Abstract
Objective
In vitro work has demonstrated that cinacalcet is a strong inhibitor of cytochrome P450 isoenzyme (CYP) 2D6. The purpose of this study was to evaluate the effect of cinacalcet on CYP2D6 activity, using desipramine as a probe substrate, in healthy subjects.
Methods
Seventeen subjects who were genotyped as CYP2D6 extensive metabolizers were enrolled in this randomized, open-label, crossover study to receive a single oral dose of desipramine (50 mg) on two separate occasions, once alone and once after multiple doses of cinacalcet (90 mg for 7 days). Blood samples were obtained predose and up to 72 h postdose.
Results
Fourteen subjects completed both treatment arms. Relative to desipramine alone, mean AUC and Cmax of desipramine increased 3.6- and 1.8-fold when coadministered with cinacalcet. The t 1/2,z of desipramine was longer when desipramine was coadministered with cinacalcet (21.0 versus 43.3 hs). The t max was similar between the regimens. Fewer subjects reported adverse events following treatment with desipramine alone than when receiving desipramine with cinacalcet (33 versus 86%), the most frequent of which (nausea and headache) have been reported for patients treated with either desipramine or cinacalcet.
Conclusion
This study demonstrates that cinacalcet is a strong inhibitor of CYP2D6. These data suggest that during concomitant treatment with cinacalcet, dose adjustment may be necessary for drugs that demonstrate a narrow therapeutic index and are metabolized by CYP2D6.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The calcimimetic cinacalcet hydrochloride (Sensipar®/Mimpara®) increases the sensitivity of the calcium-sensing receptor to activation by extracellular calcium, thereby reducing parathyroid hormone, serum calcium, and phosphorus levels in patients with secondary hyperparathyroidism (HPT) [1] and serum calcium levels in patients with primary HPT [2, 3] or parathyroid carcinoma [4]. An in vitro study has demonstrated that cinacalcet is a strong inhibitor of cytochrome P450 isoenzyme (CYP) 2D6 [50% inhibitory concentration (IC50) <0.1 μM] [5]. A multitude of drugs from different therapeutic categories are metabolized by CYP2D6, including antifungal agents, β-adrenergic blockers, antiarrhythmic agents, serotonin reuptake inhibitors (SSRI), tricyclic antidepressants (TCA), antipsychotics, and opioids [6]. Deleterious clinical effects of coadministration of a CYP2D6 substrate and inhibitor have been documented in case reports [7–9], and the potential for such interactions has been suggested and documented in clinical studies [10–12].
Desipramine hydrochloride, a commonly used TCA, is metabolized into 2-hydroxydesipramine almost exclusively by CYP2D6, making it a sensitive and selective probe substrate for CYP2D6 inhibition. Increased exposure of desipramine has been documented following coadministration with CYP2D6 inhibitors such as sertraline [10], deramciclane [13], duloxetine [14], paroxetine [10, 13, 15], fluoxetine [16], and terbinafine [11] and in individuals who are genetically deficient in CYP2D6 (poor metabolizers) [17].
To assess the potential for drug interactions involving CYP2D6 substrates following cinacalcet therapy, this study evaluated the effect of cinacalcet on the pharmacokinetics of a prototypical CYP2D6 substrate, desipramine.
Methods
Study design
This phase 1, randomized, open-label, single-center, two-treatment, two-period, two-sequence crossover study enrolled 17 healthy subjects between the ages of 18 and 55 years. The study was conducted in accordance with Good Clinical Practice guidelines, with Institutional Review Board approval, and written informed consent by all subjects prior to study participation.
Subjects were required to be CYP2D6 extensive metabolizers (determined by genotyping) (Genaissance Pharmaceuticals, New Haven, CT, USA), to have normal clinical laboratory tests (complete blood count, blood chemistries), a normal physical exam and electrocardiogram (ECG), and a negative urine alcohol and drug screen. Subjects were ineligible if they had a history or evidence of a clinically significant medical disease or condition (e.g., seizure disorder, cardiac arrhythmia), drug or alcohol abuse, hepatitis B surface antigens, or hepatitis C or human immunodeficiency virus antibodies. Subjects were excluded for tobacco use or participation in another investigational study within 30 days, or medication use, including over-the-counter (with exception of acetaminophen) or herbal products within 14 days before dosing. All of the aforesaid medications were prohibited during the study unless approved by the investigator. Subjects were also excluded if they were unwilling to use adequate contraception (women only), were pregnant or lactating, or for any other condition that would impede the study.
