Abstract
Background
Italy is reported to have a relatively low consumption of antidepressants. This is probably due to the fact that until 2000 antidepressants were reimbursed with some restrictions.
Aim
To describe the pattern of use of antidepressants in primary care in Italy, after admission of selective serotonin reuptake inhibitors (SSRIs) for reimbursement without restrictions.
Methods
We collected prescription data of antidepressants (ATC code: N06) reimbursed between January 1999 and March 2002 from three local health authorities in Emilia Romagna. Then, we calculated the prevalence of use for the different therapeutic classes of antidepressants, by age and gender. Moreover, after selecting a cohort of incident adult patients to follow for 6 months after the first prescription, we analysed the continuity, the average daily doses and the average duration of treatment.
Results
Out of 1000 subjects, 78 received at least one prescription of antidepressants in 1 year. The prevalence of use increased with age from 43 to 136/1000. Women used antidepressants more frequently than men, with a ratio varying from 1.6 to 2, depending on age. SSRIs were the most used drugs (63%), and their prevalence of use diminished with age; on the contrary, use of mianserine and trazodone increased with age, and that of the other antidepressants did not vary. About 60% of the subjects received occasional prescriptions. Continuous treatment was more frequent with SSRIs and in subjects older than 34 years. Daily doses were higher in patients receiving newer drugs (0.9–1 DDD per day), and lower in patients receiving the older agents (0.3–0.4 DDD per day). The average daily doses were usually lower than those recommended for the treatment of the major depression, especially for tricyclics, trazodone and reboxetine. Overall, doses were within the recommended range in about 75% of recipients of newer antidepressants (i.e., SSRIs, venlafaxine, mirtazapine and reboxetine), and in less than 30% of recipients of older drugs (i.e., tricyclics, trazodone and mianserine). In 59% of subjects receiving continuous treatment, the duration of the therapeutic course was at least 6 months.
Conclusions
We found a high prevalence of use of antidepressants in primary care with a frequency of occasional use higher than in other countries. Only rarely were doses and duration of treatment consistent with recommendations for treatment of depression. Recipients of newer drugs received doses consistent with a use for major depression more frequently than others; however, rates of 6 month duration did not differ among drug classes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the last two decades, surveys performed in several countries reported a high use of antidepressants in general practice with a relatively high risk of inappropriate use [1], because some antidepressants may be prescribed for a variety of minor indications, such as temporary control of anxiety disorders. Although Italy is traditionally reported as a country with a low prescription of antidepressants [2], the amount of prescriptions considerably increased in the last 5 years because of recent changes in the policy of drug reimbursement [3, 4]. Before April 1999, only tricyclic antidepressants and a few atypical agents were reimbursed by the National Health Service. After April 1999, selective serotonin reuptake inhibitors (SSRIs) and some newer compounds were admitted for reimbursement with restrictions (i.e. only to patients with contraindications to tricyclics). Subsequently, in February 2001, restrictions were removed and antidepressant utilisation data are now free from the biases deriving from reimbursement restriction.
With this background in mind, we designed this study to report the pattern of use of antidepressants in Italian primary health care during and immediately after the period of transition to reimbursement for all compounds without restrictions. Moreover, we aimed at evaluating whether antidepressant use was consistent with the most authoritative recommendations about doses and duration of treatment in major depression (i.e. 6-week treatment to achieve clinical improvement and a duration of at least 6 months to reduce the risk of relapse) [5, 6, 7, 8].
Methods
Data
Antidepressant prescription data were retrieved from the Emilia Romagna Regional Health Authority Database [9]. This database provides the following information for each reimbursed prescription: identification number of the dispensed product, ATC (Anatomical Therapeutic Chemical) code, number of packages and number of DDD (defined daily doses) dispensed [10], code of the patient, date of prescription. The patient code allows to retrieve each individual’s drug history without identification of the individual.
We collected all the prescriptions of antidepressant drugs (ATC code: N06A), reimbursed between January 1999 and March 2002, focusing on three local health authorities of Emilia Romagna (Piacenza, Bologna and Ravenna with a total number of 999,364 inhabitants) [11].
