Abstract
Purpose
The pathogenic role of angiotensin-converting enzyme (ACE) inhibition in hypertensive patients regarding endothelial progenitor-cell (EPC) function is still poorly understood. The aim of the study was to evaluate EPC number, function, and relationship to carotid intima media thickness (IMT) progression.
Methods
We studied 36 newly diagnosed mildly hypertensive patients free of cardiovascular disease and related risk factors without prior or concurrent therapy with ACE inhibitors. Patients were randomized to receive enalapril 20 mg/day (n = 18) or zofenopril 30 mg/day (n = 18). EPC number and migrating capacity, plasma nitrite and nitrate (NOx), and isoprostane concentrations were evaluated. Carotid IMT was determined by ultrasonography at baseline and after 1 and 5 years of follow-up.
Results
EPC number increased during the follow-up, with no statistical differences between treatment groups. There was an inverse correlation between circulating EPCs and IMT increase over time. Plasma NOx decreased during the study without evident differences between treatment groups. Isoprostanes decreased more markedly in zofenopril-treated patients. Multiple linear regression model demonstrated that carotid IMT was significantly inversely correlated with EPC but not with migratory cells after adjusting for confounders.
Conclusions
The study demonstrated that EPC levels increased during the follow-up in both groups of newly diagnosed hypertensive patients treated with ACE inhibitors. These drugs prevented progression of vascular damage, with an inverse correlation between circulating EPC levels and IMT values.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the last decade, there was a growing interest in regenerative medicine afforded by findings related to endothelial progenitor cells (EPCs) from bone marrow origin [1, 2]. Thus, the pathobiology of EPC is an emerging field in the clinical setting of cardiovascular diseases. It has been hypothesized that EPC depression can be causally linked to the atherogenic process [3]. EPCs constitute a circulating pool of cells that are able to repair the dysfunctional endothelium, whereas a reduced EPC pool may determine the inability to maintain adequate endothelial homeostasis. Moreover, the number and functional activity of EPCs have been reported to decrease with hypertension, diabetes mellitus, and coexistence of multiple classical cardiovascular risk factors [4–11]. Levels of EPCs are also inversely correlated with progression of coronary artery disease (CAD) [12]. Some preclinical studies suggest that angiotensin-converting enzyme (ACE) inhibition may have potential effects on EPC [13–15]. As ACE inhibitors are widely used in cardiovascular therapy, this promoted further investigation into the effects of such compounds on circulating EPC and their role in vascular healing, repair, and postnatal neovascularization. ACE inhibitors may have a pivotal role in managing atherosclerotic-related diseases independent of their vasodilating and hypotensive effects. Experimental studies show that these drugs can attenuate the development of atherosclerosis in a wide range of species and that the most effective are those containing the antioxidant sulfhydryl group [16–20]. We used a previous clinical trial [21] on ACE inhibition and vascular damage to study EPC number, function, and relation to carotid intima media thickness (IMT) progression over time.
Methods
Participants and measurements
We studied 36 newly diagnosed mildly hypertensive patients who participated in a previously published and ongoing study [21] involving 48 patients that began in 2001. Exclusion criteria were presence of other classical risk factors for CAD (e.g., diabetes/impaired glucose tolerance and hyperlipidemia); prior or concurrent therapy with ACE inhibitors, antiplatelet drugs, or anticoagulants; history of ischemic events; refusal to grant informed consent. Patients were enrolled if they had systolic blood pressure (BP) >160 mmHg and/or diastolic BP >95 mmHg. Hyperlipidemia was defined as having total cholesterol >220 mg/dl, low-density lipoprotein (LDL) cholesterol >140 mg/dl, and triglyceride >150 mg/dl, and/or taking antihyperlipidemic medications. We used a simple randomization scheme with treatment assignment determined by computerized random number generation in a sequential manner that was then provided to the clinical investigators in sealed envelopes. Follow-up measurements were scheduled at 1 and 5 years. The trial protocol followed the principles outlined in the Declaration of Helsinki and was approved by the local ethical committee.
