Abstract
Objective
To determine the effect of both growth hormone deficiency (GHD) and rhGH replacement therapy on CYP3A activity as well as the potential influence of gender.
Methods
The sample consisted of 35 GHD children (16 males and 19 females), aged 2.9–13.1 years, and a control group of 35 healthy children matched for age and sex. The urinary ratio 6β-hydroxycortisol/free cortisol was used as a marker of CYP3A activity. In patients, urine samples were collected at two times, prior to starting rhGH replacement treatment and 30 days after beginning therapy.
Results
A significantly higher metabolic activity in GHD children was observed in relation to controls (P=0.0001) without sex differences. Paired comparisons demonstrated a sexually dimorphic effect of rhGH therapy on the CYP3A activity. While boys displayed a significant decrease (P=0.003), girls showed no significantly different values of CYP3A marker (P>0.05). Unpaired comparison between controls and GHD children after therapy demonstrated absence of significant differences in boys (P>0.05) and a strikingly higher activity in girls (P=0.0001).
Conclusions
The data suggests that: (a) GHD in children increases CYP3A activity in a non-sex-dependent manner, (b) rhGH treatment for 30 days to GHD children results in a sexually dimorphic effect on CYP3A activity, with a significant decrease in males toward normalization in relation to controls and non-significant changes in females. The results of this study may have important clinical implications for GHD children, since changes in CYP3A activity importantly affect the metabolism of both steroid hormones and CYP3A substrate drugs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
CYP3A is the predominant constitutive hepatic cytochrome P 450 (CYP) in humans and is responsible for approximately 60% of the total drug oxidations [1]. Hydroxylations of endogenous steroids, such as testosterone and estradiol, are catalyzed by CYP3A [2]. Bioactivation of genotoxicants aflatoxin-B1 [3] and heterocyclic amines [4] is also produced by this P 450 isoform. CYP3A activity is characterized by its inter-individual variability, which importantly accounts for the variable pharmacokinetics of its substrates [5]. Changes in activity of this cytochrome, produced by inducers or inhibitors, are known to cause important clinical consequences in terms of either efficacy or toxicity [6, 7].
Growth hormone (GH) is recognized to be the main determinant of the expression and regulation of CYPs in the liver of rodents [8], and the importance of transcription factors related to tissue-specific gene expression has been emphasized [9]. Sex differences in CYP expression in rodents are dependent on the sexual dimorphism in the secretion pattern of GH [10]. While male rats present high concentration peaks in the blood, between which the baseline concentration is almost undetectable, in female rats, the peaks are lower but appear more frequently, and the baseline concentration is higher than in males [11, 12].
Recently, it has been demonstrated that pulsatile or continuous GH exposure decreases or increases, respectively, CYP3A activity [13]. There exists some information about the regulatory properties of GH on CYP enzymes in humans based on a few studies on children [14–17] and adults [18–20]. Despite the fact that sexual dimorphism in GH secretion in humans is well documented [21], gender differences in the effect of GH on CYPs have not been reported so far. In addition, the influence of GH-deficiency status on CYP activity has not been studied in humans.
The aim of the present study is to examine the separate and interactive effects of growth hormone deficiency (GHD) and rhGH replacement therapy on CYP3A activity in children, as well as to investigate the potential gender influence.
Material and methods
Subjects and study protocol
The study population consisted of 35 selective GH-deficient children with no other pituitary alteration (16 males and 19 females) aged 9.5±3.2 years, ranging from 2.9 years to 13.1 years. Physical examinations and laboratory tests confirmed that patients had no liver or kidney dysfunction. For the control group, we recruited 35 healthy children matched for age (±6 months) and sex with patients.
All controls were of normal height and weight. We confirmed that the control children were healthy on the basis of physical examination and routine laboratory tests. Both patients and controls were asked to refrain from ingesting any drugs or foods known to alter CYP3A activity 1 month prior to and during the entire study period.
