Abstract
Worldwide, a care gap has been recognized between presenting with a fracture and prevention of the next fracture. Fracture Liaison Service is the most cost-effective method to close this gap, but its implementation is sparse in the Nordic countries. To assess the need for a fracture prevention program, the primary aim of this study was to estimate the prevalence of osteoporosis in patients treated for fragility fractures at Aarhus University Hospital, Denmark. Secondary aims were to identify clinical risk factors associated with osteoporosis and the up-take of anti-osteoporosis treatment. The study was conducted as a cross-sectional study and patients aged 18+ years were consecutively identified over a 12 months period. Of 1164 identified patients, 832 were included and 794 (70% women, 66% aged ≥ 50 years) patients completed the study. Bone mineral density was measured by DXA and information about clinical risk factors were obtained. The overall prevalence of osteoporosis in this cohort was 14.9%, increasing to 20.3% in patients ≥ 50 years (22.9% in women, 9.6% in men). In addition to age above 50 years, female sex, low BMI, and early menopause were significantly associated with osteoporosis. At 3-years follow-up in patients diagnosed with osteoporosis, 95% of patients who initiated anti-osteoporosis treatment after their fracture were still adherent to treatment. Given that osteoporosis was demonstrated in one in five fragility fracture patients above 50 years, OFELIA stresses the need for implementation of a program aiming at securing appropriate investigation and treatment of osteoporosis in patients presenting a fragility fracture.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a systemic skeletal condition characterized by low bone mass and micro architectural deterioration of bone that increases bone fragility and risk of fractures [1,2,3]. It is a common but under-diagnosed disease in most parts of the world [4,5,6,7,8]. The clinical consequence of osteoporosis is fractures, and the ultimate goal of treating osteoporosis is to prevent fractures and reduce the associated morbidity and mortality [9]. Pharmacological treatments that effectively reduce both first and subsequent fractures in men and women are available [10,11,12,13,14,15]. Given that low-energy fractures are associated with a two-to-four fold increased risk of subsequent fractures and their associated risk of premature mortality [16, 17], patients, who already have sustained a fracture, are relevant candidates for osteoporosis investigation and subsequent fracture prevention. The International Osteoporosis Foundation (IOF) suggests that the single most important thing that can directly improve patient care and reduce spiraling fracture-related healthcare costs worldwide is the implementation of Fracture Liaison Service (FLS) [18, 19]. FLS is a coordinator-based, post-fracture model of care to ensure, that patients aged 50 years or older suffering fragility fractures receive appropriate assessment and intervention to reduce future fractures. Two decades ago, FLS was successfully implemented in Glasgow, Scotland [20], and today FLS covers more than half of United Kingdom [21]. The documented reduction in fractures, especially disabling hip-fractures, as a result of FLS is an important outcome for the patients as well as the society [5, 18, 22]. Despite evidence of cost effectiveness of organized fracture prevention programs and on-going international campaigns, a care gap remains worldwide in the prevention of subsequent fractures in fracture patients [23,24,25]. To bridge the care gap, the Task Force Report [26] performed in 2012 by an international group representing 36 countries urged: “At a systems level, when a patient presents with a fracture to the emergency room or to an orthopedist, there should be a care pathway in place to ensure that clinicians evaluate for osteoporosis, future fracture risk, and for the need for treatment for prevention of secondary fractures”.
In Denmark, only one in four of 500,000 individuals estimated by World Health Organisation (WHO) to have osteoporosis is diagnosed according to Health Government in Denmark, and despite campaigns and national recommendations, the majority of the 50,000 patients above 50 years, who annually sustain a fracture [27], does not receive appropriate investigation and assessment of future fracture risk. Prevention of subsequent fractures is therefore very limited.
Thus, to assess the need for FLS in a context, where implementation of fracture prevention programs is sparse and the population may differ from the UK population, the aim of the present study was to estimate the prevalence of osteoporosis and identify clinical risk factors related to osteoporosis in a Danish population of fragility fracture patients. Since being younger than 50 years or a man has been shown to be associated with lower rates of investigation for osteoporosis [28], we included both male and female fracture patients aged 18 years or more in this study.
Materials and Methods
Study Design
Osteoporosis Fracture Liaison Aarhus (OFELIA) was conducted as a cross-sectional study in a population of patients presenting with fractures after low-energy traumas (fragility fractures). A low-energy trauma was defined as a fall from same level (slip) or maximum 1 m. No motor vehicles could be involved. Fractures caused by the hit of a ball or another person’s hand during sport were included. Inclusion criterion was patients at or above the age of 18 years (no upper limit) presenting with a fragility fracture. Exclusion criteria were pathological fractures, fractures at face or skull, dementia, or difficulties in understanding Danish in speaking and reading.
Participants were recruited from the Emergency Department (ED), the Orthopedic Department, Trauma Unit (OD), and the fracture clinics (FC) at Aarhus University Hospital (AUH) in the period from 1st of May 2014 until 30th of April 2015. Due to the logistics at AUH, spine fracture patients normally bypass the acute wards and are admitted directly to the specialized unit of spine surgery or to the internal medicine wards if surgery is not needed and therefore only spine fracture patients admitted to ED or OD were potential participants. AUH is located in the second largest city in Denmark and serves 320,000 inhabitants. Approximately 4000 patients aged 18 years and older are annually treated for a fracture at AUH.
