Abstract
Purpose
To compare family paediatricians’ and general practitioners’ habits on drug prescribing to children.
Methods
Prescriptions reimbursed by the Health Service and dispensed by the retail pharmacies of 15 local health units in the Lombardy Region of Italy during 2005 were analysed. Only family paediatricians and general practitioners who were in charge of children aged 6–13 years were included.
Results
During 2005, 239,296 children (43.6% of the selected population) received at least one drug prescription. The prevalence was higher in children treated by general practitioners (44.2 versus 43.4%), in particular in children 13 years old, with a prevalence of 38.7 versus 31.8% in children cared for by general practitioners and family paediatricians respectively. The prevalence of the most prescribed therapeutic classes was similar in the two groups. Some differences were found concerning the antibiotic classes, with family paediatricians prescribing penicillins more frequently and general practioners prescribing macrolides and cephalosporins more frequently. A total of 542 drugs were prescribed, 78% of which were prescribed by both the family paediatricians and the general practitioners. In all, only four drugs were prescribed by 75% or more physicians. The chance of receiving a drug prescription, adjusted for age, gender and local health unit of residence, was slightly higher in children cared for by general practitioners (OR 1.16; 95%CI 1.14–1.17).
Conclusions
Few differences were found between the prescribing patterns of family paediatricians and those of general practitioners. Differences exist in particular for older children and for some drug classes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Drug utilisation studies performed in the Italian paediatric population found a prescription profile that appears to be specific to Italy, especially concerning antibiotics [1–5]. For these drugs, both quantitative and qualitative differences with respect to other European countries were found [6]. The antibiotic prescription prevalence was three- to four-fold higher in Italy than in the Netherlands or the UK, with a wide use of second-choice antibiotics such as cephalosporins [6]. Moreover, a wide, irrational use of anti-asthmatics, in particular inhaled steroids, was observed [7].
According to some international studies, drug prescriptions are influenced by the type of physician writing them [8–13]. In fact, differences in prescription profiles between family paediatricians and general practitioners have been found, in particular concerning antibiotics [9, 10, 12, 13].
In Italy, children are assigned to a paediatrician until they are 6 years old; afterwards, the parents can choose to remain with that paediatrician until the child is 14 years old or to register the child with a general practitioner. All adolescents over 14 years of age are assigned to a general practitioner. No studies have been performed in Italy to compare the prescribing profile of the two kinds of physicians.
Thus, an analysis of drugs prescribed to children 6–13 years old was performed in order to compare general practitioners’ with family paediatricians’ prescribing profiles.
Methods
The data source was a database routinely updated for administrative and reimbursement reasons. The database stores all community (i.e., out of hospital) prescriptions issued to individuals living in the Lombardy Region which are reimbursed by the National Health Service (NHS). Data were managed and analyzed using an anonymous patient code, after obtaining each local health unit director’s authorisation.
The analysis involved all paediatric prescriptions reimbursed by the Health Service and dispensed by the retail pharmacies of all the 15 local health units (LHU) in the Lombardy Region, in northern Italy, between 1 January and 31 December 2005. In order to obtain a comparable sample, only physicians who were in charge of children representing ages in the 6–13 year old range were included. Moreover, physicians below the 5-centile according to the number of treated children were excluded. Children receiving six or more prescriptions were also excluded, since the percentage of chronically treated patients may be different between physician types and may influence the prescribing profile.
A total of 548,922 children 6–13 years of age were selected (81% of the Lombardy Region’s population of 6–13 year olds); 402,053 children were cared for by 1,020 family paediatricians (88% of the total number of family paediatricians) and 146,869 children were cared for by 2,824 general practitioners (42% of the total).
Prescribed drugs were classified according to the International Anatomical-Therapeutic-Chemical Classification system (ATC). Prevalence data by children’s age and type of physician were calculated by dividing the number of drug users by the total number of residents in each age group. Moreover, a Mantel-Haentzel χ2 test was performed in order to compare the drug prescription prevalence in children cared for by family paediatricians versus children cared for by general practitioners.
The area under the prevalence-time curve (AUC) from time 6 to 13 years (data plotted at mid-time interval) was calculated according to the linear trapezoidal rule. The slopes of the prevalence vs. time curve were estimated by log-linear least square fit of the 6 and 13 year age points. Comparisons were made using the t test. A logistic regression analysis was performed to evaluate the association between drug prescription, type and gender of physician, and the age, gender, and LHU of residence of the child. The percentage of family paediatricians and general practitioners who prescribed each drug was calculated, and a percentage ≥75% was considered a high degree of concordance. Statistical analysis was performed using SAS software, version 9.1. A P value < 0.05 was considered statistically significant.