The rhGH therapy for GH-deficient children was approved by the Spanish Committee for GH Treatment, on the basis of a peak GH concentration greater than 5 ng/ml with two tests: insulin and either clonidine or ornitine in children above the age of 5 years or clonidine and ornitine in children below the age of 5 years. One blood sample was obtained from each patient to measure insulin-like growth factor I (IGF-I) and IGF-binding protein 3 (IGFBP-3). Patients received once daily subcutaneous injection of rhGH at 2200 hours, at a dose of 0.166 mg/kg per week. Children and their parents were adequately informed, and they gave their informed consent to participate in the study, which was approved by the Ethics Committee for Clinical Research of the Hospital “Miguel Servet” of the University of Zaragoza, Spain. Controls and GHD children were white Caucasians from the same geographical area (North of Spain).
Overnight urine samples (interval from 2200 hours to 0800 hours) were collected from patients at two times: day 0 (prior to starting treatment) and day 30 (30 days after beginning rhGH treatment). In the control group, a unique urine sample was obtained, which was collected at the same time interval. Aliquots (15 ml) were immediately frozen at −80°C until analysis.
Analytic methods
6β-Hydroxycortisol was quantified according to the procedure described by Lee [22]. 6β-Hydroxycortisone was used as internal standard. Urine extraction was performed through an activated Sep-Pack C18 cartridge washed with 10 ml of 4% methanol. The column was eluted with 10 ml of ethyl acetate. After washing the eluate, it was evaporated to dryness in a 37°C bath under a gentle stream of nitrogen. The residue was dissolved in 0.2 ml of CH3OH, and an aliquot of 20 μl of the solution was injected into the high-performance liquid chromatography (HPLC) system. The reverse phase column was a 100×8 mm Radial-Pack Novapack C18 (Millipore Ibérica S.A.) with a 5-μm particle size (Waters Corporation, Madrid, Spain), which was eluted isocratically with a mobile phase containing 0.01 M KH2PO4/acetonitrile/methanol (84/5/11, v/v/v) at a flow rate of 2 ml/min and a pressure of 1500 psi. The compounds were detected by ultraviolet absorbance at 244 nm. The chromatograph was a LC Module I Plus equipped with Millenium 2010 software (Waters Corp., Madrid, Spain). We used a Waters 996 photodiode array detector (Waters Corporation, Madrid, Spain) to compare the spectral of the peaks with the spectral libraries of standards. All reagents were of analytical grade for HPLC. 6β-Hydroxycortisol and 6β-hydroxycortisone were purchased from Sigma Chemical, Co., Madrid, Spain. Within-run and between-run coefficients of variation were greater than 5.5% and 6.2%, respectively. The recovery ranged from 92% to 95% for three different concentrations of 6β-hydroxycortisol, and the limit of quantification was 26 nmol/l. Urinary free cortisol concentrations were assayed using a fluorescence polarization immunoassay method (TDX System, Abbott Diagnostics, Madrid, Spain), following the instructions of the manufacturer, after an extraction of the unconjugated cortisol with methylene chloride. Within- and between-day coefficients of variation were lower than 5%. For data analysis, 6β-hydroxycortisol and free cortisol concentrations were expressed as nanomole per liter. The metabolic ratio was calculated by the quotient 6β-hydroxycortisol/free cortisol, as indicator of CYP3A activity. Serum GH, total IGF-I and IGFBP-3 concentrations were measured by inmunoradiometric assays by Diagnostic System Laboratories (Webster, Tex., USA).
Statistical analysis
Non-parametric statistical methods were selected, since the data distributions were neither normal nor fitted to an ordinal scale. We used the Wilcoxon test or the Mann–Whitney test for paired or unpaired comparisons, respectively. The associations between variables were performed using the Spearman correlation test. Data are presented as medians and 95% confidence intervals for a better description. A P value of <0.05 was considered to be statistically significant. The statistical analysis was done using the SPSS 11.0 software for Windows.