Methods
Bone mineral density (BMD) of the hip (total hip, femoral neck, trochanter) and spine was measured by Dual energy X-ray Absorptiometry (DXA) by trained and experienced technicians using one of three Hologic discovery system (Hologic Inc., Waltham, MA, USA) DXA-scanners, all routinely calibrated with routine daily quality control. The primary result of the DXA was categorized as “normal”, “osteopenia”, or “osteoporosis” using the standard BMD-based diagnostic criteria at the total hip or spine (normal: T-score ≥ − 1; osteopenia: T-score between − 1 and − 2.5; and osteoporosis: T-scores ≤ − 2.5) [29]. If a DXA had been performed within 12 months prior to the fracture, these results were used. Body height and weight (wearing in-doors clothing and without shoes) were measured at the time of DXA.
A questionnaire capturing history of fractures in adulthood, co-morbidities, medical treatments, lifestyle, and other risk factors for osteoporosis was answered retrospectively by the participants. The risk factors asked were identified from guidelines and the fracture risk assessment tool; FRAX [30].
Body mass index (BMI) was calculated, and low BMI was in this study defined as BMI < 20 kg/m2. “Early menopause” was set to be menopause in women younger than 46 years. Menopause was defined as a period of 12 month without menstruation; meaning that the last menstrual bleeding happened before the age of 45 years.
Identification and Inclusion of Participants
Potential participants were identified by the health-professionals at the ED, OD, and FC and asked for their permission to be contacted by phone within 2–3 week. In order to facilitate recruitment, an illustrated website and a hand-out card in pocketsize (OFELIA-card) provided relevant study information including contact details of the study coordinator (a clinical nurse specialist). Identified patients were registered in log-books present in the different departments. If given permission, the study coordinator contacted the potential participant by phone. During this conversation, in-depth information about the study and the association between bone health, bone strength and fracture risk were given. Supplementation with D-vitamin and calcium was recommended and practical issues related to DXA were explained. DXA was scheduled within the following 2–12 weeks. Written patient information, informed consent form and a questionnaire were mailed after the enrolling phone call and returned in connection with DXA. DXA was performed by trained technicians, who also collected the informed consent form, briefly reviewed the answering of the questionnaire, and if needed assisted the patients in answering the questionnaire. The interpretation of DXA was performed by consultant endocrinologists. Outcome and further advices were mailed to the patient’s general practitioner (GP), who was responsible for follow-up, including further investigation and treatment, if needed. In case of T-scores ≤ − 2.5, the study coordinator contacted the patient within 1 week from time of DXA to provide information about the result, to offer blood tests for secondary osteoporosis, and to secure involvement of the patients’ GP for further investigation and treatment.
Follow-Up in Patients Diagnosed with Osteoporosis
Patients diagnosed with osteoporosis in OFELIA were contacted by phone 3 years after their enrollment in OFELIA to answer questions about treatment, subsequent fractures and results of new DXA scans if performed.
Statistical Analysis
Characteristics of the fracture patients are presented as numbers and percentages [n (%)] for categorical variables and range, mean, and standard deviation [mean (SD)] for continuous variables. QQ-plots and histograms were used to evaluate if the continuous variables followed a normal distribution. Age, sex, BMI, and other potential confounders were compared across BMD categories (normal, osteopenia, or osteoporosis), using Chi-squared tests for categorical variables and analysis of variance (ANOVA) for continuous variables. Associations between risk factors and osteoporosis were investigated in logistic regression models, adjusting for age and sex, and reported as odds ratios (OR) with 95% confidence intervals (95% CI). Statistical analyses were carried out using STATA 13 (Stata Corporation, College Station, TX, USA).
Results
Participants
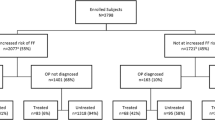
A total of 1164 consecutive fracture patients were identified and approached by the health-professionals (Fig. 1). Of these, 75 patients refused immediately any contact whereas 1089 patients accepted to be contacted for further information (group A). A group of 136 patients (12.5%) were unreachable after 3–8 phone calls at different times and weekdays (group B), and 59 patients (5.4%) were after being contacted found to be ineligible for inclusion in accordance with the inclusion- and exclusion criteria (group E). A group of 62 patients (5.7%) refused participation (group C) mostly due to lack of surplus related to co-morbidities or practical problems related to e.g., transportation, opening hours. A total of 832 patients (76.4% of the identified fracture patients) were enrolled in OFELIA, but 38 patients (3.5%) never showed up for DXA (group D). The final study population (72.9% of those contacted) therefore consisted of 794 participants; 237 men and 557 women between 18 and 93 years, who answered the questionnaire and were investigated by DXA within 2–16 weeks after their fracture episode. All patients were mobilized at the time of DXA. The eligible 311 approached non-participants fell in four groups (referred to as A, B, C and D in Fig. 1). Details on these patients are shown in Supplementary Table A.