Carotid ultrasonography measurements
All carotid ultrasonography measurements were made by two investigators (GB and AL) to eliminate interobserver variability and who were blinded to treatment randomization, as previously described [21]. Carotid artery IMT was measured by high-resolution B-mode ultrasonography with a 7.5-MHz high-resolution transducer (Sonos-5500 system; Philips Medical Systems, Andover, MA, USA), as described previously [22, 23]. The carotid arteries were carefully examined in the longitudinal and transverse views for wall changes. The common carotid artery, carotid bulb, and internal and external arteries were examined. Presence of carotid atherosclerotic lesions (plaques or shadowing) was determined from scans of all right and left carotid artery segments (common carotid artery, bifurcation, and internal carotid artery). The presence of plaques was defined during ultrasound reading based on wall thickness and arterial-wall roughness, loss of alignment, or protrusion into the lumen. Calcification or mineralization, another indicator of atherosclerosis, was based on acoustic shadowing. Right and left common carotid artery-wall areas were calculated as the total artery area minus the lumen area, assuming a circular lumen and an outer artery structure that was either circular or elliptical. The IMT of the far wall was defined as the distance from the lumen–intima interface (leading edge of the first echogenic line) to the media–adventitia interface (leading edge of the second echogenic line). We measured IMT of the common carotid arteries bilaterally at three points (1, 2, and 3 cm proximal to the carotid bifurcation); the averaged value was taken as the carotid IMT. IMT values for the three different projections were averaged to obtain the mean maximum IMT (MM-IMT). Lesions of apparent plaque appearing either as faint gray echoes (soft plaques) or bright white echoes (calcified plaque) protruding into the lumen were always excluded from IMT measurement [24].
Blood pressure measurements
BP was measured at baseline and during the two subsequent examinations with a mercury sphygmomanometer in a standardized fashion after 10 min of rest with the patient in the supine position [25]. Systolic and diastolic BPs (mmHg) were defined according to Korotkoff sounds I and V. All BP measurements were done by a physician blinded to patients' profiles and treatment assignments just before carotid ultrasound measurements and after drug administration.
Evaluation of plasma nitrite and nitrate and isoprostane concentrations
Plasma nitrite and nitrate (NOx) levels were measured with the classical Griess method, as previously described [25]. Amounts of plasma nitrite were estimated by a standard curve obtained from enzymatic conversion of sodium nitric oxide (NaNO3) to nitrite. Isoprostanes [8-iso-PGF2-α] were measured from plasma samples using a commercially available immunoassay (Cayman Chemical, Ann Arbor, MI, USA) according to the manufacturer’s instructions [25].
Measurement of EPC number (culture assay)
Mononuclear cells were isolated by density-gradient centrifugation with Biocoll (Biochrom, Berlin, Germany) from 20 ml peripheral blood, as previously described [26]. After isolation, 4 × 106 mononuclear cells were plated on 24-well culture dishes coated with human ibronectin (Sigma-Aldrich, Munich, Germany) and maintained in endothelial basal medium (Cambrex, Walkerville, MD, USA) supplemented with endothelial growth medium and 20% fetal calf serum. After 4 days in culture, nonadherent cells were removed by thorough washing with phosphate-buffered saline (PBS).
Measurement of functional capacity of EPCs (migrating capacity)
Isolated EPCs were detached using 1 mmol/L ethylenediaminetetraacetic acid (EDTA) in PBS (pH 7.4), harvested by centrifugation, resuspended in 500 μl endothelial basal medium, counted, and placed in the upper chamber of a modified Boyden chamber (2 × 104 cells; BD Bioscience, Milan, Italy). The chamber was placed in a 24-well culture dish containing endothelial basal medium, 20% fetal calf serum, and human recombinant vascular endothelial growth factor (VEGF) (50 ng/ml; R&D Systems, Minneapolis, MN, USA). After 24-h incubation at 37°C, the lower side of the filter was washed with PBS and fixed with 2% paraformaldehyde. For quantification, cell nuclei were stained with 4',6'-diamidino-2-phenylindole. Cells migrating into the lower chamber were counted manually in several random microscopic fields. [26] Measurements were blinded to treatment randomization
Statistical analysis
Data are presented as mean ± standard deviation (SD). Analysis of variance (ANOVA) for repeated measures was used to test the effect of treatment (enalapril vs zofenopril) over time (baseline, 1 year, 5 years) on systolic and diastolic BP, IMT, EPCs, migratory cells, NOx, and PGF2-α and showed statistical significance for treatment effect, time effect, and interaction between treatment and time. To assess the association between IMT vs EPC and/or migratory cells controlling for confounder effect of treatment, time, and other variables, we used linear regression analysis with robust variance estimation clustering for each patient to compensate for the correlation between repeated measures [27]. A p value < 0.05 was considered statistically significant. Analysis was performed using STATA 10 software.