Results
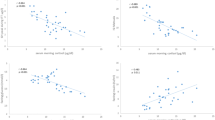
First, we investigated the influence of the age and gender on the marker of CYP3A activity. Correlation analysis and unpaired comparisons showed lack of influence of the age or sex on the 6β-hydroxycortisol/free cortisol ratio (P>0.05) both in the control group (r=0.07 and Z=−0.9) and the group of GHD children (r=0.06 and Z= −1.45). There were no significant associations between the CYP3A marker and either serum GH, IGF-I or IGFBP-3 (P>0.05 in all cases).
Table 1 summarizes unpaired and paired comparisons of the metabolic ratio between groups. GHD children displayed a strikingly higher activity than controls (P<0.0001). The differences were also significant in the two subgroups established by gender (Z=−2.37, P=0.01 for males, and Z=−2.7, P=0.007 for females).
With regard to the effect of rhGH treatment for 30 days (Table 1), the 6β-hydroxycortisol/free cortisol ratio did not change significantly in the total group of children (Z=−1.09, P>0.05). However, when males and females were analyzed separately, a significant decrease was observed after rhGH treatment in relation to day 0 in males (Z=−2.99, P<0.02). In contrast, in females, although median values tended to be higher, no significant changes were detected (Z=−1.44, P>0.05). Baseline serum GH, IGF-I or IGFBP-3 had no influence on the changes of the cortisol metabolic ratio (P>0.05 for the three correlation coefficients).
The results of the unpaired comparisons of the metabolic ratio between GH-treated children (30 days) and controls are illustrated in Table 1. Male children showed a normalization of the CYP3A marker toward values non-statistically different from those of controls (Z=−0.07, P>0.05). In contrast, females showed the opposite effect with statistically higher values than controls (Z=−3.86, P<0.001).
Discussion
To evaluate CYP3A activity, we selected the urinary ratio 6β-hydroxycortisol/free cortisol, as it is a non-invasive test. The interval of urine collection from 2200 hours to 0800 hours was chosen for several reasons. First, this time interval is more comfortable than that of 24 h, since in most cases, it implies only the collection of the first urine in the morning. Moreover, subcutaneous administration of rhGH takes place at 2200 hours, and hence the highest GH plasma concentrations are reached at night, mimicking the physiological high nocturnal GH secretion [23]. In addition, a good correlation has been reported between cortisol metabolic ratio in 24-h urine and in overnight urine [24].
The present study shows, to our knowledge, the first observation of a higher CYP3A activity in GH-deficient children in relation to controls (Table 1). The mechanism underlying this effect is unclear. Some observations in rodents demonstrate that GH suppresses CYP3A2 expression in rat liver. CYP3A2 is the steroid and xenobiotic-metabolizing enzyme in the rat that is constitutively expressed in prepubertal male and female rats [25, 26], and it does not require the presence of GH [27]. Moreover, hypophysectomy leads to increased expression of CYP3A2 in rats [28], and, conversely, overexpression of GH in transgenic mice results in both lower CYP3A2 expression and CYP3A2 enzyme activity [29].
Another novel finding of this work is the sexual dimorphism in the effect of rhGH treatment on CYP3A activity (Table 1). We have observed a marked decrease in male children toward normalization in relation to controls. In contrast, in females, the CYP3A values did not change significantly.
Previous studies conducted to examine the effect on drug metabolism of GH treatment given to GHD children show contradictory results without reference to sex differences [14–17]. Redmond et al. [14] found a significant increase in elimination half-life on amobarbital in six children after hGH therapy for 6 weeks. In contrast, these same authors reported a decrease in plasma half-life of theophylline in four children following the same therapeutic scheme. Redmond et al. [15] and Levitski et al. [16] noted a significant decrease in caffeine N-3-demethylation in six GHD children after 1 month on hGH therapy. Recently, Gil-Berglund et al. [17] observed a higher CYP3A activity in 14 GHD children after 3 months on rhGH replacement therapy.