Descriptive Data
Characteristics of the 794 participants are shown in Table 1 stratified according to sex. A total of 527 (66.4%) participants were 50 years or older. On average female participants were 11 years older than males. BMI was similar (26.2 and 25.9) in male and female participants. DXA were performed within 2–16 weeks from the fracture episode in 738 (92.9%) participants in OFELIA, as 56 participants had a recent (< 12 months) DXA. Of these 56 participants already knowing their bone health status, 20 (35.7%) patients had osteoporosis.
The total of 859 fractures occurred in 794 patients, 59 patients had more than one fracture, in most cases fractures at the same extremity. Five patients had three fractures each, and one patient suffered four fractures; shoulder, forearm, hand, and hip after a slip on the grass while exercising her dog.
Characteristics of participants stratified by their BMD T-score as osteoporotic, osteopenic, or normal are presented in Table 2. The prevalence of osteoporosis in the overall study population was 14.9%. More women (18.7%) than men (5.9%) had osteoporosis, in patients aged ≥ 50 years the prevalence of osteoporosis was 20.3%; in women 22.9% and in men 9.6%. Mean age increased from 46 years in participants presenting a T-score within the normal range to a mean age of 57 years in osteopenic participants and up to 63 years in osteoporotic participants. BMI average was declined from 27.6 kg/m2 in participants within a normal BMD T-score range to 23.8 kg/m2 in osteoporotic participants.
As osteoporosis was known before the fracture in 20 of 118 osteoporotic patients, the remaining 98 (13.3% of 738 patients) were unaware of having osteoporosis before investigated in OFELIA.
The prevalence of osteoporosis according to fracture location stratified for sex and age is shown in Figs. 2 and 3, respectively. In women, osteoporosis was present in ≥ 20% of the patients with fractures of the clavicle, shoulder/upper arm or fore-arm. In patients aged 50+ years, osteoporosis was found in > 30% of patients with fractures of hip/femur, and in ≥ 50% of patients with fractures of pelvis or the spine. Details of the fracture localization in men and women aged < 50/≥ 50 years divided by BMD T-score categories are shown in Table 3.
Table 4 shows crude and age-/sex-adjusted associations of having osteoporosis if being a woman versus a man, aged ≥ 50 versus < 50 years, having experienced a fracture earlier in life versus not having experienced a fracture, presenting a BMI below 20 versus a BMI at or above 20 kg/m2, being menopausal before the age of 46 years versus older, being a non-smoker versus former or current smoker, being alcohol abstinent versus different degrees of alcohol consumption. Independent of sex, a lower T-score was observed with higher age, and the risk of having osteoporosis was almost five times higher in individuals aged 50+ years than in individuals < 50 years [sex-adjusted OR 4.7 (2.5; 9.1)]. Among the 42% of the participants, who had experienced at least one previous fracture in adulthood, the risk of having osteoporosis was similar to the risk in those without a previous fracture [OR 1.3 (0.9; 2.0)]. Low BMI was associated with osteoporosis [5.7 (2.6; 12.4)] as was early menopause in women [OR 2.3 (1.3; 3.9)].
No associations were observed between smoking or alcohol consumption and osteoporosis.
Supplementary Table B shows non-significant associations between use of prednisolone, family history of osteoporosis, loss of height, and diseases previously demonstrated to be associated with fracture risk and osteoporosis.
Three years (± 6 month) after the fracture that led to participation in OFELIA, the 98 patients who had been diagnosed with osteoporosis in OFELIA were contacted again. A total of 93 patients could be reached. All patients and their GPs had been given recommendation to start anti-osteoporosis treatment. Seventy-five (81%) of the patients had started anti-osteoporosis treatment. Weekly alendronate was the chosen treatment in 90% of the patients starting treatment. Three years after the fracture 71 of the 75 patients (95%) who started treatment are still adherent and compliant with the treatment. Eighty-five percent of the patients diagnosed with osteoporosis are taking calcium and vitamin D supplementation on daily basis.
Despite treatment compliance, 6 of 71 patients (8%) receiving anti-osteoporosis treatment experienced a (minor) subsequent fracture in the follow-up period. Four of these six had had increasing BMD by DXA 2 years after initiation of treatment. In the group of 18 patients who did not receive anti-osteoporosis treatment, four patients (22%) experienced a new fracture at follow-up. DXA has been repeated in 55 patients. BMD was improved in 49 (89.1%), unchanged in one (1.8%) and reduced in 5 (9.1%). Of the five patients who had lost BMD, four had not initiated anti-osteoporosis treatment.
Discussion
We estimated the prevalence of osteoporosis and investigated clinical risk factors for osteoporosis in a population of male and female fracture patients between 18 and 93 years presenting numerous fracture locations following a low-energy trauma except fractures at skull and face (excluded) and ribs. A few patients with rib fractures were approached but declined participation. In OFELIA, osteoporosis was present in more than one in seven patients, and in more than one in eight patients the diagnosis was previously unknown. In patients aged 50+ years, osteoporosis was observed in one in five patients.
