Abstract
Osteogenesis imperfecta (OI) is a systemic connective tissue disorder most often caused by mutations in collagen type 1 related genes. Patients with OI suffer from multiple fractures and various degrees of growth deficiency and bone deformity. It is unknown whether the systemic effect of defect collagen type 1 influences the quality of life in patients with OI. We therefore aimed to investigate health-related quality of life (HRQoL) in a well-characterized cohort of adult patients with OI. We included 85 adult patients with mild to severe OI (types I, III, and IV) and obtained information about skeletal- and non-skeletal phenotypes and patient demographics. We investigated physical and mental HRQoL using a validated questionnaire, SF-36, and compared the data to values obtained in a population without OI. Patients with mild, moderate, and severe OI all had lower mean scores on domains describing physical HRQoL and a lower mean physical component score compared to the general population, p < 0.001. Patients with severe OI had lower mean scores on physical HRQoL, p < 0.05. The scores on domains reflecting mental HRQoL were more inhomogenously affected, but did not differ significantly from the general population. OI has an impact on physical and some aspects of mental HRQoL. The scores on physical health were correlated to severity of the OI disease. The mental component score in the OI patients was unaffected and comparable with the general population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteogenesis imperfecta (OI) is a rare hereditary disorder of the connective tissue leading to fractures and a wide range of other physical signs and symptoms that include pre-senile hearing loss, dental abnormalities, blue sclera, growth deficiency, bone deformities, and hypermobility [1–3]. The clinical severity ranges from perinatal lethality to early onset osteoporosis as described in the Sillence classification (originally 1979, updated in 2014) [2, 4]. Fractures are frequent in childhood but the incidence decreases in early adulthood and increases again with increasing age, mimicking age-related osteoporosis [3, 5, 6]. Other symptoms increase in severity with age, e.g., hearing impairment and physical restrictions due to pain, progressively deforming bones or hypermobility [7–9]. Due to these different disabilities, health-related quality of life (HRQoL) may be affected in OI and the potential impact of skeletal as well as non-skeletal phenotypes may also vary significantly depending on OI type and age [10, 11].
HRQoL consigns to the perception of disease and its influence on physical and mental well-being [12]. The effect of OI on HRQoL in adults has been very sparsely investigated [10, 13, 14]. Thus, a recent systematic review [15] included only three studies involving adults with OI [10, 13, 16] as well as one study focusing on the impact of having a severely affected child with OI in the family [17]. The three studies investigating QoL in OI included less than 30 patients and did not consistently include patients with OI type I, III, and IV. Knowledge about how OI affects HRQoL may provide the grounds for focusing treatment and support to the needs of the patients in this disorder that can only be treated symptomatically [18]. The aim of the present study therefore was to assess HRQoL in a large cohort of clinically well-characterized adult Danish OI patients (OI type I, III, and IV) and compare the outcome to HRQoL in the general Danish population. We tested the hypothesis that there was no difference between HRQoL in OI patients compared to healthy controls. Secondly, we aimed to investigate whether specific OI symptoms affect HRQoL, in order to increase awareness of these symptoms in the management of patients with OI.
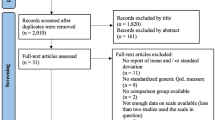
Materials and Methods
Study Population
The study population consists of 85 adult OI patients as described previously [19]. One patient died before the end of the study and is not included in this study.
Health-Related Quality of Life Measure
HRQoL was assessed by SF-36 version 1 [20]. This is a validated multidimensional measure of QoL consisting of 36 questions in eight sub domains, four physical domains and four mental domains. The physical domains include physical functioning (PF), limitations in the everyday life due to physical health problems or physical role limitations (RP), bodily pain (BP), and perception of general health (GH). The mental domains include: vitality (VT), social functioning (SF), role limitations due to emotional problems (RE), and perception of mental health (MH). Within each domain the score ranges from 0 to 100, with a higher score reflecting a better self-reported HRQoL. In accordance with Ware et al. physical and mental domains were combined into the Physical Component Summary (PCS) and Mental Component Summary (MCS) [21]. Ware et al. described this method and reported validated values of PCS and MCS originating from investigations of the general American population [21]. Bjorn et al. investigated this in a large Danish cohort of healthy adults and these data were used for comparison in this study [22, 23].
Medical History and Clinical Assessments
All patients underwent a systematic interview and clinical examination [19]. Information was collected about educational status (no high school, high school, basic training, under graduate, graduate) and family predisposition. Anthropometric markers included body height (without shoes, by wall mounted stadiometer when possible, alternatively measuring tape), weight (lightly clothed without shoes), sitting height (1 m ruler), arm span (by wall mounted scale), and head circumference (measuring tape). General signs of OI included scleral color (white/colored), number of self-reported previous fractures, self-reported hypermobility (e.g., if the patient had sprain problems), self-reported daily pain, and degree of mobility (normal, assisted, or wheelchair). All patients were invited to undergo clinical and radiographic dental examinations for the diagnosis of dentinogenesis imperfecta (DI), audiologic evaluations by an audiologist, and ophthalmologic investigations to assess hearing loss and visual impairment, respectively (manuscript in preparation). The original Sillence classification was applied to all patients as mild (OI type I), moderate (OI type IV), or severe (OI type III) [2]. OI severity was defined as OI type graded by severity.