In order to assess the time course of sales before and after the changes of the reimbursement status, we also used the national wholesale data of antidepressants (IMS Health—Italy), as kindly provided by the “Osservatorio Nazionale sull’impiego dei medicinali (OsMed)” of the Italian Ministry of Health (http://www.ministerosalute.it/medicinali/osmed/osmed.jsp). From the same source (OsMed), we also obtained data of national reimbursed prescriptions.
Analysis of general pattern
Antidepressants were divided into four classes.
-
Tricyclics: desipramine, imipramine, clomipramine, trimipramine, amitriptyline, nortriptyline (ATC N06AA)
-
Selective serotonin reuptake inhibitors (SSRI): fluoxetine, citalopram, paroxetine, sertraline, fluvoxamine (ATC N06AB)
-
Older “other antidepressants”: mianserine, trazodone, viloxazine (this compound is no longer marketed) (ATC N06AX03, N06AX05, N06AX09)
-
Newer “other antidepressants”: mirtazapine, venlafaxine, reboxetine (ATC N06AX11, N06AX16, N06AX18)
Over the entire period of interest (January 1999 through March 2002), we calculated the monthly prevalence of use of antidepressants as number of subjects receiving any antidepressant out of 1000 inhabitants.
Analysis of continuity, doses and duration of treatments
We selected a cohort of incident patients receiving their first prescription in September 2001 and analysed all their subsequent prescriptions over a 6-month period. Occasional treatment was defined as: (a) a single prescription over the entire observation period or (b) a period between the first and the last prescription shorter than 10 days or (c) a daily dose lower than the minimal unit dose (one tablet or a half scored tablet).
For subjects receiving more than one antidepressant, only those prescribed at the time of recruitment were considered for the subsequent analysis, and each drug was considered separately.
According to Rosholm et al. [12], the average daily dose and the duration of each treatment were calculated as follows:
and
where DDDs = number of DDDs received before the last prescription; days = number of days between the first and the last prescription; and last DDDs =number of DDDs contained in the last prescription.
The average daily doses were evaluated for each antidepressant agent and for each drug class. For agents prescribed to more than 15 patients, the average daily dose was compared with doses recommended for the treatment of major depression [13].
Moreover, we evaluated the average duration of treatment, excluding the occasional ones (see definitions above), and for each class we calculated the percentage of patients completing a 6-month course (the course was considered complete when it covered at least 160 days).
Results
Time course of antidepressant prescriptions
In the period 1999–2001, the monthly prevalence of use of antidepressants increased fourfold, from 5 to 20 subjects/1000 inhabitants (Fig. 1). The main variations occurred in April 1999 (after the first change in reimbursement status) and in February 2001 (after the second change), with major increases in the use of SSRI (up to 13 subjects/1000 inhabitants) and also of newer “other antidepressants” (up to 3 subjects/1000 inhabitants). The prescriptions of the older classes, including tricyclics and older “other antidepressants”, were virtually unchanged. In the same period, national wholesale data of all antidepressants increased from 11 (1999) to 19 (2001) DDD/1000 inhabitants per day, and SSRI showed an even more pronounced increase (from 6 to 14 DDD).
Table 1 shows a comparison of antidepressant consumption (DDD/1000 inhabitants per day) between the LHAs included in this study, the Emilia Romagna region and the other Italian regions. Data from the LHAs were similar to those from Emilia Romagna, which, in turn, was one of the regions with the highest consumption in Italy.
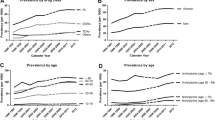
Year prevalence of use by age and gender
After February 2001 (no restriction to reimbursement of antidepressants), the overall year prevalence of use was 78/1000 inhabitants. The prevalence increased with age (Table 2) and, independently of age, women used antidepressants more frequently than men, with a ratio varying from 1.6 to 2.