The prevalence of osteoporosis in OFELIA was considerably lower than the prevalence seen in The West Glasgow FLS-cohort [20]. Assuming that the OFELIA cohort is representative for the Danish and perhaps even Nordic populations with limitations as argued above, the socioeconomic benefits of FLS based on the Glasgow model may be challenged in a Danish/Nordic context. In this very first FLS-cohort investigated in Glasgow 15 years ago including (n = 734) men and women aged 50+ years with any low-trauma fractures except skull and facial, the prevalence of osteoporosis was 46.7% (32.5% in men and 49.5% in women) [20]. The difference in osteoporosis prevalence between the West Glasgow FLS and the present study may be explained by several factors. First of all, the recruitment strategies were different. In West Glasgow FLS, hip-fractures comprised 9.3% of the cohort, whereas as in the present study, only 5.2% of the patients had hip-fractures. Based on the strong associations between osteoporosis and high age, hip-fractures and female gender, it can be assumed that the ten patients (five men and five women), six of them being 70+ years with hip-fractures, who refused participation would have increased the prevalence of osteoporosis in our study, had they been investigated. Secondly, the socio-economic background and level of education of the Glasgow and Aarhus populations may differ [31]. Thirdly, general knowledge about bone health and the importance of sufficient intake of calcium and vitamin D has improved over the 15 years since the patients were recruited into the Glasgow FLS [32], and the fracture rate has been decreasing [33]. The importance of the latter two explanations is underscored by the findings of a recent study by Clunie and Stephenson investigating fracture patients above the age of 45 years and found osteoporosis to be present in 18% of patients [34].
In the present study, we only diagnosed osteoporosis based on BMD T-scores. In daily clinical practice, fractures of the hip and spine after low-energy traumas are also used to diagnose osteoporosis even with BMD in the osteopenic or normal ranges. Some participants, who were categorized in OFELIA as not having osteoporosis, therefore had a previous osteoporosis diagnosis and had received anti-osteoporotic treatment or were diagnosed with osteoporosis due to the incident fracture. As we only classified participants with T-scores ≤ − 2.5 in hip or spine as osteoporotic in this study, we most likely have underestimated the prevalence of clinically relevant osteoporosis.As the time span from fracture to DXA was relatively short, and as all patients were mobilized at the time of DXA, we suggest that bone loss as a result of immobilization in relation to the fracture is reflected in the BMD measured by DXA in OFELIA.
Only one out of three fracture patients had normal BMD. The lack of care for fracture patients is highlighted by the fact that 42% of the patients have had a previous fracture, but only few of these patients have had a DXA performed because of the fracture. Our findings are in accordance with findings from both Canada [35] and a fracture cohort from Australia [28], where approximately half of the fracture patients had already suffered a previous low-energy fracture. Participants in OFELIA with a history of fracture had a higher risk of having osteopenia or osteoporosis than patients without previous fractures. We also observed that the majority of fractures in OFELIA occurred in patients with osteopenia (48.9%), which is in agreement with previous studies [6, 36,37,38]. This is a challenge for secondary prevention programs as these patients will not be offered secondary prevention in the form of medical treatment according to guidelines which suggest treatment to patients with osteoporosis, whereas at least some of these patients would be offered treatment if guidelines based on absolute fracture risk are used.
In both men and women, osteoporosis was found in more than 30%, if the fracture was located at pelvic, hip, or spine. Furthermore, in women, fractures of the clavicle, shoulder/upper arm, and fore-arm were also associated with the presence of osteoporosis. Löffman et al. [36] found a similar strong association between osteoporosis and fractures at spine, hip, or shoulder/upper arm in their study of 303 Norwegian women aged 55–75 years, and osteoporosis was observed in one-third of patients with forearm fracture.
Even though certain fracture sites (e.g., forearm, shoulder and hip) are recognized as ‘osteoporotic fractures’ we did see clinically relevant prevalence of osteoporosis in patients with other fracture locations as e.g., pelvis (Figs. 2, 4). This finding is supported by a study from the UK [34] where Clunie and Stephenson advocate that osteoporosis in a substantial minority of patients can present with fractures at other sites. They investigated 1014 fracture patients aged 45–70 years over a period of 2 years and found osteoporosis prevalence in relation to specific fracture localizations similar to our findings in OFELIA.
Early menopause was associated with osteoporosis in the present study. This is in line with a population-based observational study from Sweden, where early menopause was found to be associated with risk of osteoporosis, fractures and increased mortality [39]. It is well-known that the incidence of fractures in women rises rapidly after the menopause because of the increased bone turnover and the rapid bone loss seen after menopause [40]. In the case of early menopause, a longer period of a woman’s lifespan is with low BMD compared to women who enter menopause at the normal age. Low body weight is a well-known risk factor for osteoporosis [41, 42] and in OFELIA, BMI < 20 kg/m2 was strongly associated with osteoporosis. We observed no association between previously identified risk factors such as tobacco, alcohol and treatment with prednisolone and osteoporosis. As all the participants in the present study had suffered one or more fractures they might constitute a different population than the general populations used for establishing the clinical risk factors for osteoporosis and/or fractures in international guidelines [43]. Information about smoking status, alcohol consumption, use of prednisolone etc. was retrospectively self-reported and might be affected by recall-bias most often leading to underestimate real use of cigarettes and alcohol. All questions were answered by the participants before knowing the outcome of the DXA. Therefore, any misclassification is most likely of non-differential nature, resulting in bias towards the null. The response rate was high, which may be a result of the procedure by which the questionnaires were collected as described in methods.
