reported no recurrent MI data in the treated groups. We used the fixed effects model to calculate the pooled risks due to the absence of heterogeneity. In pooled analyses, there were 908 recurrent MIs in 10,090 treated patients and 1,267 in 10,054 placebo patients. Statin therapy reduced the risk of MI by 28% (RR, 0.72; 95% CI, 0.63–0.82, P = 0.004), with absolute risk reduction (ARR) of 3.6% in the secondary prevention studies (Fig. 2).
Primary prevention studies
In pooled analyses, there were 295 first MIs in 14,015 treated subjects and 437 in 13,948 placebo subjects. Statin treatment reduced the incidence of MI by 33% (fixed effects model: RR, 0.67; 95% CI, 0.55–0.82, P = 0.01), with an ARR of 0.9% in the primary prevention studies (Fig. 3).
MI risk reduction per mmol/L of cholesterol reduction
Overall, in the secondary prevention studies, a 28% reduction of risk of recurrent MI was observed for every 1.54 mmol/L, 1.62 mmol/L and 0.31 mmol/L reduction in TC, LDL-C and TG levels, and for every 0.20 mmol/L increase in HDL-C levels. Thus, recurrent MI was reduced by 18% per mmol reduction in TC.
In the primary prevention studies a 33% reduction of risk of incident MI was found for every 1.37 mmol/L, 1.49 mmol/L, and 0.26 mmol/L reduction in TC, LDL-C and TG levels. Thus incident MI was reduced by 24% per mmol reduction in TC.
Observational study
There were 2,759 patients (1,703 in the statin-treated cohort and 1,056 in the non-statin-treated cohort) included in the study. The baseline and follow-up TC levels are listed in Table 5. TC concentration reductions from baseline to the end of follow-up for recurrent MI and death were 1.41 mmol/L (SD 1.29) or 24% and 1.43 mmol/L (SD 1.29) or 24% in the statin-treated cohort, and 0.43 mmol/L (SD 1.08) or 8% and 0.48 mmol/L (SD 1.10) or 9% in the non-statin-treated cohort. There were 95 recurrent MIs and 117 deaths in the treated cohort and 112 and 155 in the non-statin-treated cohort. Statin treatment was significantly associated with decreased risk of recurrent MI (unadjusted hazards ratio [HR], 0.53, 95% CI 0.41–0.68). After adjustment for the covariates, the benefit of statin treatment remained significant (adjusted HR, 0.72, 95% CI 0.51–0.98). However, there was no effect of statin treatment on all-cause mortality after adjusting for the available confounders (adjusted HR, 1.06, 95% CI 0.76–1.47).
Discussion
Key findings
We carried out the present study because we could not find meta-analysis data on the relationship between TC changes with statin therapy and MI. We found this surprising as most clinical decisions in the UK are based on TC concentrations supplemented where available by HDL-C measurements, with few centres directly measuring LDL-C.
The present paper reports our findings of the effect on MI of changes in TC in RCTs and in an observational study. Both types of study show that the changes in TC concentrations by statin treatment were similar to the results obtained in our previous study of routinely collected biochemistry data in a general healthcare population. In the observational study TC reductions occurred in both the statin-treated and non-treated patients. In addition, TC reductions observed in the statin-treated patients were similar to those seen in RCTs.
Comparison with other review studies
The result of our review also confirms the findings of a previous review, which showed that a reduction in LDL-C of 1 mmol/L using lipid-lowering drugs leads to reductions of 26% in the incidence of non-fatal MI (RR, 0.74, 99%CI, 0.70–0.79) [10]. However, this previous review focused on LDL-C because its reduction accounted for most of the variance in risk reductions for overall mortality and cardiovascular endpoints. Another review identified trials of lipid-lowering agents (non-statin and statin) reporting changes in HDL-C levels and CHD risk [33]. Although this review supplied data on reductions of TC (32%), reductions in LDL-C levels (45%) and the increase in HDL-C levels (<10%) after statin therapy, it only analysed CHD mortality and morbidity versus the HDL-C effect, which was not a significant linear predictor of CHD risk reduction. A third review addressed the use of statins in the primary and secondary prevention of CHD and ischaemic stroke [11]. However, there were no separate data quoted on TC change and MI outcome in this review paper.