Results
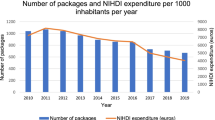
During 2005, 239,296 children (43.6% of the population) received at least one drug prescription (Table 1). The prevalence was highest at 6 years of age (53.9%) and decreased to 35% in children 13 years old (Fig. 1).
The prevalence was slightly higher in children treated by general practitioners (44.2 versus 43.4%; χ2 M-H = 845, P < 0.001). The greatest difference was observed in 13-year-old children, with a prevalence of 38.7 versus 31.8% in children cared for by general practitioners and family paediatricians respectively. A difference was found when comparing the slopes of the prevalence versus age curve (P < 0.001).
The AUC6–14 prevalence ratio for general practitioners/paediatricians was 1.1.
The chance, adjusted for age, gender, and LHU of residence, of receiving a drug prescription was slightly higher in children cared for by general practitioners (OR 1.16; 95%CI 1.14–1.17). Moreover, the chance was slightly higher for children in the charge of female compared to male physicians (OR 1.08; 95%CI 1.07–1.10).
On average, each treated child received two prescriptions, without differences between the two physician type groups, while the mean number of medication packages prescribed to children cared for by family paediatricians was slightly higher (2.9 versus 2.6).
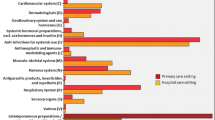
Antibiotics, anti-asthmatics, and antihistamines were the most prescribed therapeutic classes and covered 92.5% of the packages. The prevalence of antibiotics was nearly the same in the two groups (37%), while the prevalence of anti-asthmatics was slightly higher in children treated by family paediatricians (10.6 vs 9.9%) and, in contrast, the prevalence of antihistamines was higher in the general practitioner–treated group (4.2 vs 3.6%).
Taking into account the ten most prescribed classes, the prevalence of antinflammatory and antirheumatic drugs was 5-fold higher and the prevalence of intestinal antidiarrheals/antinfectives was 3.5-fold higher in children treated by general practitioners. In contrast, the prevalence rates of antiparasitic drugs and antivirals were 1.4 fold higher in the paediatrician treated–group.
An analysis of antibiotic prescriptions by class was also performed. The prevalence of penicillins was higher in children cared for by family paediatricians (64.5 vs 54.2%), while the prevalence of macrolides and cephalosporins was higher in children cared for by general practitioners (32.9 vs 28.3%, and 32.2 vs 26.6% respectively).
Amoxicillin + clavulanic acid was the most frequently prescribed drug independently of the type of physician, followed by amoxicillin and beclometasone. Fourteen out of the 15 most frequently prescribed drugs were the same in both groups (Table 2).
Budesonide was among the most prescribed drugs only in the family paediatrician–treated group and oxatomide only in the general practitioner group.
A total of 542 drugs were prescribed, 78% of which were prescribed by both the family paediatricians and the general practitioners. Of these, 74 drugs (14%) were prescribed only by the family paediatricians and 42 (8%) only by the general practitioners. In particular, 7/74 and 4/42 were sexual hormones (mainly oral contraceptives). Furthermore, 48 out of 74 (64%) and 36 out of 42 (86%) drugs were prescribed by only one physician to one child.
In all, 96% of the drugs were prescribed by less than 25% of the physicians, with a higher percentage among general practitioners compared to family paediatricians (97 versus 92% respectively; χ2 = 11, P < 0.001). In all, 13 drugs were prescribed by 75% or more of family paediatricians, and only 4 drugs were prescribed by 75% or more of general practitioners (Table 2).
The drug with the highest degree of concordance was amoxicillin + clavulanic acid, prescribed by more than 96% of family paediatricians and general practitioners. The other common drugs were amoxicillin, beclometasone and clarithromycin. These four drugs covered 68% of the treated children and the 54% of the packages. A total of 91 pharmaceutical preparations (identified by trade name, strength and formulation) containing the four leading drugs were prescribed, 87 of which (96%) were shared by family paediatricians and general practitioners.
Only two pharmaceutical preparations were prescribed by 75% or more family paediatricians and general practitioners: Augmentin (amoxicillin + clavulanic acid) 400/57 mg dry powder for oral suspension and Clenil (beclometasone) 0.8 mg/2 ml nebulised suspension. No pharmaceutical preparation of amoxicillin or clarithromycin was prescribed by more than 50% of the general practitioners (Table 3).
Among physicians prescribing amoxicillin, 91% of family paediatricians and 44% of the general practitioners prescribed a generic version (χ2 = 504; P < 0.001). The percentage of children receiving generic amoxicillin was 41% in those cared for by family paediatricians and 22% in those cared for by general practitioners (χ2 = 1,525; P < 0.001).