The sexual dimorphism in CYP3A activity found here could be related to the changes in GH exposure profile as a consequence of the daily s.c. administration of rhGH. The GH secretory pattern is sexually different in humans [21] and rodents [12]. Males secrete in episodic bursts with undetectable GH levels between peaks. In contrast, females present more frequent pulses of a lower magnitude than those in males, whereas the interpulse concentrations of GH are always measurable [30, 31]. Recently, in GHD adults, it has been demonstrated that the type of GH pulses is an important factor of GH actions on CYP3A and other metabolic parameters, with an increase in CYP3A activity when GH is administered continuously (mimicking the feminine profile) and a tendency to decrease when pulses mimic the GH masculine profile [13].
The dimorphic sexual effect of GH in rodents on the expression of CYP3A2 and other cytochromes is well documented [28, 31–33], as well as the differential regulation of constitutive CYPs by GH pulse pattern [34]. GH mediates the activation of the transcriptional factor STAT 5b in a manner that enables it to act as a transcriptional activator of hepatic CYP3A2 and other genes in response to male GH pulses [35] Pulsatile GH, which is a characteristic feature of males, increases STAT 5b activation by tyrosine phosphorylation and nuclear translocation [35, 36]. The low nadir GH concentrations between pulses in males sensitize phosphotyrosine phosphatases, which allow STAT 5b to be newly phosphorylated in the following peak [37]. Continuous GH exposure, similar to the pattern of adult female rats, leads to desensitization of tyrosine phosphorylation and, consequently, to lower STAT5b activation [38].
Nevertheless, whether or not the regulation of STAT 5b depends on the secretory profile of GH in humans is unknown. However, as suggested by Jaffe et al. [13], a daily subcutaneous injection of rhGH, which has been administered to children in this study, mimics the nearly continuous feminine profile. Therefore, male GH-deficient children treated with rhGH could suffer a relative “feminization” of their GH plasma pattern with a presumable loss of some regulatory actions of GH. This could explain the decreased values of the CYP3A marker in boys from baseline to 30 days after beginning rhGH therapy with a normalization in relation to controls.
In GHD females treated with rhGH, CYP3A activity has shown a marked increase regarding controls (Table 1). A possible explanation could arise from the change in their GH profile toward more elevated and continuos levels of plasma GH. As referred to previously, the continuous profile of GH delivery increases CYP3A activity [13]. This is consistent with the higher CYP3A activity measured by the erythromycin breath test found in acromegaly patients [39], since in acromegaly, GH levels are higher, and the physiological low nadir GH concentrations are never reached [40]. The higher CYP3A activity in women in relation to men found in a previous work [20] could also be due to the more continuous hepatic exposure to GH in women, since a lack of sex differences in CYP3A activity has been found in hepatic microsomes [1]. To further reinforce this argument, the continuous presence of GH in vitro induced CYP3A4 expression in primary hepatic cells [41].
The urinary ratio 6β-hydroxicortisol/free cortisol, in spite of being one of the most successfully used biomarker to indicate CYP3A activity [42–45], also measures that of CYP3A5 isoform. CYP3A5 is polymorphically expressed, and subjects with the variant allele CYP3A5*3 have improper mRNA splicing and, consequently, lower catalytic activity [46]. A possible limitation of the present study is that we did not determine genotypes of CYP3A5. Therefore, differences between controls and patients in the proportion of carriers of the allelic variant CYP3A5*3 could presumably account for the differences found in the cortisol metabolic ratio. However, the low prevalence of the rapid phenotype/genotype in white Caucasian people (5–10%) [47, 48] makes this possibility remote.
In summary, the data suggests that: (a) GH deficiency in children produces increased CYP3A activity in a non-sex-dependent manner, (b) rhGH treatment for 30 days to GHD children causes a sexually dimorphic effect on CYP3A activity, with a decrease in males towards normalization in relation to controls. These data clearly support the notion of the central role of GH in determining the level of expression of some metabolic genes. Since changes in CYP3A activity importantly affect the metabolism of pharmacological, environmental or endogenous substrates, such as steroid hormones, the results of this study should be taken into account to avoid potential undesirable consequences in GH-deficient children.