Comparison between meta-analysis and observational studies
Our meta-analysis showed a reduction of 1.21 mmo/L (5.91 mmol/L minus 4.70 mmol/L) in mean TC in the statin-treated group in the secondary prevention trials. However, our observational study showed a reduction of 1.41 mmol/L (SD 1.29), which was similar to that found in a population level study [12]. This better outcome could be due to patient characteristic differences [34]. Our meta-analysis also found that the mean TC increased by 0.01 mmol/L (5.92 mmol/L minus 5.91 mmol/L) in the placebo-treated patients at the end of follow-up in trials. In contrast, TC concentration decreased in the non-statin-treated patients in our current observational cohort study (0.43 mmol/L). This difference may be because all risk factors were well balanced in clinical trials while some factors such as increased awareness of CHD prevention and lifestyle changes may have contributed to the population cholesterol reductions.
Strengths and limitations
This meta-analysis and population-based cohort study are the first, to our knowledge, to assess the relationship between TC concentration changes associated with using statins in patients with and without MI, and to describe how TC reduction predicted the risk reduction of recurrent or incident MI. The results of our meta-analysis were similar to those observed in our cohort study. This demonstrates that statin trials had good external validity. Thus, the benefits of statins seen in the RCTs can probably be extended to the general population, although there were some differences in patient characteristics between RCTs and the real world. The results of the present study would seem to justify the current practice of introducing and titrating statin therapy based on the measurement of TC without the measurement of LDL cholesterol.
One limitation of the present meta-analysis is the lack of complete data on every outcome from every trial. For example, in some trials there was no information on cholesterol concentrations in the placebo group during follow-up. Another limitation is that some of the RCTs had small sample sizes. Also the majority of studies focused on male participants so females are under-represented. There is also the possibility of publication bias because information on unpublished papers and ongoing RCTs was not sought. This review was also limited to the English-language literature and the available databases. Additionally, the effect of lipid-lowering drugs in clinical trials might be overestimated because of the higher adherence to treatment by patients compared with observational studies. The limitations of the observational study were that the adherence to statin treatment, the dosages and duration of statin treatment, and the effects of lifestyles were not taken into consideration. The serious side effects of statins such as rhabdomyolysis were not compared between the clinical trials and the Tayside cohort because of the relatively small size of the Tayside cohort. There may be differences in serious side effects of statins between RCTs and an unselected general population due to stringent inclusion and exclusion criteria in RCTs. However, previous studies have shown that the incidence of rhabdomyolysis was about 0.01% in a meta-analysis of clinical trials [10] and 0.44 per 10,000 patients in a population-based study of 252,460 patients [35].
Conclusion
Our analysis has found that TC reductions as a result of statin use is a reasonable measure of their efficacy in the setting of clinical trials. Furthermore, the findings of clinical trials of statins are comparable to those observed in the general population.
References
Collins R, Armitage J, Parish S, Sleight P, Peto R, Heart Protection Study Collaborative Group (2002) MCR/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20536 high-risk individuals. Lancet 360:7–22
Sacks FM, Moye LA, Davis BR, Cole TG, Rouleau JL, Nash DT, Pfeffer MA, Braunwald E (1998) Relationship between plasma LDL concentrations during treatment with pravastatin and recurrent coronary events in the cholesterol and recurrent events trial. Circulation 97(15):1446–1452
Long-term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group (2002) Long-term effectiveness and safety of pravastatin in 9014 patients with coronary heart disease and average cholesterol concentrations. Lancet 359:1379–1387