Results
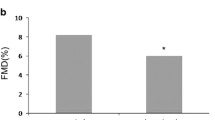
Mean patient age was 41.6 ± 2.6 (range 36–46) years. No significant difference in age, gender, family history of an ischemic event (CAD, peripheral arterial disease, or stroke), history of smoking, sedentary lifestyle, or medication used (calcium antagonist: two in enalapril and two in zofenopril groups) were present at baseline between the two groups [21]. Moreover, no differences were present for others risk factors, such as total cholesterol, triglycerides, high-density lipoprotein (HDL) cholesterol, or LDL cholesterol [21]. No patient had diabetes or was in treatment with statin or aspirin. Compliance to pharmacological treatment was good, with no withdrawals during the follow-up period. EPCs increased during the follow-up, with no statistical differences between treatment groups. Migrating capacity of EPCs did not change during the study, and no differences were evident between treatment groups. Plasma NOx decreased significantly, whereas no differences were evident between the treatment groups. PGF2-α decreased significantly, most markedly in zofenopril-treated patients. IMT increased, and this effect was more evident in the group of patients treated with enalapril, even though this difference did not reach statistical significance when compared with the zofenopril-treated group. A statistically significant interaction between treatments and time suggested a time-related effect of pharmacological treatment in reducing IMT progression. As expected, a significant reduction of systolic and diastolic BP was obtained, with no statistical differences between treatment groups, even considering the effect of interaction between treatment and time (Table 1 and Fig. 1).
To assess the correlation between IMT and EPCs and migratory cells adjusted for all other covariates, we built a multiple linear regression model, with IMT as independent variable and EPC and migratory cells as effect modifiers and all the remaining variables as confounder. The multiple linear regression model showed that IMT was significantly inversely correlated with EPC but not with migratory cells after adjustment for confounders (Table 2 and Fig. 2).
Discussion
The major findings of our study are: (1) an EPC increase during the follow-up in both groups of patients treated with enalapril and zofenopril, (2) an inverse correlation between circulating EPCs and IMT increase over time, (3) a plasma NOx decrease without evident differences between treatment groups, and (4) 8-iso-PGF2-α decrease more evidently in zofenopril-treated patients. Migrating capacity of EPCs did not change during the study, and no differences were evident between treatment groups. Multivariate analysis demonstrated that vascular damage was significantly inversely correlated with EPC levels but not with migrating capacity after adjustment for confounders. A previous cross-sectional study demonstrated an association of EPC migration, age, and mean arterial BP on carotid IMT. They also found an inverse correlation with EPC number (r = −0.349) but with no statistical significance (p = 0.063), demonstrating an age-related decrease in EPC function and a possible effect on vascular remodelling.[28] Another study [29] demonstrated that a significantly higher carotid mean maximum IMT, prevalence of carotid plaque, and a lower number of circulating CD34+/KDR+ EPCs was found in stroke patients compared with controls. In stroke patients, circulating CD34+/KDR+ EPCs count correlated negatively with carotid IMT and was an independent risk factor for increased carotid IMT > 1 mm and the presence of carotid plaque. Another very recent study [30] established that telmisartan shows a more potent anti-inflammatory effect than does the ACE inhibitor ramipril, and the two drugs showed no differential effects on EPCs. As ACE expression may regulate primitive hemangioblasts derived from