SSRIs were the most used drugs in every age class (57–71% of the subjects receiving antidepressants), but their proportion diminished with increasing age (−14% in the subjects older than 65 years versus subjects 20–34 years); however, the proportion of older “other antidepressants” increased (+15%, Table 3).
Continuity, dose and duration of treatment
Table 4 shows the rate of continuous treatments prescribed to adults for the different classes of drugs. Of the 2834 subjects 20 years or older observed for 6 months after the first prescription, 60% received only occasional prescriptions. A continuous treatment was more frequent with SSRI (39%) and in subjects older than 34 years.
Daily doses were higher in patients receiving SSRI (about 1 DDD per day on average) or newer “other antidepressants” (0.9 DDD per day) and consistent with recommendations for major depression (Table 5 and Fig. 2). On the contrary, average daily doses in patients receiving the older classes were very low (0.4 and 0.3 DDD per day) and were not consistent with recommended doses. Overall, the doses were consistent with the recommendations in approximately 75% of the recipients of newer antidepressants, and for less than 30% of the recipients of older drugs.
Comparison of average daily doses received by subjects under continuous treatment (black squares) and range of recommended daily doses for the treatment of major depression (dash bars). Recommended doses were obtained from a recent review [13] and were adapted to formulations marketed in Italy. Values are expressed as fractions of defined daily doses (DDD)
Overall, 23% of the patients in the cohort received therapeutic courses lasting at least 6 months; while the proportion was 59% when only subjects under continuous treatment were considered (Table 6). The values were very heterogeneous among drug and age classes; in particular, a 6-month duration was more frequent in subjects older than 34 years receiving older “other antidepressants” (58–71%), whereas the percentage was very low for 20–34 receiving older classes (25–33%) or 35–49 receiving newer “other antidepressants” (39%).
Discussion
This is the first study providing detailed information on prevalence, doses and duration of treatment with antidepressants in Italian primary health care after removal of the reimbursement restrictions. The main finding of our study was that Italy can no longer be considered as a country with a low consumption of these drugs [2] because of the very high prevalence of antidepressant prescriptions in general practice (approximately 8 of 100 adults received prescriptions in a year). When wholesale data are considered, it appears that the recent changes in reimbursement status of antidepressants were followed by a marked overall increase in SSRI consumption and not only by a transfer from private to public expenditure.
The prevalence of use observed in our study is in accordance with the report by Tansella and De Girolamo on the prevalence of patients treated for depression and related disorders (anxiety, situational and reactive disorders) in general practice in Italy [14].
An increase of antidepressant use is also confirmed by the comparison with other Italian studies: the first, performed in 1990–1992 before marketing of most new antidepressants, reported a 30-month prevalence of 5.4% [15]; another recent Italian study using a reimbursement database, performed in 2000, found a 6-month prevalence of 1.9%, but its results cannot be considered fully representative, since the described restrictions to SSRI reimbursement were still operative [4]. Moreover, the results of these studies cannot be easily compared with our data because prevalence of use was based on periods of variable length.
Our data should be compared to those available for countries with a high rate of depressive disorders such as Sweden and Denmark. In those countries, a prevalence of use of antidepressants in 1996 of 3.8% and 4.1%, respectively, was reported [16, 17]. Apart from possible differences in the prevalence of depression, the lower prevalence of antidepressant use could be explained by the fact that, in those countries, antidepressants were prescribed only for severe depression.
The methodology and the results of the present paper cannot answer the question whether depression is actually increasing in Italy or is simply more frequently recognised. The issue whether doctors are using antidepressants mostly to treat minor disorders also remains unclear. Different approaches, including questionnaires to doctors or analysis of medical records, should be followed to answer these questions.