References
Shimada T, Yamazaki H, Mimura M, Inui Y, Guengerich FP (1994) Interindividual variations in the human liver cytochrome P450 enzyme involved in the oxidation of drugs, carcinogens and toxic chemicals: studies with liver microsomes of 30 Japanese and 30 Caucasians. J Pharmacol Exp Ther 270:414–423
de Wildt SN, Kearns GL, Leeder JS, van den Anker JN (1999) Cytochrome P4503A: ontogeny and drug disposition. Clin Pharmacokinet 37:485–505
Gallagher EP, Wienkers LC, Stapleton PL, Kunze K, Eaton DL (1994) Role of human microsomal and human complementary DNA-expressed cytochromes P4501A2 and P4503A4 in the bioactivation of aflatoxin B1. Cancer Res 54:101–108
Guengerich FP (1991) Oxidation of toxic and carcinogenic chemicals by human cytochrome P450 enzymes. Chem Res Toxicol 4:391–407
Watkins PB, Turgeon DK, Saenger P, Lown KS, Kolars JC, Hamilton T, Fishman K, Guzelian PS, Voorhees JJ (1992) Comparison of urinary 6-beta-cortisol and the erythromycin breath test as measures of hepatic P450 IIIA (CYP3A) activity. Clin Pharmacol Ther 52:265–273
Anzenbacher P, Anzenbacherova E (2001) Cytochromes P450 and metabolism of xenobiotics. Cell Mol Life Sci 58:737–747
Dresser GK, Spencer JD, Bailey DG (2000) Pharmacokinetic–pharmacodynamic consequences and clinical relevance of cytochrome P450 3A4 inhibition. Clin Pharmacokinet 38:41–57
Thummel KE, Schenkman JB (1990) Effects of testosterone and growth hormone treatment on hepatic microsomal P450 expression in the diabetic rat. Mol Pharmacol 37:119–129
Gonzalez F, Liu S, Yano M (1993) Regulation of cytochrome P450 genes: molecular mechanisms. Pharmacogenetics 3:51–57
Mode A, Norstedt G, Simic B, Eneroth P, Gustafsson JA (1981) Continuous infusion of growth hormone feminizes hepatic steroid metabolism in the rat. Endocrinology 108:2103–2108
Tannenbaum GS, Martin JB (1976) Evidence for an endogenous ultradian rhythm governing growth hormone secretion in the rat. Endocrinology 98:562–570
Eden S (1979) Age and sex-related differences in episodic growth hormone secretion in the rat. Endocrinology 105:555–560
Jaffe CA, Turgeon DK, Lown K, Demott-Friberg R, Watkins PB (2002) Growth hormone secretion pattern is an independent regulator of growth hormone actions in humans. Am J Physiol Endocrinol Metab 283:E1008–E1015
Redmond GP, Bell JJ, Perel JM (1978) Effect of human growth hormone on amobarbital metabolisms in children. Clin Pharmacol Ther 24:213–218
Redmond G, Bell JJ, Nichola PS, Perel JM (1980) Effect of growth hormone on human drug metabolism: time course and substrate specificity. Pediatr Pharmacol 1:63–70
Levitsky LL, Schoeller DA, Lambert GH, Edidin DV (1989) Effect of growth hormone therapy in growth hormone-deficient children on cytochrome P450-dependent 3-N-demethylation of caffeine as measured by the caffeine 13CO2 breath test. Dev Pharmacol Ther 12:90–95
Gil-Berglund E, Johannsson G, Beck O, Bengtsson BA, Rane A (2002) Growth hormone replacement therapy induces codeine clearance. Eur J Clin Invest 32:507–512
Cheung NW, Liddle C, Coverdale S, Lou JC, Boyages SC (1996) Growth hormone treatment increases cytochrome P450-mediated antipyrine clearance in man. J Clin Endocrinol Metab 81:1999–2001
Jürgens G, Lange KHW, Reuther LO, Rasmussen BB, Brosen K, Christensen HR (2002) Effect of growth hormone on hepatic cytochrome P450 activity in healthy elderly men. Clin Pharmacol Ther 71:162–168