human stem cells [14], the renin-angiotensin-aldosterone axis can be therefore exploited to direct the EPC fate during vascular regeneration. This issue may constitute an important clinical implication of ACE therapy on vascular damage occurring in hypertensive patients. ACE inhibitors may have a pivotal role in managing atherosclerotic-related diseases independent of their vasodilating and hypotensive effects. Experimental studies showed that these drugs can attenuate the development of atherosclerosis in a wide range of species, the most effective drugs being those containing the antioxidant sulfhydryl group [16–20]. Different ACE inhibitors have quite different chemical functional groups, and these structural variations may account for different in vivo and in vitro effects. The ACE inhibitor captopril has a sulfhydryl group to coordinate the zinc ion of the active site, enalaprilat has a carboxylate group, and zofenopril has two sulfhydryl groups [31, 32]. Sulfhydryl ACE inhibition stimulates NOx activity and decreases oxidative stress in human endothelial cells [33] and in patients with essential hypertension [21]. Zofenopril increases NOx production in endothelium, decreases atherosclerotic development, and reduces reactive oxygen species [34–37], as well as susceptibility to oxidation of plasma LDL and oxidation-specific epitope formation in the arterial wall and atherogenesis in apolipoprotein-E knockout mice [35]. The meaning of NOx levels would be qualitative rather than quantitative. However, repeated assays in the same subjects have high sensitivity. In the present study, as expected, untreated hypertension was associated with increased levels of NOx. After both treatment regimens, NOx levels decreased, indicating that BP normalization was associated with restoring effects of the NOx pathway.
Circulating EPCs could play an important role in accelerating endothelialization in areas of vascular damage, and EPC function would be a viable strategy for assessing reparative ability. Consistently, some studies established that EPCs are affected both in number and function by several cardiovascular risk factors and various cardiovascular disorders, such as hypertension, hypercholesterolemia, and CAD [38].
Our study had some limitations. First, we used plasma storage collected from another clinical trial [21]. Another is the limited power of the study due to a small group of patients. In conclusion, our study demonstrated that EPC levels increased during treatment in both groups of patients treated with ACE inhibitors, indicating that these drugs prevent vascular damage in newly hypertensive patients, not only by reducing BP but also acting on circulating EPCs.
References
Napoli C, Balestrieri A, Ignarro LJ (2007) Therapeutic approaches in vascular repair induced by adult bone marrow cells and circulating progenitor endothelial cells. Curr Pharm Des 13:3245–3251
Napoli C, Cacciatore F (2009) Novel pathogenic insights in the primary prevention of cardiovascular disease. Prog Cardiovasc Dis 51:503–523
Fadini GP, Coracina A, Baesso I et al (2006) Peripheral blood CD34+ KDR+ endothelial progenitor cells are determinants of subclinical atherosclerosis in a middle-aged general population. Stroke 37:2277–2282
Heitzer T, Schlinzig T, Krohn K, Meinertz T, Munzel T (2001) Endothelial dysfunction, oxidative stress, and risk of cardiovascular events in patients with coronary artery disease. Circulation 104:2673–2678
Vasa M, Fichtlscherer S, Aicher A et al (2001) Number and migratory activity of circulating endothelial progenitor cells inversely correlate with risk factors for coronary artery disease. Circ Res 89:E1–E7
Liguori A, Fiorito C, Balestrieri ML et al (2008) Functional impairment of hematopoietic progenitor cells in patients with coronary heart disease. Eur J Haematol 80:258–264