We explored information on gender, age and fracture localisation in approached eligible non-participants at all stages of the enrolment procedure. As mentioned, the number of hip-fractures among non-participants was higher than in the OFELIA cohort and the prevalence of osteoporosis found in this study is probably an underestimation of the true osteoporosis prevalence among fracture patients due to the difficulties associated with enrolling more fragile patients such as patients with hip or spine fractures or patients with severe comorbidity. As shown in Supplementary Table B, the comorbidity in participants was relatively low, and patients refusing enrolment often mentioned comorbidity and lack of surplus as reasons for not attending to OFELIA. These difficulties were not unique for participants in OFELIA, where 41% (31 of 76) identified and eligible hip-fracture patients refused investigation. A recent Dutch study by Eekman et al. [44] found that the overall response rate to more than 2200 invitations to participate in FLS at four hospitals was 51% and that patients with a hip-fracture responded less frequently (29%)., Therefore, when implementing a future prevention program, this non-participating group of patients underscores that, there is a need for organizing special offers of investigation/intervention in the group of fragile older patients with high risk of having osteoporosis who are unable to show up for a DXA.
The present study is among the first studies to investigate the prevalence of osteoporosis and fracture location in adult male and female patients as young as 18 years. We observed a strong association between increasing age and osteoporosis, however, 11 participants in OFELIA (four men and seven women) under the age of 50 years had osteoporosis, and more than 40% of patients below the age of 30 years had abnormal BMD. The diagnosis and treatment of osteoporosis in younger patients are complex and controversial [45], and although specific anti-osteoporotic treatment would not be recommended in these patients, they may benefit from general advice regarding bone healthy lifestyle and a plan for a follow-up evaluation in due time. When FLS traditionally investigates fracture patients aged 50+ years, a potential care gap still remains of reducing the risk of subsequent fractures among this subgroup of younger fracture patients; however, a significant knowledge gap still exists when it comes to understanding the risk of future fractures in younger fracture patients.
A recent meta-analysis has found that the fracture risk increases by approximately 30% with non-compliance to therapy for osteoporosis [46]. In OFELIA more than 4 of 5 (81%) patients diagnosed with osteoporosis initiated anti-osteoporosis treatment and 95% of those initiating treatment were still adherent and compliant 3 years later. An overall treatment up-take and adherence over 3 years of 76% demonstrates that implementation of FLS will reduce the future fracture burden in patients presenting with fragility fracture. In OFELIA the fraction of patients treated is higher compared to other reports. A meta-analysis of adherence to drug therapy for osteoporosis concluded that one-third to half of patients did not take their medication as directed [47]. Similarly, a French epidemiological study including 785 women (51.5% with a history of fracture) found 65% adherence to treatment [48] and suggested that being well-informed of osteoporosis since diagnosis were significantly associated with compliance. In OFELIA all patients had suffered a fracture which may motivate them to comply with fracture prevention. In addition, as participants in OFELIA they had an in-depth conversation about the link between fractures and bone health, and at the time for diagnosis they had a new informative conversation about osteoporosis which may also have improved the up-take and adherence to treatment.
The study has strengths and limitations. We investigated a large number of male and female fracture patients presenting a wide range of age and different localisations of fractures. In addition, the inclusion of patients was performed over a full year, including all four seasons which, in Denmark, include a rainy, slippery autumn and a cold winter with snow and iced roads and pavements. BMD, weight and height were measured by trained technicians and, in combination with sex and age, with negligible numbers of missing data.
The enrolment procedure depended on the willingness of the health-professionals to ask patients for permission to be contacted by the study coordinator. The study coordinator repeatedly informed and stressed the importance of avoiding subjective selection of patients for the study due to any “sense of the patient’s risk of having osteoporosis”. Approximately, one-fourth of fracture patients treated at AUH were approached by the health-professionals to provide information about the study. When exploring the registration of all approached fracture patients in the OFELIA log-book we recognized an overall tendency that recruitment of eligible patients was mostly based on the enthusiasm of the individual health professional at work and not upon the health care professional assumption regarding the likelihood of the patient having osteoporosis or not. This could lead us to suggest, that the OFELIA cohort represented a non-selected group of fracture patients. However, according to fracture localisation, the percentage of hip-fractures in OFELIA was lower than in the approached non-participating group of fracture patients as well as in the patients identified in the register at AUH. Thus, to assess the generalisability of the study population in OFELIA to the overall Danish fracture population, we need to take selection bias and the differences in the distribution of fractures in patients being investigated compared to patients not investigated into account.