Watkins PB, Murray SA, Winkelman LG, Heuman DM, Wrighton SA, Guzelian PS (1989) Erythromycin breath test as an assay of glucocorticoid-inducible liver cytochrome P-450. J Clin Invest 83:688–697
Jaffe CA, Ocampo-Lim B, Guo W, Krueger K, Sugahara I, DeMott-Friberg R et al (1998) Regulatory mechanisms of growth hormone secretion are sexually dimorphic. J Clin Invest 102:153–164
Lee C (1995) Urinary 6β-hydroxycortisol in humans: analysis, biological variations, and reference range. Clin Biochem 28:49–54
Van Cauter E, Kerkhofs M, Caufriez A, Van Onderbergen A, Thorner MO, Copinschi G (1992) A quantitative estimation of growth hormone secretion in normal man: reproducibility and relation to sleep ant time of day. J Clin Endocrinol Metab 74:1441–1450
Kovacs SJ, Martin DE, Everitt DE, Patterson SD, Jorkasky DK (1998) Urinary excretion of 6β-hydroxycortisol as an in vivo marker for CYP3A induction: applications and recommendations. Clin Pharmacol Ther 63:617–622
Yamazoe Y, Murayama N, Shimada M, Yamauchi K, Nagata K, Imaoka S, Funae Y, Kato R (1988) A sex specific form of cytochrome P-450 catalyzing propoxycoumarin O-depropylation and its identity with testosterone 6β-hydroxylase in untreated rat livers: reconstitution of the activity with microsomal lipids. J Biochem 104:785–790
Wright MC, Edwards RJ, Pimenta M, Ribeiro V, Ratra GS, Lechner MC, Paine AJ (1997) Developmental changes in the constitutive and inducible expression of cytochrome P450 3A2. Biochem Pharmacol 54:841–846
Kawai M, Bandiera SM, Chang TKH, Bellward GD (2000) Growth hormone regulation and developmental expression of rat hepatic CYP3A18, CYP3A9, and CYP3A2. Biochem Pharmacol 59:1277–1287
Lemoine A, Marie S, Cresteil T (1988) Expression of cytochrome P450 isozymes in the liver of hypophysectomized rats. Evidence for different regulation mechanisms concerning P450IIB and P450IIIA subfamilies. Eur J Biochem 177:597–604
Cheriathundam E, Doi SQ, Knapp JR, Jasser MZ, Kopchick JJ, Alvares AP (1998) Consequences of overexpression of growth hormone in transgenic mice on liver cytochrome P450 enzymes. Biochem Pharmacol 55:1481–1487
Shapiro BH, Agrawal AK, Pampori NA (1995) Gender differences in drug metabolism regulated by growth hormone. Int J Biochem Cell Biol 27:9–20
Legraverend C, Mode A, Wells T, Robinson I, Gustafsson JA (1992) Hepatic steroid hydroxylating enzymes are controlled by the sexually dimorphic pattern of growth hormone secretion in normal and dwarf rats. FASEB J 6:711–718
Waxman DJ, Leblanc GA, Morrissey JJ, Staunton J, Lapenson DP (1988) Male-specific and neonatally programmed rat hepatic P-450 forms RLM2 and 2a are not dependent on pulsatile plasma growth hormone for expression. J Biol Chem 263:11396–11406
Waxman DJ, Ram PA, Pampori NA, Shapiro BH (1995) Growth hormone regulation of male-specific rat liver P-450 2A2 and 3A2: induction by intermittent growth hormone pulses in male but not female rats rendered growth hormone deficient by neonatal monosodium glutamate. Mol Pharmacol 48:790–797
Mode A, Ahlgre R, Lahuna O, Gustafsson JA (1988) Gender differences in rat hepatic CYP2C gene expression-regulation by growth hormone. Growth Horm IGF Res 8[Suppl B]:61–67
Waxman DJ, Ram PA, Park SH, Choi K (1995) Intermittent plasma growth hormone triggers tyrosine phosphorylation and nuclear translocation of a liver-expressed, Stat5-related ADN binding protein. J Biol Chem 270:13262–13270