Kinnaird T, Stabile E, Zbinden S, Burnett MS, Epstein SE (2008) Cardiovascular risk factors impair native collateral development and may impair efficacy of therapeutic interventions. Cardiovasc Res 78:257–264
Spinetti G, Kraenkel N, Emanueli C, Madeddu P (2008) Diabetes and vessel wall remodelling: from mechanistic insights to regenerative therapies. Cardiovasc Res 78:265–273
Feihl F, Liaudet L, Levy BI, Waeber B (2008) Hypertension and microvascular remodelling. Cardiovasc Res 78:274–285
Lijnen HR (2008) Angiogenesis and obesity. Cardiovasc Res 78:286–293
Balestrieri ML, Rienzo M, Felice F et al (2008) High glucose downregulates endothelial progenitor cell number via SIRT1. Biochim Biophys Acta 1784:936–994
Briguori C, Testa U, Riccioni R et al (2010) Correlations between progression of coronary artery disease and circulating endothelial progenitor cells. FASEB J 24:1981–1988
You D, Cochain C, Loinard C et al (2008) Combination of the Angiotensin-Converting Enzyme inhibitor Perindropil and diuretic indapamide activate postnatal vasculogenesis in spontaneously hypertensive rats. J Pharmacol Exp Ther 325:766–773
Zambidis ET, Park TS, Yu W et al (2008) Expression of angiotensine-converting enzyme (CD 143) identifies and regulate primitive hemangioblasts derived from human pluripotent stem cells. Blood 112:3601–3614
Muller P, Kazalov A, Jagoda P, Semenov A, Bohm M, Laufs U (2009) ACE inhibition promotes upregulation of endothelial progenitor cells and neoangiogenesis in cardiac pressure overload. Cardiovasc Res 83:106–114
Napoli C, Cicala C, D'Armiento FP et al (1999) Beneficial effects of ACE-inhibition with zofenopril on plaque formation and low-density lipoprotein oxidation in Watanabe heritable hyperlipidemic rabbits. Gen Pharmacol 33:467–477
Chobanian AV, Haudenschild CC, Nickerson C, Drago R (1990) Antiatherogenic effect of captopril in the Watanabe heritable hyperlipidemic rabbit. Hypertension 15:327–331
Hayek T, Attias J, Smith J, Breslow JL, Keidar S (1998) Antiatherosclerotic and antioxidative effects of captopril in apolipoprotein E-deficient mice. J Cardiovasc Pharmacol 31:540–544
Sun YP, Zhu BQ, Browne AE et al (2001) Comparative effects of ACE inhibitors and an angiotensin receptor blocker on atherosclerosis and vascular function. J Cardiovasc Pharmacol Ther 6:175–181
Candido R, Jandeleit-Dahm KA, Cao Z et al (2002) Prevention of accelerated atherosclerosis by angiotensin-converting enzyme inhibition in diabetic apolipoprotein E-deficient mice. Circulation 106:246–253
Napoli C, Bruzzese G, Ignarro LJ et al (2008) Long-term treatment with sulfhydryl angiotensin-converting enzyme inhibition reduces carotid intima-media thickening and improbe the nitric oxide/oxidative stress pathways in newly diagnosed patients with mild to moderate primary hypertension. Am Heart J 156:1154–1162
Napoli C, Lerman LO, de Nigris F, Gossl M, Balestrieri ML, Lerman A (2006) Rethinking primary prevention of atherosclerosis-related diseases. Circulation 114:2517–2527
Napoli C, Liguori A, Sorice P et al (1996) Relations between vasoactive hormones and diastolic function in hypertensive uraemic patients. J Intern Med 240:389–394
Persson J, Stavenow L, Wikstrand J, Israelsson B, Formgren J, Berglund G (1992) Noninvasive quantification of atherosclerotic lesions. Reproducibility of ultrasonographic measurement of arterial wall thickness and plaque size. Arterioscler Thromb 12:261–266
Napoli C, Sica V, de Nigris F et al (2004) Sulfhydryl angiotensin-converting enzyme inhibition induces sustained reduction of systemic oxidative stress and improves the nitric oxide pathway in patients with essential hypertension. Am Heart J 148:e5–e13
Casamassimi A, Balestrieri ML, Fiorito C et al (2007) Comparison between total endothelial progenitor cell isolation versus enriched Cd133+ culture. J Biochem 141:503–511
Williams RL (2000) A note on robust variance estimation for cluster-correlated data. Biometrics 56:645–646