Treatment procedures
Subjects were randomized in a 1:1 ratio to receive a single 50 mg dose of desipramine alone (treatment A) or during a 7-day course of cinacalcet 90 mg (treatment B) in the first period based on a computer-generated randomization schedule prepared at Amgen, Inc. using SAS. After a washout period of at least 10 days subjects received the other treatment during period 2. For treatment A, subjects were administered a single oral dose of desipramine on day 1 following a 10-h fast. For treatment B, subjects received cinacalcet on days 1, 2, 3, 4, 6, and 7 with breakfast, and with desipramine on the morning of day 5 following a 10-h fast. Subjects remained in the research facility through day 2 for treatment A (with outpatient visits on days 3 and 4), and through the morning of day 8 for treatment B.
On day 1 of treatment A and day 5 of treatment B, blood samples for determination of plasma desipramine concentrations were collected into sodium heparinized tubes predose and 1, 2, 4, 6, 8, 10, 12, 24, 48, and 72 h postdose. Physical exams and ECGs were conducted and blood samples for complete blood count and blood chemistries were collected at screening and at the conclusion of the study. Vital signs and adverse event reporting were conducted daily during the treatment periods.
Pharmacokinetics
Plasma concentrations of desipramine were determined by liquid chromatography coupled with tandem mass spectrometry (LC-MS/MS), with a lower limit of quantitation (LOQ) of 0.500 ng/ml (MDS Pharma Services, Lincoln, NE, USA). Desipramine plasma concentration-time data were analyzed by noncompartmental methods using WinNonlin Professional v. 3.3 (Pharsight Corporation, Mountain View, CA, USA) and were plotted on a semi-log scale. The data points that described the log-linear terminal phase were identified. The terminal phase rate constant, λz, was estimated using a linear regression of the log-transformed terminal data points versus time, and terminal half-life (t 1/2,z) was calculated as 0.693/λz. The area under the concentration-time curve from 0 to the time of the last measurable concentration (AUC0−t) was calculated by the linear trapezoidal rule. The area under the concentration-time curve from the time of the last measurable concentration to infinity (\({\text{AUC}}_{{{\text{t}} - \infty }}\)) was calculated by dividing the concentration for the last measurable plasma concentration by λz. \({\text{AUC}}_{{0 - \infty }}\) was calculated by the summation of AUC0−t and \({\text{AUC}}_{{{\text{t}} - \infty }}\). Oral clearance (CL/F) was calculated as dose/\({\text{AUC}}_{{0 - \infty }}\).
Concentration values for desipramine below the LOQ were set to zero for all calculations. Concentration data and pharmacokinetic parameters were summarized using descriptive statistics. AUC and Cmax were analyzed using a crossover analysis of variance (ANOVA) model. The subject, subject within sequence, period, and treatment effects were extracted. AUC and Cmax were transformed to natural logarithms before analysis. All other summary statistics were based on original scale data. For AUC and Cmax, point estimates and 90% confidence intervals (CI) were constructed for the ratio of desipramine with cinacalcet to desipramine alone using the residual variance from the ANOVA and were expressed as a percentage. Absence of an interaction was to be concluded if the 90% CIs were between 0.8 and 1.25.
Safety
The safety profile was characterized using adverse events, vital signs, clinical laboratory measurements, ECGs, and physical examinations for subjects who received at least one dose of either study drug. Adverse events were summarized by frequency and type for each group (i.e., desipramine alone or desipramine with cinacalcet).
Results
Subjects
Seventeen subjects were enrolled, with 15 (8 women, 7 men) completing at least one treatment period. Of these 15, 9 (60%) were white, 2 (13%) were black, and 4 (27%) were of other races. Subjects had a mean±SD age of 31.5±10.8 years, and a body mass index of 24.6±3.19 kg/m2. Two subjects were deemed ineligible due to a positive urine alcohol screen before the first dose, and one subject withdrew consent during the study. All 15 treated subjects were included in the safety analyses, and the 14 subjects who completed both treatment periods were included in the pharmacokinetics analyses.
Pharmacokinetics
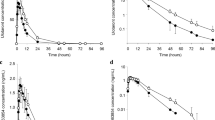
Relative to when desipramine was administered alone, a 3.6-fold increase in \({\text{AUC}}_{{0 - \infty }}\) and 1.8-fold increase in Cmax of desipramine was observed when cinacalcet was administered for 5 days before and 2 days after dosing with desipramine (Table 1, Fig. 1). Administration with cinacalcet resulted in an increase in the \({\text{AUC}}_{{0 - \infty }}\) and Cmax of desipramine for all subjects (Fig. 2). Coadministration of desipramine and cinacalcet also resulted in a notable reduction in desipramine oral clearance. The terminal half-life of desipramine was also increased by approximately twofold when desipramine was coadministered with cinacalcet. The median t max was 6 h following administration of desipramine alone and following administration with cinacalcet.