The absence of reimbursement restrictions and the perception of a safer profile for SSRIs probably induced the high frequency (60%) of sporadic prescriptions observed by us and this rate was the highest among published data [16, 17]. Moreover, only rarely were doses and duration consistent with recommendations for the treatment of major depression. A similar pattern of antidepressant use was reported by other studies performed in different countries: in the already-mentioned study by Arpino et al. [15], only 11% of treatments were longer than 2 months; in U.K., treatments were in accordance with guidelines in 1–6% of patients receiving tricyclics and in 29–33% of patients receiving SSRIs [18, 19, 20]. Although the use of lower doses is said to be useful in some circumstances [21], it should be kept in mind that, also for mood disorders frequently observed in general practice such as disthymia, some weeks of treatment are needed to achieve the first response and a treatment period of at least 6 months is required to complete the therapy [8].
Moreover, as widely reported in the literature [12, 16, 20, 22, 23], we observed that newer antidepressants were prescribed more frequently at doses consistent with the recommendations than older agents. It is hard to believe that this empirical finding is due to doctors’ awareness about the possible efficacy of low doses of tricyclics [21]; rather, it is more likely to be related to doctors’ worries about the toxicity of these drugs. An additional technical reason of the above finding may be that only tricyclics are commercially available in Italy also as low-strength preparations, whereas SSRIs are presented only as full-dose formulations.
Data shown in the present study were average values coming from all the GPs working in the three local health authorities considered, and the rate of inappropriate prescribing observed could be not uniformly distributed among them. As reported by Gilda Hansen et al. in a recent issue of this journal [24], a high inter-practice variability exists; therefore, further studies evaluating this variability and identifying factors involved in inappropriate pattern of antidepressant prescription are needed.
Some limitations of this study must be acknowledged. First, no information about the diagnosis were available in our database; therefore, we could not directly evaluate the accordance of prescriptions with the recommendations for the treatment of depression. However, since a minimal duration of treatment should be ensured, whatever the diagnosis, the findings of the present study concerning occasional use at least point out a scarce appropriateness in antidepressant use. Moreover, our study did not take into account the data of drugs directly dispensed by the Mental Health Services (about 5% of total consumption, without differences among drug classes); however, this was beyond the scope of the present investigation, which aimed at assessing prescriptions in general practice, i.e., in a population different from that treated by the Mental Health Services. A further limitation is that by analysing only reimbursement data, we could underestimate the prevalence of use. Moreover, some patients could have been considered as occasional users only because they purchased some prescriptions without reimbursement.
In conclusion, this study showed a considerable use of antidepressants in general practice in Italy, largely at low doses and with short-term courses. Such a pattern of use is not consistent with the recommendations for the treatment of depression, and this suggests that antidepressants are often used to treat minor disorders, in which they have not been demonstrated to be more effective than non-pharmacological therapies or placebo. In consideration of the high cost of the most widely used antidepressants, such as SSRI agents, educational interventions addressed to limit inappropriate prescription of these drugs should be undertaken.
References
Donoghue J, Hylan TR (2001) Antidepressant use in clinical practice: efficacy v. effectiveness. Br J Psychiatry Suppl 42:S9–S17
McManus P, Mant A, Mitchell PB, Montgomery WS, Marley J, Auland ME (2000) Recent trends in the use of antidepressant drugs in Australia, 1990–1998. Med J Aust 173:458–461
Osseratorio nazionale sull’impiego dei medicinali (2002) L’uso dei farmaci in Italia—rapporto nazionale anno 2001
Pietraru C, Barbui C, Poggio L, Tognoni G (2001) Antidepressant drug prescribing in Italy, 2000: analysis of a general practice database. Eur J Clin Pharmacol 57:605–609