Sever PS, Dahlöf B, Poulter NR, Wedel H, Beevers G, Caulfield M, Collins R, Kjeldsen SE, Kristinsson A, McInnes GT, Mehlsen J, Nieminen M, O'Brien E, Ostergren J (2003) ASCOT investigators. Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial-Lipid Lowering Arm (ASCOT-LLA). Lancet 361:1149–1158
Sacks FM, Pfeffer MA, Moye LA, Rouleau JL, Rutherford JD, Cole TG, Brown L, Warnica JW, Arnold JM, Wun CC, Davis BR, Braunwald E (1996) The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial investigators (CARE). N Engl J Med 335(14):1001–1009
Shepherd J, Blauw GJ, Murphy MB, Bollen EL, Buckley BM, Cobbe SM, Ford I, Gaw A, Hyland M, Jukema JW, Kamper AM, Macfarlane PW, Meinders AE, Norrie J, Packard CJ, Perry IJ, Stott DJ, Sweeney BJ, Twomey C, Westendorp RG (2002) Pravastatin in elderly individuals at risk of vascular disease (PROSPER). Lancet 360:1623–1630
Serruys PW, de Feyter P, Macaya C, Kokott N, Puel J, Vrolix M, Branzi A, Bertolami MC, Jackson G, Strauss B, Meier B, Lescol Intervention Prevention Study, Lescol Intervention Prevention Study (LIPS) Investigators (2002) Fluvastatin for prevention of cardiac events following successful first percutaneous coronary intervention: a randomized controlled trial. JAMA 287:3215–3222
The Long-term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group (1998) Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med 339:1349–1357
Shepherd J, Cobbe SM, Ford I, Isles CG, Lorimer AR, MacFarlane PW, McKillop JH, Packard CJ, West of Scotland Coronary Prevention Study Group (1995) Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. N Engl J Med 333:1301–1307
Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, Kirby A, Sourjina T, Peto R, Collins R, Simes R, Cholesterol Treatment Trialists’ (CTT) Collaborators (2005) Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90 056 participants in 14 randomised trials of statins. Lancet 366(9493):1267–1278
Vrecer M, Turk S, Drinovec J, Mrhar A (2003) Use of statins in primary and secondary prevention of coronary heart disease and ischemic stroke. Meta-analysis of randomized trials. Int J Clin Pharmacol Ther 41(12):567–577
Murphy MJ, Wei L, Waston AD, Macdonald TM (2008) ‘Real-life’ reduction in cholesterol with statins, 1993 to 2002. Br J Clin Pharmacol 65(4):587–592
Blettner M, Sauerbrei W, Schlehofer B, Scheuchenpflug T, Friedenreich C (1999) Traditional reviews, meta-analyses and pooled analyses in epidemiology. Int J Epidemiol 28:1–9
Wei L, Parkinson J, Macdonald TM (2005) The Tayside Medicines Monitoring Unit (MEMO). In: Strom BL (ed) Pharmacoepidemiology, 4th edn. Wiley, Chichester, pp 323–336
Tamura A, Mikuriya Y, Nasu M (1997) Effect of pravastatin (10 mg/day) on progression of coronary atherosclerosis in patients with serum total cholesterol levels from 160 to 220 mg/dl and angiographically documented coronary artery disease. Coronary Artery Regression Study (CARS) Group. Am J Cardiol 79(7):893–896
The Pravastatin Multinational Study Group for Cardiac Risk Patients (1993) Effects of pravastatin in patients with serum total cholesterol levels from 5.2 to 7.8 mmol/liter (200 to 300 mg/dl) plus two additional atherosclerotic risk factors. Am J Cardiol 72(14):1031–1037
Pitt B, Mancini GB, Ellis SG, Rosman HS, Park JS, McGovern ME (1995) Pravastatin limitation of atherosclerosis in the coronary arteries (PLAC I): reduction in atherosclerosis progression and clinical events. PLAC I investigation. J Am Coll Cardiol 26(5):1133–1139
Crouse JR III, Byington RP, Bond MG, Espeland MA, Craven TE, Sprinkle JW, McGovern ME, Furberg CD (1995) Pravastatin, lipids, and atherosclerosis in the carotid arteries (PLAC-II). Am J Cardiol 75(7):455–459
Jukema JW, Bruschke AV, van Boven AJ, Reiber JH, Bal ET, Zwinderman AH, Jansen H, Boerma GJ, van Rappard FM, Lie KI (1995) Effects of lipid lowering by pravastatin on progression and regression of coronary artery disease in symptomatic men with normal to moderately elevated serum cholesterol levels. The Regression Growth Evaluation Statin Study (REGRESS). Circulation 91(10):2528–2540
Scandinavian Simvastatin Survival Study Group (1994) Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Atheroscler Suppl 5(3):81–87
MAAS Investigators (1994) Effect of simvastatin on coronary atheroma: the Multicentre Anti-Atheroma Study (MAAS). Lancet 344(8923):633–638