Safety
Overall, treatment-related adverse events (as determined by the investigator) occurred in 33% (5/15) of the subjects during the desipramine alone period and 86% (12/14) during the desipramine with cinacalcet period. The most common treatment-related adverse events (>1 in either group) are reported in Table 2.
All adverse events were mild to moderate in severity. There were no clinically significant changes in laboratory results, vital signs, or ECGs over the course of the study. No deaths occurred during the study and no subjects withdrew due to adverse events.
Discussion
Coadministration of cinacalcet (90 mg once daily for 7 days) and a single oral dose desipramine 50 mg on day 5 resulted in a 3.6-fold and 1.8-fold increase in the AUC and Cmax, respectively, of desipramine, a CYP2D6 substrate. The terminal half-life of desipramine was significantly prolonged, and clearance was correspondingly reduced when cinacalcet was coadministered. These in vivo findings are consistent with in vitro data which demonstrated that cinacalcet is a strong inhibitor of CYP2D6 [18]. The approximate threefold increase in desipramine exposure observed in this study was slightly less than the largest (approximately fourfold to fivefold) increases in AUC observed in studies of coadministration of desipramine with other known strong CYP2D6 inhibitors: paroxetine [10, 13], fluoxetine [16], and terbinafine [11]. Assuming that these other CYP2D6 inhibitors completely abolish CYP2D6 activity, the 3.6-fold increase in desipramine AUC resulting from coadministration of cinacalcet corresponds to an approximately 90% inhibition of CYP2D6 activity. Presumably, higher doses of cinacalcet could result in even greater inhibition, and therefore, cinacalcet should be classified as a strong inhibitor of CYP2D6.
An increased incidence of adverse events was observed during coadministration of desipramine and cinacalcet compared with administration of desipramine alone. Although this study was not designed to draw a definitive link between either agent and a particular adverse event, some associations based on previous findings can be made. Paresthesia is a known adverse effect of desipramine, and increased exposure of desipramine may increase the probability of subjects experiencing this side effect. Conversely, nausea is among the most commonly reported adverse events in clinical studies of cinacalcet [1, 19, 20] and is, therefore, not necessarily the result of CYP2D6 inhibition.
Deleterious clinical effects have been reported following coadministration of TCAs and CYP2D6 inhibitors [7–9]. In this study, an increase in the number of treatment-related adverse events was observed during the desipramine with cinacalcet treatment arm in relation to the desipramine alone arm, the most frequent of which (nausea and headache) have been reported for patients treated with either desipramine or cinacalcet.
In conclusion, these in vivo findings confirm the in vitro findings that cinacalcet is a strong CYP2D6 inhibitor. Coadministration of desipramine with cinacalcet resulted in a significant increase in exposure to desipramine. Therefore, caution should be undertaken when cinacalcet is coadministered with known CYP2D6 substrates that have narrow therapeutic windows.