Whooley MA, Simon GE (2000) Managing depression in medical outpatients. N Engl J Med 343:1942–1950
Anderson IM, Nutt DJ, Deakin JF (2000) Evidence-based guidelines for treating depressive disorders with antidepressants: a revision of the 1993 British Association for Psychopharmacology guidelines. British Association for Psychopharmacology. J Psychopharmacol 14:3–20
Anonymous (2000) Practice guideline for the treatment of patients with major depressive disorder (revision). American Psychiatric Association. Am J Psychiatry 157:1–45
Simon GE (2002) Evidence review: efficacy and effectiveness of antidepressant treatment in primary care. Gen Hosp Psychiatry 24:213–224
Montanaro N, Vaccheri A, Magrini N, Battilana M (1992) FARMAGUIDA: a databank for the analysis of the Italian drug market and drug utilization in general practice. Eur J Clin Pharmacol 42:395–399
WHO Collaborating Centre for Drug Statistics Methodology (Norway) (2000) ATC index with DDDs
Anonymous (2002) Web site of the Regional Government of Emilia Romagna by January 2003:http://www.regione.emilia-romagna.it/sas/statistica/
Rosholm JU, Gram LF, Isacsson G, Hallas J, Bergman U (1997) Changes in the pattern of antidepressant use upon the introduction of the new antidepressants: a prescription database study. Eur J Clin Pharmacol 52:205–209
Williams JWJ, Mulrow CD, Chiquette E, Noel PH, Aguilar C, Cornell J (2000) A systematic review of newer pharmacotherapies for depression in adults: evidence report summary. Ann Intern Med 132:743–756
Tansella, M De Girolamo G (2001) Il ruolo del medico in medicina generale. In: Salute mentale: contro il pregiudizio, il coraggio delle cure.http://www.salutementale-oms.it/Medico.htm
Arpino C, Da Cas R, Donini G, Pasquini P, Raschetti R, Traversa G (1995) Use and misuse of antidepressant drugs in a random sample of the population of Rome, Italy. Acta Psychiatr Scand 92:7–9
Isacsson G, Boethius G, Henriksson S, Jones JK, Bergman U (1999) Selective serotonin reuptake inhibitors have broadened the utilisation of antidepressant treatment in accordance with recommendations. Findings from a Swedish prescription database. J Affect Disord 53:15–22
Rosholm JU, Andersen M, Gram LF (2001) Are there differences in the use of selective serotonin reuptake inhibitors and tricyclic antidepressants( A prescription database study. Eur J Clin Pharmacol 56:923–929
MacDonald TM, McMahon AD, Reid IC, Fenton GW, McDevitt DG (1996) Antidepressant drug use in primary care: a record linkage study in Tayside, Scotland. BMJ 313:860–861
MacDonald TM, Reid IC, McMahon AD (1997) Patients receive an inadequate dose of antidepressants for an inadequate period. BMJ 315:56
Dunn RL, Donoghue JM, Ozminkowski RJ, Stephenson D, Hylan TR (1999) Longitudinal patterns of antidepressant prescribing in primary care in the UK: comparison with treatment guidelines. J Psychopharmacol 13:136–143
Furukawa TA, McGuire H, Barbui C (2002) Meta-analysis of effects and side effects of low dosage tricyclic antidepressants in depression: systematic review. BMJ 325:991
Lawrenson RA, Tyrer F, Newson RB, Farmer RD (2000) The treatment of depression in UK general practice: selective serotonin reuptake inhibitors and tricyclic antidepressants compared. J Affect Disord 59:149–157
McManus P, Mant A, Mitchell P, Britt H, Dudley J (2003) Use of antidepressants by general practitioners and psychiatrists in Australia. Aust N Z J Psychiatry 37:184–189
Gilsa HD, Sondergaard J, Vach W, Freng GL, Rosholm JU, Kragstrup J (2003) Antidepressant drug use in general practice: inter-practice variation and association with practice characteristics. Eur J Clin Pharmacol 59:143–149
Acknowledgements
The study was supported by grants from the Regione Emilia Romagna Health Authority. For supplying prescribing data, the authors wish to thank the pharmacists of participating local health authorities: Francesco Pacella, Maria Vittoria Novi, Marco Manzoli and Mirna Magnani. We also thank Mr. Roberto Da Cas (OsMed, Rome) for kindly supplying data of other Italian regions.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Poluzzi, E., Motola, D., Silvani, C. et al. Prescriptions of antidepressants in primary care in Italy: pattern of use after admission of selective serotonin reuptake inhibitors for reimbursement. Eur J Clin Pharmacol 59, 825–831 (2004). https://doi.org/10.1007/s00228-003-0692-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-003-0692-1