Keymel S, Kalka C, Rassaf T, Yeghiazarians Y, Kelm M, Heiss C (2008) Impaired endothelial progenitor cell function predicts age-dependent carotid intimal thickening. Basic Res Cardiol 103:582–586
Lau KK, Chan YH, Yiu KH et al (2007) Burden of carotid atherosclerosis in patients with stroke: relationships with circulating endothelial progenitor cells and hypertension. J Hum Hypertens 21:445–451
Porto I, Di Vito L, De Maria GL et al (2009) Comparison of the effects of ramipril versus telmisartan on high-sensitivity C-reactive protein and endothelial progenitor cells after acute coronary syndrome. Am J Cardiol 103:1500–1505
Kowala MC, Grove RI, Aberg G (1994) Inhibitors of angiotensin converting enzyme decrease early atherosclerosis in hyperlipidemic hamsters. Fosinopril reduces plasma cholesterol and captopril inhibits macrophage-foam cell accumulation independently of blood pressure and plasma lipids. Atherosclerosis 108:61–72
Unger T (2002) The role of the renin-angiotensin system in the development of cardiovascular disease. Am J Cardiol 89:3A–10A
Jacoby DS, Rader DJ (2003) Renin-angiotensin system and atherothrombotic disease: from genes to treatment. Arch Intern Med 163:1155–1164
Scribner AW, Loscalzo J, Napoli C (2003) The effect of angiotensin converting enzyme inhibition on endothelial function and oxidant stress. Eur J Pharmacol 482:95–99
de Nigris F, D'Armiento FP, Somma P et al (2001) Chronic treatment with sulfhydryl angiotensin-converting enzyme inhibitors reduce susceptibility of plasma LDL to in vitro oxidation, formation of oxidation-specific epitopes in the arterial wall, and atherogenesis in apolipoprotein E knockout mice. Int J Cardiol 81:107–115
Evangelista S, Manzini S (2005) Antioxidant and cardioprotective properties of the sulphydryl angiotensin-converting enzyme inhibitor zofenopril. J Int Med Res 33:42–54
Cominacini L, Pasini A, Garbin U et al (2002) Zofenopril inhibits the expression of adhesion molecules on endothelial cells by reducing reactive oxygen species. Am J Hypertens 15:891–895
António N, Fernandes R, Rodriguez-Losada N et al (2010) Stimulation of endothelial progenitor cells: a new putative effect of several cardiovascular drugs. Eur J Clin Pharmacol 66:219–230
Acknowledgments
This work was supported in part by grants from the Progetto di Rilevante Interesse Nazionale Ministero Italiano Università e Ricerca 2006 [Code 0622153_002 “Meccanismi fisiopatologici di danno vascolare/trombotico ed angiogenesi” (to CN), Ricerca Finalizzata del Ministero della Salute 2007 (to FC), and the Fondation Jerome Lejeune, France (to CN)
Author contributions
Dr. Cacciatore, Dr. Vitale, and Prof. Napoli played a major role in the writing of the manuscript. Dr. Cacciatore and Dr. Vitale were also responsible for statistical analysis. Dr. Liguori, and Dr. Bruzzese had the overall responsibility for all in-hospital activities, in particular, coordination of the clinical team, permissions to access medical records, obtaining informed consent, and clinical protocols. Dr. de Nigris, Dr. Fiorito, Dr. Infante, and Dr. Minucci provided execution and interpretation of clinical laboratory measurements. Prof. Napoli and Prof. Ignarro were involved in the first series of studies addressing the vascular effects of ACE inhibitors, thus providing the rationale and aim of the study. However, strong support on the detailed design of the study and its follow-up was given by Prof. Donatelli, Dr. Liguori, and Dr. Cacciatore.
Conflict of Interest
None of the authors have a conflict of interest in connection with this study
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cacciatore, F., Bruzzese, G., Vitale, D.F. et al. Effects of ACE inhibition on circulating endothelial progenitor cells, vascular damage, and oxidative stress in hypertensive patients. Eur J Clin Pharmacol 67, 877–883 (2011). https://doi.org/10.1007/s00228-011-1029-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-011-1029-0