Discussion
The prevalence of drug prescriptions was slightly higher, with an OR of 1.2, in children treated by general practitioners. In contrast, children cared for by paediatricians received a greater number of packages. Despite these differences, the prescription profiles of general practitioners and family paediatricians were similar. Only a few differences were found concerning the most prescribed therapeutic classes, as expected since the two types of physicians face the same diseases. However, the differences were greater for some classes with a low prevalence rate, e.g. the prevalence of antinflammatory drugs was five-fold higher in children treated by general practitioners, even if the most frequently prescribed drugs were the same in both groups (ketoprofen, nimesulide, acetylsalicylic acid).
A large number of drugs were prescribed, and most of them were prescribed by both family paediatricians and general practitioners. Only a few drugs were specific to a physician type, and nearly all of these were prescribed by one physician to one child.
It is interesting to note that while 13 drugs were prescribed by 75% or more family paediatricians, only 4 drugs were prescribed by 75% or more general practitioners. A wide variability in the drugs was observed for both groups of physicians, even if a greater percentage of drugs prescribed by less than 25% of the physicians was found for general practitioners (97 versus 92%). A lower concordance was, therefore, observed among general practitioners, and very few drugs can be considered “essential” on the basis of their prescribing attitude.
It is likely that this finding is influenced by the fact that general practitioners are in charge of fewer children compared to family paediatricians and that each general practitioner has to therefore deal with a narrower spectrum of diseases and therapeutic needs.
A low level of agreement emerged also when looking at the pharmaceutical preparations of the four drugs with a high degree of concordance among prescribers: 11 preparations were prescribed by 75% or more of family paediatricians and only 2 by 75% or more of general practitioners. In the case of amoxicillin and clarithromycin, there were no pharmaceutical preparations prescribed by more than 50% of the general practitioners. However, this could indicate that many general practitioners prefer to prescribe only one trade name, while family paediatricians more commonly prescribe different trade names of the same drug. This was the case for clarithromycin, for which three different trade name oral suspensions were prescribed by more than 75% of family paediatricians.
General practitioners seem to have less of a tendency to prescribe generic drugs, at least taking into account amoxicillin prescriptions. In fact, nearly six out of ten general practitioners never prescribed generic amoxicillin, and children cared for by general practitioners had a 50% lower chance of receiving generic amoxicillin compared to children cared for by family paediatricians.
The prescribing profile observed in this setting did not differ from that of other Italian contexts, in particular concerning the antibiotic prescription profile, which was characterised by a wide use of second-line agents (cephalosporins or macrolides). In this, Italy differs from other European countries [6].
A more common inappropriate use of antibiotics has been observed among general practitioners than family paediatricians in three international studies [10, 12, 13]. In this study, no differences were observed regarding antibiotic prevalence rate; however, differences were found concerning antibiotic classes, with the family paediatricians prescribing penicillins more commonly and general practictioners prescribing macrolides and cephalosporins more frequently. This finding partly reflects the profile observed in the Italian adult population [14]. Amoxi-clavulanic acid was the most prescribed antibiotic, and it was prescribed by more than 96% of physicians, despite the fact that amoxicillin is considered the antibiotic of choice for the most common infections in the paediatric age group [15–17] and is the most prescribed antibiotic in other countries [6]. Moreover, nearly one out of ten general practitioners had never prescribed amoxicillin.
In Italy, amoxicillin + clavulanic acid was probably preferred due to its twice-daily schedule regimen, which is supposed to yield a better compliance compared to the amoxicillin dosage schedule, and to an unproved concern of beta-lactamase-producing bacteria. This study therefore seems to confirm that different attitudes towards antibiotic prescribing exist between family paediatricians and general practitioners.
However, taking into account other drug classes, family paediatricians and general practitioners seem to share the same inappropriate prescriptions. In this regard, it is interesting to note that the prevalence of nebulised beclometasone, commonly prescribed without evidence of efficacy for the symptomatic treatment of upper respiratory tract infections (e.g. common cold, pharyngitis), as previously reported in a study performed with a group of Italian family paediatricians [18], was the same in the two groups.
The main limitation of this study is that only drugs reimbursed by the National Health Service were evaluated. It is therefore possible that there are some differences in the prescribing profile of drugs that are not reimbursed or that are over-the-counter (e.g., analgesics, antitussive medicines and prokinetics). Moreover, this study was performed in a very homogeneous regional setting and the findings may not perfectly reflect the national situation. However, the study sample represents 12% of the 6- to 13-year-old Italian population, and the profile of drug prescriptions is similar to that observed in other national settings.