References
Block GA, Martin KJ, de Francisco AL, Turner SA, Avram MM, Suranyi MG et al (2004) Cinacalcet for secondary hyperparathyroidism in patients receiving hemodialysis. N Engl J Med 350(15):1516–1525
Peacock M, Bilezikian JP, Klassen PS, Guo MD, Turner SA, Shoback D (2005) Cinacalcet hydrochloride maintains long-term normocalcemia in patients with primary hyperparathyroidism. J Clin Endocrinol Metab 90(1):135–141
Shoback DM, Bilezikian JP, Turner SA, McCary LC, Guo MD, Peacock M (2003) The calcimimetic cinacalcet normalizes serum calcium in subjects with primary hyperparathyroidism. J Clin Endocrinol Metab 88(12):5644–5649
Silverberg SJ, Faiman C, Bilezikian JP, Shoback D, Rubin MR, Smallridge R et al (2004) Cinacalcet HCl effectively treats hypercalcemia in patients with parathyroid carcinoma. J Bone Miner Res 19(S1):S103
Bajpai M, Esmay J, Chi V, Hayashi M, Poppe L, Kumar G (2005) In vitro metabolism and prediction of drug-drug interactions of the calcimimetic agent cinacalcet HCl. Drug Metab Rev 37(Suppl 2):124
Venkatakrishnan K, von Moltke LL, Greenblatt DJ (2000) Effects of the antifungal agents on oxidative drug metabolism: clinical relevance. Clin Pharmacokinet 38(2):111–180
Preskorn SH, Beber JH, Faul JC, Hirschfeld RM (1990) Serious adverse effects of combining fluoxetine and tricyclic antidepressants. Am J Psychiatry 147(4):532
Bell IR, Cole JO (1988) Fluoxetine induces elevation of desipramine level and exacerbation of geriatric nonpsychotic depression. J Clin Psychopharmacol 8(6):447–448
Westermeyer J (1991) Fluoxetine-induced tricyclic toxicity: extent and duration. J Clin Pharmacol 31(4):388–392
Alderman J, Preskorn SH, Greenblatt DJ, Harrison W, Penenberg D, Allison J et al (1997) Desipramine pharmacokinetics when coadministered with paroxetine or sertraline in extensive metabolizers. J Clin Psychopharmacol 17(4):284–291
Madani S, Barilla D, Cramer J, Wang Y, Paul C (2002) Effect of terbinafine on the pharmacokinetics and pharmacodynamics of desipramine in healthy volunteers identified as cytochrome P450 2D6 (CYP2D6) extensive metabolizers. J Clin Pharmacol 42(11):1211–1218
Hamelin BA, Bouayad A, Methot J, Jobin J, Desgagnes P, Poirier P et al (2000) Significant interaction between the nonprescription antihistamine diphenhydramine and the CYP2D6 substrate metoprolol in healthy men with high or low CYP2D6 activity. Clin Pharmacol Ther 67(5):466–477
Laine K, De Bruyn S, Bjorklund H, Rouru J, Hanninen J, Scheinin H et al (2004) Effect of the novel anxiolytic drug deramciclane on cytochrome P(450) 2D6 activity as measured by desipramine pharmacokinetics. Eur J Clin Pharmacol 59(12):893–898
Skinner MH, Kuan HY, Pan A, Sathirakul K, Knadler MP, Gonzales CR et al (2003) Duloxetine is both an inhibitor and a substrate of cytochrome P4502D6 in healthy volunteers. Clin Pharmacol Ther 73(3):170–177
Brøsen K, Hansen JG, Nielsen KK, Sindrup SH, Gram LF (1993) Inhibition by paroxetine of desipramine metabolism in extensive but not in poor metabolizers of sparteine. Eur J Clin Pharmacol 44(4):349–355
Preskorn SH, Alderman J, Chung M, Harrison W, Messig M, Harris S (1994) Pharmacokinetics of desipramine coadministered with sertraline or fluoxetine. J Clin Psychopharmacol 14(2):90–98
Spina E, Gitto C, Avenoso A, Campo GM, Caputi AP, Perucca E (1997) Relationship between plasma desipramine levels, CYP2D6 phenotype and clinical response to desipramine: a prospective study. Eur J Clin Pharmacol 51(5):395–398
Amgen Inc. (2004) Sensipar (cinacalcet HCl) prescribing information. Retrieved 11 January 2006 from http://www.sensipar.com/prescribingInfo.jsp
Lindberg JS, Culleton B, Wong G, Borah MF, Clark RV, Shapiro WB et al (2005) Cinacalcet HCl, an oral calcimimetic agent for the treatment of secondary hyperparathyroidism in hemodialysis and peritoneal dialysis: a randomized, double-blind, multicenter study. J Am Soc Nephrol 16(3):800–807
Charytan C, Coburn JW, Chonchol M, Herman J, Lien YH, Liu W et al (2005) Cinacalcet hydrochloride is an effective treatment for secondary hyperparathyroidism in patients with CKD not receiving dialysis. Am J Kidney Dis 46(1):58–67
Acknowledgements
Amgen, Inc. supported this study (Study 20040151). The study was conducted at PPD Development, LP, Austin, Texas. Drs. Padhi, Posvar, and Harris and Ms. Salfi are employees and stockholders of Amgen, Inc. Dr. William Stark, an employee and stockholder of Amgen, Inc., contributed to the writing of this manuscript. This study complied with Good Clinical Practice guidelines and ethics regulations put forth by the United States of America.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Harris, R.Z., Salfi, M., Posvar, E. et al. Pharmacokinetics of desipramine HCl when administered with cinacalcet HCl. Eur J Clin Pharmacol 63, 159–163 (2007). https://doi.org/10.1007/s00228-006-0129-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-006-0129-8