The participants and the non-participants differed in age, sex and fracture localisation—especially hip-fractures—which may have caused selection bias. The older (women) with hip-fractures expected to be at high risk of osteoporosis and the younger men expected to be at low risk declined participating in the study. A perception of osteoporosis as an “old-woman disease” could be the reason behind the younger men’s relatively higher rate as non-participates, but despite reasons behind, the young men’s’ absence might have overestimated the prevalence of osteoporosis in OFELIA. On the other hand, the prevalence estimate could also be underestimated given the high proportion of older hip-fracture patients among the group of non-participants due to co-morbidities and lack of surplus. We assume that a study population comprising relatively less patients with hip or spine fractures might cause an underestimation of the prevalence of osteoporosis.
The OFELIA study demonstrated that osteoporosis was present in more than one in five fragility fracture patients ≥ 50 years, that nearly half of the fracture patients had suffered a fracture previously, and that the vast majority of patients was unaware of osteoporosis prior to the fracture and is unlikely to be investigated for osteoporosis by the current non-systematic approach to fracture patients. Furthermore, the up-take and adherence to anti-osteoporosis treatment are high in patients being diagnosed with osteoporosis after a fracture. We therefore suggest that a considerable group of fracture patients will benefit from a systematic approach to reduce the risk of subsequent fractures in Denmark. We also suggest implementing an individualized approach to the most fragile and older fracture patients.
References
[Anonymous] (1993) Consensus development conference: diagnosis, prophylaxis, and treatment of osteoporosis. Am J Med 94:646–650
Center J, Eisman J (1997) The epidemiology and pathogenesis of osteoporosis. Baillière’s Clin Endocrinol Metab 11:23–62
Kanis JA (2002) Diagnosis of osteoporosis and assessment of fracture risk. Lancet 359:1929–1936
Ganda K, Puech M, Chen JS, Speerin R, Bleasel J, Center JR, Eisman JA, March L, Seibel MJ (2013) Models of care for the secondary prevention of osteoporotic fractures: a systematic review and meta-analysis. Osteoporos Int 24:393–406
McLellan AR, Wolowacz SE, Zimovetz EA, Beard SM, Lock S, McCrink L, Adekunle F, Roberts D (2011) Fracture liaison services for the evaluation and management of patients with osteoporotic fracture: a cost-effectiveness evaluation based on data collected over 8 years of service provision (structured abstract). Osteoporos Int 22:2083–2098
Mehrpour SR, Aghamirsalim MR, Sorbi R (2012) Are hospitalized patients with fragile fractures managed properly in relation to underlying osteoporosis? J Clin Rheumatol 18:122–124
Elliot-Gibson V, Bogoch ER, Jamal SA, Beaton DE (2004) Practice patterns in the diagnosis and treatment of osteoporosis after a fragility fracture: a systematic review. Osteoporos Int 15:767–778
Giangregorio L, Papaioannou A, Cranney A, Zytaruk N, Adachi JD (2006) Fragility fractures and the osteoporosis care gap: an international phenomenon. Semin Arthritis Rheum 35:293–305
McCloskey EV, Harvey NC, Kanis JA (2015) Can we treat to target in osteoporosis?. Int J Clin Rheumatol 10:01
Boonen S, Reginster J, Kaufman J, Lippuner K, Zanchetta J, Langdahl B, Rizzoli R, Lipschitz S, Dimai HP, Witvrouw R, Eriksen E, Brixen K, Russo L, Claessens F, Papanastasiou P, Antunez O, Su G, Bucci-Rechtweg C, Hruska J, Incera E, Vanderschueren D, Orwoll E (2012) Fracture risk and zoledronic acid therapy in men with osteoporosis. N Engl J Med 367:1714–1723
Cummings SR, Martin JS, McClung MR, Siris ES, Eastell R, Reid IR, Delmas P, Zoog HB, Austin M, Wang A, Kutilek S, Adami S, Zanchetta J, Libanati C, Siddhanti S, Christiansen C (2009) Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med 361:756–765
Black DM, Delmas PD, Eastell R, Reid IR, Boonen S, Cauley JA, Cosman F, Lakatos P, Leung PC, Man Z, Mautalen C, Mesenbrink P, Hu H, Caminis J, Tong K, Rosario-Jansen T, Krasnow J, Hue TF, Sellmeyer D, Eriksen EF, Cummings SR (2007) Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med 356:1809–1822
Neer RM, Arnaud CD, Zanchetta JR, Prince R, Gaich GA, Reginster J, Hodsman AB, Eriksen EF, Ish-Shalom S, Genant HK, Wang O, Mellström D, Oefjord ES, Marcinowska-Suchowierska E, Salmi J, Mulder H, Halse J, Sawicki AZ, Mitlak BH (2001) Effect of parathyroid hormone (1–34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med 344:1434–1441
Black DM, Cummings SR, Karpf DB, Cauley JA, Thompson DE, Nevitt MC, Bauer DC, Genant HK, Haskell WL, Marcus R, Ott SM, Torner JC, Quandt SA, Reiss TF, Ensrud KE (1996) Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Lancet 348:1535–1541