Ihle JN, Witthuhn BA, Quelle FW, Yamamoto K, Thierielder WE, Kreider B, Silvennoinen O (1994) Signaling by the cytokine receptor superfamily: JAKs and STATs. Trends Biochem Sci 19:222–227
Ram PA, Waxman DJ (1997) Interaction of growth hormone-activated STATs with SH2-containing phosphotyrosine phosphatase SHP-1 and nuclear JAK2 tyrosine kinase. J Biol Chem 272:17694–17702
Gebert CA, Park SH, Waxman DJ (1999) Down-regulation of liver JAK2-STAT5b signaling by the female plasma pattern of continuous growth hormone stimulation. Mol Endocrinol 13:213–227
Watkins PB, Turgenon DK, Jaffe CA, Ho PJ, Barkan AL (1993) Pulsation frequency of growth hormone may mediate gender differences in CYP3A activity in man (abstract). Clin Res 41:132
Matthews DR, Hindmarsh PC, Pringle PJ, Brook CG (1991) A distribution method for analysing the baseline of pulsatile endocrine signals as exemplified by 24-hour growth hormone profiles. Clin Endocrinol (Oxf) 35:245–252
Lidle C, Goodwin BJ, Geoerge J, Tapner M, Farrell GC (1998) Separate and interactive regulation of cytochrome P450 3A4 by triiodothyronine, dexamethasone, and growth hormone in cultured hepatocytes. J Clin Endocrinol Metab 83:2411–2416
Boulton DW, Arnaud P, DeVane CL (2001) A single dose of methadone inhibits cytochrome P450 3A in healthy volunteers as assessed by the urinary cortisol ratio. Br J Clin Pharmacol 51:350–354
Lillibridge JH, Liang BH, Kerr BM, Webber S, Quart B, Shetty BV, Lee CA (1998) Characterization of the selectivity and mechanism of human cytochrome P450 inhibition by the human immunodeficiency virus-protease inhibitor nelfinavir mesylate. Drug Metab Dispos 26:609–616
Morita K, Konishi H, Shimakawa H (1992) Fluconazole: a potent inhibitor of cytochrome P-450-dependent drug metabolism in mice and human in vivo-comparative study with ketoconazole. Chem Pharm Bull 40:1247–1251
Konishi H, Takenaka A, Minouchi T, Yamaji A (2001) Impairment of CYP3A4 capacity in patients receiving danazol therapy: examination on oxidative cortisol metabolism. Horm Metab Res 33:628–630
Lamba JK, Lin YS, Schuetz EG, Thummel KE (2002) Genetic contribution to variable human CYP3A-mediated metabolism. Adv Drug Deliv Rev 54:1271–1294
van Schaik RHN, van der Heiden IP, van den Anker JN, Lindemans J (2002) CYP3A5 variant allele frequencies in Dutch Caucasians. Clin Chem 48:1668–1671
Hustert E, Haberl M, Burk O, Wolbold R, He YQ, Klein K, Nuessler AC, Neuhaus P, Klattig J, Eiselt R, Koch J, Zibat A, Brockmoller J, Halpert JK, Zanger UM, Wojnowski L (2001) The genetic determinants of the CYP3A5 polymorphism. Pharmacogenetics 11:773–779
Acknowledgements
We thank Susana García for her technical assistance in determining the biochemical parameters. This work was supported by Pfizer Endocrine Care (Contract 980003), and Ministerio de Ciencia y Tecnología (MCYT), Spain (Reference SAF 2003-06878).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sinués, B., Mayayo, E., Fanlo, A. et al. Effects of growth hormone deficiency and rhGH replacement therapy on the 6β-hydroxycortisol/free cortisol ratio, a marker of CYP3A activity, in growth hormone-deficient children. Eur J Clin Pharmacol 60, 559–564 (2004). https://doi.org/10.1007/s00228-004-0806-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-004-0806-4