Teo KK, Burton JR, Buller CE, Plante S, Catellier D, Tymchak W, Dzavik V, Taylor D, Yokoyama S, Montague TJ (2000) Long-term effects of cholesterol lowering and angiotensin-converting enzyme inhibition on coronary atherosclerosis: the Simvastatin/Enalapril Coronary Atherosclerosis Trial (SCAT). Circulation 102(15):1748–1754
Blankenhorn DH, Azen SP, Kramsch DM, Mack WJ, Cashin-Hemphill L, Hodis HN, DeBoer LW, Mahrer PR, Masteller MJ, Vailas LI, Alaupovic P, Hirsch LJ; MARS Research Group (1993) Coronary angiographic changes with lovastatin therapy. The Monitored Atherosclerosis Regression Study (MARS). Ann Intern Med 119(10):969–976
Waters D, Lespérance J, Gladstone P, Boccuzzi SJ, Cook T, Hudgin R, Krip G, Higginson L (1996) Effects of cigarette smoking on the angiographic evolution of coronary atherosclerosis. A Canadian Coronary Atherosclerosis Intervention Trial (CCAIT) Substudy. CCAIT Study Group. Circulation 94(4):614–621
Herd JA, Ballantyne CM, Farmer JA, Ferguson JJ III, Jones PH, West MS, Gould KL, Gotto AM Jr (1997) Effects of fluvastatin on coronary atherosclerosis in patients with mild to moderate cholesterol elevations (Lipoprotein and Coronary Atherosclerosis Study [LCAS]). Am J Cardiol 80:278–286
Riegger G, Abletshauser C, Ludwig M, Schwandt P, Widimsky J, Weidinger G, Welzel D (1999) The effect of fluvastatin on cardiac events in patients with symptomatic coronary artery disease during one year of treatment. Atherosclerosis 144(1):263–270
Furberg CD, Adams HP Jr, Applegate WB, Byington RP, Espeland MA, Hartwell T, Hunninghake DB, Lefkowitz DS, Probstfield J, Riley WA (1994) Effect of lovastatin on early carotid atherosclerosis and cardiovascular events. Asymptomatic Carotid Artery Progression Study (ACAPS) research group. Circulation 90(4):1679–1687
Downs JR, Clearfield M, Weis S, Whitney E, Shapiro DR, Beere PA, Langendorfer A, Stein EA, Kruyer W, Gotto AM Jr (1998) Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/TexCAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study. JAMA 279(20):1615–1622
Salonen R, Nyyssönen K, Porkkala E, Rummukainen J, Belder R, Park JS, Salonen JT, Kuopio Atherosclerosis Prevention Study (KAPS) (1995) A population-based primary preventive trial of the effect of LDL lowering on atherosclerotic progression in carotid and femoral arteries. Circulation 92(7):1758–1764
Shepherd J, Cobbe SM, Ford I, Isles CG, Lorimer AR, MacFarlane PW, McKillop JH, Packard CJ (2004) Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. Atheroscler Suppl 5(3):91–97
Bestehorn HP, Rensing UF, Roskamm H, Betz P, Benesch L, Schemeitat K, Blümchen G, Claus J, Mathes P, Kappenberger L, Wieland H, Neiss A (1997) The effect of simvastatin on progression of coronary artery disease. The Multicenter Coronary Intervention Study (CIS). Eur Heart J 18(2):226–234
Colhoun HM, Betteridge DJ, Durrington PN, Hitman GA, Neil HA, Livingstone SJ, Thomason MJ, Mackness MI, Charlton-Menys V, Fuller JH, CARDS investigators (2004) Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study (CARDS): multicentre randomised placebo-controlled trial. Lancet 364(9435):685–696
Dean BB, Borenstein JE, Henning JM, Knight K, Merz CN (2004) Can change in high-density lipoprotein cholesterol levels reduce cardiovascular risk? Am Heart J 147(6):966–976
Wei L, Ebrahim S, Bartlett C, Davey PD, Sullivan FM, MacDonald TM (2005) Statin use in the secondary prevention of coronary heart disease in primary care: cohort study and comparison of inclusion and outcome with patients in randomized trials. BMJ 330:821
Graham DJ, Staffa JA, Shatin D, Andrade SE, Schech SD, La Grenade L, Gurwitz JH, Chan KA, Goodman MJ, Platt R (2004) Incidence of hospitalized rhabdomyolysis in patients treated with lipid-lowering drugs. JAMA 292(21):2585–90
Acknowledgements
LW holds a Special Training Fellowship in Health Services and a Health of the Public Research Award from the Medical Research Council, UK.
Competing interests
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sheng, X., Wei, L., Murphy, M.J. et al. Statins and total (not LDL) cholesterol concentration and outcome of myocardial infarction: results from a meta-analysis and an observational study. Eur J Clin Pharmacol 65, 1071–1080 (2009). https://doi.org/10.1007/s00228-009-0720-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-009-0720-x