The findings from this study seem to document that there are few differences in the prescribing pattern between general practitioners and family paediatricians. Differences exist in particular for older children and for some drug classes. The inappropriateness of drug prescription to children is mostly independent of the type of physician. This should be taken into account in planning and performing educational interventions with the aim of improving the rational use of drugs in children. Such interventions should involve all health care professionals and not only family paediatricians.
References
Cazzato T, Pandolfini C, Campi R, Bonati M, The ACP Puglia-Basilicata Working Group (2001) Drug prescribing in out-patient children in southern Italy. Eur J Clin Pharmacol 57:611–616
Clavenna A, Berti A, Gualandi L, Rossi E, De Rosa M, Bonati M (2009) Drug utilisation profile in the Italian paediatric population. Eur J Pediatr 168:173–180
Borgnolo G, Simon G, Francescutti C, Lattuada L, Zanier L (2001) Antibiotic prescription in Italian children: a population-based study in Friuli Venezia Giulia, north-east Italy. Acta Paediatr 90:1316–1320
Resi D, Milandri M (2003) Antibiotic prescriptions in children. J Antimicrob Chemother 52:282–286
Gagliotti C, Morsillo F, Resi D, Milandri M, Moro ML (2005) A three-year population-based study of antibiotic treatments for children. Acta Paediatr 94:1502–1504
Rossignoli A, Clavenna A, Bonati M (2007) Antibiotic prescription and prevalence rate in the outpatient paediatric population: analysis of surveys published during 2000–2005. Eur J Clin Pharmacol 63:1099–1106
Clavenna A, Rossi E, Berti A et al (2003) Inappropriate use of anti-asthmatic drugs in the Italian paediatric population. Eur J Clin Pharmacol 59:565–569
Sun HL, Kao YH, Chou MC, Lu TH, Lue KH (2006) Differences in the prescription patterns of anti-asthmatic medications for children by paediatricians, family physicians and physicians of other specialties. J Formos Med Assoc 105:277–283
Akici A, Kalaca S, Ugurlu MU, Oktay S (2004) Prescribing habits of general practitioners in the treatment of childhood respiratory-tract infections. Eur J Clin Pharmacol 60:211–216
Quach C, Collet JP, LeLorier J (2004) Acute otitis media in children: a retrospective analysis of physician prescribing patterns. Br J Clin Pharmacol 57:500–505
Rushton JL, Clark SJ, Freed GL (2000) Paediatrician and family physician prescription of selective serotonin reuptake inhibitors. Pediatrics 105:E82
Pradier C, Rotily M, Cavailler et al (1999) Factors related to the prescription of antibiotics for young children with viral pharyngitis by general practitioners and family paediatricians in southeastern France. Eur J Clin Microbiol Infect Dis 18:510–514
Bocquet A, Chalumeau M, Bollotte D, Escano G, Langue J, Virey B (2005) Comparison of prescriptions by paediatricians and general practitioners: a population-based study in Franche-Comté from the database of Regional Health Insurance Fund. Arch Pediatr 12:1688–1696
Mazzaglia G, Caputi AP, Rossi A et al (2003) Exploring patient- and doctor-related variables associated with antibiotic prescribing for respiratory infections in primary care. Eur J Clin Pharmacol 59:651–657
Scottish Intercollegiate Guidelines Network (SIGN) (2003) Diagnosis and management of childhood otitis media in primary care. A national clinical guideline. SIGN, Edinburgh
American Academy of Pediatrics Subcommittee on Management of Acute Otitis Media (2004) Diagnosis and management of acute otitis media. Pediatrics 113:1451–1465
Scottish Intercollegiate Guidelines Network (SIGN) (1999) Management of sore throat and indication for tonsillectomy. A national clinical guideline. SIGN, Edinburgh
Pandolfini C, Campi R, Clavenna A, Cazzato T, Bonati M (2005) Italian family paediatricians and off-label prescriptions: loyal to regulatory or guideline standards. Acta Paediatr 94:753–757
Acknowledgements
Antonio Clavenna holds an educational fellowship granted by Boehringer Ingelheim Italia. The authors would like to acknowledge Dr Angela Bortolotti, Dr Luca Merlino and Dr Ida Fortino, of the Regional Health Ministry - Lombardy Region, Milan, for providing data. This study has been funded in part by the Lombardy Region Health Ministry (Progetto “Epidemiologia dei farmaci - EPIFARM”)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Clavenna, A., Sequi, M. & Bonati, M. Differences in the drug prescriptions to children by Italian paediatricians and general practitioners. Eur J Clin Pharmacol 66, 519–524 (2010). https://doi.org/10.1007/s00228-010-0786-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-010-0786-5