Langdahl BL, Silverman S, Fujiwara S, Saag K, Napoli N, Soen S, Enomoto H, Melby TE, Disch DP, Marin F, Krege JH (2018) Real-world effectiveness of teriparatide on fracture reduction in patients with osteoporosis and comorbidities or risk factors for fractures: integrated analysis of 4 prospective observational studies. Bone 116:58–66
Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA, Berger M (2000) Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res 15:721–739
Kanis JA, Johnell O, De Laet C, Johansson H, Oden A, Delmas P, Eisman J, Fujiwara S, Garnero P, Kroger H, McCloskey EV, Mellstrom D, Melton LJ, Pols H, Reeve J, Silman A, Tenenhouse A (2004) A meta-analysis of previous fracture and subsequent fracture risk. Bone 35:375–382
Wu C-, Kao I-, Hung W-, Lin S-, Liu H-, Hsieh M-, Bagga S, Achra M, Cheng T, Yang R (2018) Economic impact and cost-effectiveness of fracture liaison services: a systematic review of the literature. Osteoporos Int 29:1227–1242
Marsh D, Åkesson K, Beaton DE, Bogoch ER, Boonen S, Brandi M-, McLellan AR, Mitchell PJ, Sale JEM, Wahl DA (2011) Coordinator-based systems for secondary prevention in fragility fracture patients. Osteoporos Int 22:2051–2065
McLellan AR, Gallacher SJ, Fraser M, McQuillian C (2003) The fracture liaison service: success of a program for the evaluation and management of patients with osteoporotic fracture. Osteoporos Int 14:1028–1034
United Kingdom, National Osteoporosis Society. http://www.nos.org.uk. Accessed 31 Aug 2018
van Geel TACM, Bliuc D, Geusens PPM, Center JR, Dinant G, Tran T, van den Bergh JPW, McLellan AR, Eisman JA (2018) Reduced mortality and subsequent fracture risk associated with oral bisphosphonate recommendation in a fracture liaison service setting: a prospective cohort study. PLoS ONE 13(6):e0198006
Mitchell PJ (2013) Best practices in secondary fracture prevention: fracture liaison services. Curr Osteoporos Rep 11:52–60
Åkesson K, Marsh D, Mitchell PJ, McLellan AR, Stenmark J, Pierroz DD, Kyer C, Cooper C (2013) Capture the fracture: a best practice framework and global campaign to break the fragility fracture cycle. Osteoporos Int 24:2135–2152
Leslie WD, Giangregorio LM, Yogendran M, Azimaee M, Morin S, Metge C, Caetano P, Lix LM (2012) A population-based analysis of the post-fracture care gap 1996–2008: the situation is not improving. Osteoporos Int 23(5):1623–1629
Eisman JA, Bogoch ER, Dell R, Harrington JT, McKinney RE, McLellan A, Mitchell PJ, Silverman S, Singleton R, Siris E (2012) Making the first fracture the last fracture: ASBMR task force report on secondary fracture prevention. J Bone Miner Res 27:2039–2046
Hansen L, Petersen KD, Eriksen SA, Langdahl BL, Eiken PA, Brixen K, Abrahamsen B, Jensen JB, Harsløf T, Vestergaard P (2015) Subsequent fracture rates in a nationwide population-based cohort study with a 10-year perspective. Osteoporos Int 26(2):513–519
Bliuc D, Ong CR, Eisman JA, Center JR (2005) Barriers to effective management of osteoporosis in moderate and minimal trauma fractures: a prospective study. Osteoporos Int 16:977–982
Kanis JA, McCloskey EV, Harvey NC, Johansson H, Leslie WD (2015) Intervention thresholds and the diagnosis of osteoporosis. J Bone Miner Res 30:1747–1753
Fracture risk assessment tool FRAX. http://www.shef.ac.uk/FRAX. Accessed 31 Aug 2018
Vestergaard P, Rejnmark L, Mosekilde L (2006) Socioeconomic aspects of fractures within universal public healthcare: a nationwide case-control study from Denmark. Scand J Public Health 34:371–377
Pedersen MA, Gregersen M, Langdahl BL, Damsgaard EMS (2014) Frail elderly hip fracture patients and vitamin D. J Gerontol Geriatr Res 3(5):180
Abrahamsen B, Vestergaard P (2010) Declining incidence of hip fractures and the extent of use of anti-osteoporotic therapy in Denmark 1997–2006. Osteoporos Int 21:373–380
Clunie G, Stephenson S (2008) Implementing and running a fracture liaison service: an integrated clinical service providing a comprehensive bone health assessment at the point of fracture management. J Orthop Nurs 12:159–165
Osteoporosis Canada. http://www.osteoporosis.ca. Accessed 31 Aug 2018
Löffman O, Hallberg I, Berglund K, Wahlström O, Kartous L, Rosenqvist AM, Larsson L, Toss G (2007) Women with low-energy fracture should be investigated for osteoporosis. Acta Orthop 78:813–821
Åstrand J, Thorngren KG, Tägil M (2006) One fracture is enough!: experience with a prospective and consecutive osteoporosis screening program with 239 fracture patients. Acta Orthop 77:3–8
Siris ES, Miller PD, Barrett-Connor E, Faulkner KG, Wehren LE, Abbott TA, Berger ML, Santora AC, Sherwood LM (2001) Identification and fracture outcomes of undiagnosed low bone mineral density in postmenopausal women: results from the national osteoporosis risk assessment. JAMA 286:2815–2822
Svejme O, Ahlborg H, Nilsson J, Karlsson M (2012) Early menopause and risk of osteoporosis, fracture and mortality: a 34-year prospective observational study in 390 women. BJOG: Int J Obstet Gynaecol 119:810–816
Cummings SR, Melton LJ (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet 359:1761–1767
Sambrook P, Cooper C (2006) Osteoporosis. Lancet 367:2010–2018
De Laet C, Kanis JA, Odén A, Johanson H, Johnell O, Delmas P, Eisman JA, Kroger H, Fujiwara S, Garnero P, McCloskey EV, Mellstrom D, Melton LJ 3rd, Meunier PJ, Pols HAP, Reeve J, Silman A, Tenenhouse A (2005) Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int 16:1330–1338
Kanis JA, Hans D, Cooper C, Baim S, Bilezikian JP, Binkley N, Cauley JA, Compston JE, Dawson-Hughes B, El-Hajj Fuleihan G, Johansson H, Leslie WD, Lewiecki EM, Luckey M, Oden A, Papapoulos SE, Poiana C, Rizzoli R, Wahl DA, McCloskey EV (2011) Interpretation and use of FRAX in clinical practice. Osteoporos Int 22:2395–2411
Eekman DA, van Helden SH, Huisman AM, Verhaar HJJ, Bultink IEM, Geusens PP, Lips P, Lems WF (2014) Optimizing fracture prevention: the fracture liaison service, an observational study. Osteoporos Int 25:701–709
Langdahl BL (2017) Osteoporosis in premenopausal women. Curr Opin Rheumatol 29:410–415
Ross S, Samuels E, Gairy K, Iqbal S, Badamgarav E, Siris E (2011) A meta-analysis of osteoporotic fracture risk with medication nonadherence. Value Health 14:571–581
Kothawala P, Badamgarav E, Ryu S, Miller RM, Halbert RJ (2007) Systematic review and meta-analysis of real-world adherence to drug therapy for osteoporosis. Mayo Clin Proc 82:1493–1501
Huas D, Debiais F, Blotman F, Cortet B, Mercier F, Rousseaux C, Berger V, Gaudin A, Cotté F (2010) Compliance and treatment satisfaction of post menopausal women treated for osteoporosis. Compliance with osteoporosis treatment. BMC Womens Health 10:26
Acknowledgements
We wish to express our gratitude to all participants in OFELIA for their willingness to make this study possible. To our colleagues at the Department of orthopedic surgery (E) and the Department emergency and acute medicine (FAA) at Aarhus University Hospital (AUH) for identifying fracture patients for this study. Also, many thanks to the staff at The Osteoporosis Clinic, AUH for their great work performing the DXAs.
Funding
For financial support, we wish to thank the Health Research Fund of Central Denmark Region, Aarhus University Hospital (“Spydspidspuljen”), Department of Endocrinology and Internal Medicine (MEA), AUH and the Danish Osteoporosis Society.
Author information
Authors and Affiliations
Contributions
Study design and conduct: RT, BL and OB. Data collection: RT. Data analysis and interpretation: RT, CR, OR, OB and BL. Drafting manuscript: RT and BL. Revising manuscript content: CR, OR and OB. Approving final version of manuscript: RT, CH, OR, OB and BL. RT takes responsibility for the integrity of the data analysis, has full control of all primary data and agrees to allow the journal to review data if requested.
Corresponding author
Ethics declarations
Conflict of interest
Bente L. Langdahl has received honoraria for consulting and lecturing for Amgen, Merck, UCB, and TEVA and received research grants from Amgen and Novo Nordisk. Randi M. H. Tei, Cecilia H. Ramlau-Hansen, Oleguer Plana-Ripoll, Ole Brink have no conflicts of interests.
Ethical Approval
The study complies with the principles outlined in the Declaration of Helsinki. The study was approved by the Danish Data Protection Agency.
Informed Consent
All informants were informed that they could withdraw their participation at any time before or during the interview without any consequences for their further fracture treatment and follow-up. The study was approved by the Danish Data Protection Agency (J. No. 2007-58-0016). We submitted the protocol to review by the Central Denmark Region Committees on Health Research Ethics, but they found that the study procedures were in accordance to the Danish osteoporosis guidelines and non-interventional. Therefore, the study did not need formal ethical approval and did not need informant consent. Nevertheless, in agreement with good clinical practice we collected informed written consent from all participants.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tei, R.M.H., Ramlau-Hansen, C.H., Plana-Ripoll, O. et al. OFELIA: Prevalence of Osteoporosis in Fragility Fracture Patients. Calcif Tissue Int 104, 102–114 (2019). https://doi.org/10.1007/s00223-018-0476-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-018-0476-3