Statistics
All parameters were tested for normal distribution by histograms and q–q plots. Normally distributed data were compared between groups using analysis of variance (ANOVA) and data not normally distributed were tested using non-parametric tests. The numbers of fractures were normally distributed after log transformation. Comparison between the patients and normative data was done with one-sample t test or one-sample Wilcoxon Signed-Rank test as appropriate. Simple linear regression was performed to investigate the influence of specific variables (OI severity, age, educational level, fracture within 24 months) on PCS and MCS, and R 2-values and p-values were reported accordingly. Validity was evaluated by scatter plots and investigations of residuals. The significance level was p < 0.05. Statistical analyses were performed using SPSS version 20.0 (Chicago, IL).
Results
Baseline and clinical characteristics of this cohort are reported in Table 1. Mean age was 45 [18–78] years. In this cohort 92% had colored sclera, 52% had impaired hearing, 25% suffered from dentinogenesis imperfecta (DI), 65% suffered from hypermobility, 77% were independent walkers, and 12 and 11% were wheelchair users and assisted walkers, respectively. Pain was reported by 49, and 24% of the cohort had suffered a fracture within 24 months. Sixty-nine percent had family members with OI. Nine percent of the cohort had stopped school before high school; in 5% high school was the highest education. The remaining had an education of basic training (37%), undergraduate (30%), or graduate-level (19%). One patient in the cohort did not work due to mental issues. No patients reported previous hospitalization in a psychiatric department.
Table 2 shows the results of the 8 SF-36 domains and the 2 summary component scores of the 84 OI adults. In the four physical domains the mean for all three types of OI was significantly below the mean of the general Danish population (p < 0.01 for all). Thus, physical function (PF) was 72.8 ± 26.4 (mean ± SD), 20.9 ± 21.5, and 64.7 ± 30.4 for OI type I, III, and IV, respectively versus 88.2 ± 19.8 in the general Danish population. The same pattern of differences was seen in the remaining three domains. Using ANOVA the three OI types only differed significantly with respect to PF (p < 0.05) where the score for OI type III was significantly lower than for OI type I and IV (p < 0.001). Regarding the physical component score (PCS) the pattern was the same. All OI types had significantly lower PCS scores than the general Danish population (40.5 ± 11.5, 30.5 ± 9.4, and 39.2 ± 11.5 for OI type I, III, and IV, respectively vs. 51.2 ± 8.8 in the general Danish population, p < 0.01) and using ANOVA the three OI types differed significantly (p < 0.05) with the score for OI type III being significantly lower than that for OI type I and IV (p < 0.05), Fig. 1.
Linear regression analysis showed that increased age (R 2 = 0.10, p = 0.003) and increased OI severity (R 2 = 0.07, p = 0.015) were significantly correlated with a lower PCS. PCS did not correlate with educational level (0.3) or fracture within 24 months (p = 0.5).
The four mental domains are depicted in Table 2. The scores reflecting vitality (VT), social function (SF), and role limitations due to mental health (RE) were generally lower than in the general Danish population. VT scores were significantly reduced in patients with OI type I compared to the general Danish population (p = 0.02), whereas SF was reduced in patients with OI type I, III, and IV compared to the general Danish population (p < 0.001, p = 0.043, and p = 0.042, respectively). The RE scores were significantly reduced in patients with OI type I and IV compared to the general Danish population (p < 0.001 and p = 0.024, respectively). The mental health (MH) scores were 79.9 ± 15.9, 82.2 ± 10.3, 78.9 ± 21.5, and 81.8 ± 15.5 for OI type I, III, and IV and the general Danish population, respectively. There were no differences between any OI type and the general Danish population or between OI types (p > 0.05 for all). The mean mental component score (MCS) was 52.7 ± 10.3, 60.6 ± 8.7, and 53.0 ± 12.5 for OI type I, III, and IV, respectively versus 54.0 ± 8.4 in the general Danish population. In this case the score was in fact significantly higher in OI type III compared to the general Danish population (p < 0.05) whereas there was no difference between OI types.
Linear regression analysis showed that lower MCS was significantly correlated with lower educational level (R 2 = 0.099, p = 0.006), but MCS did not correlate significantly with OI severity (p = 0.05), age (p = 0.5), or a fracture within 24 months (p = 0.2).
Discussion
In the present study, we evaluated health-related quality of life in a large group of adult patients with OI and which factors affect HRqOL. Our study showed that OI affected HRQoL with a considerable effect on physical and to a smaller degree also on mental health. QoL in adult OI has previously been sparsely investigated. Three other studies investigated the topic in smaller cohorts within the last two decades.
In a cross-sectional setting Widmann et al. [13] investigated QoL in 30 adults with OI categorized by the presence of fractures before or after birth using SF-36. They found impaired physical health compared to the American general population, and lower values in patients characterized by having suffered fractures prenatally compared to the patients less severely affected. Mental health was comparable to the American general population.
Another study by Widmann et al. showed that the degree of scoliosis and thereby decreased vital capacity reduced the physical but not the mental QoL using SF-36 [16].
In a prospective, cross-sectional study Balkefors et al. [10] investigated quality of life (by SF-36) and life satisfaction (questionnaires) in 29 adults with mild to moderate OI and concluded that despite preserved physical mobility the physical HRQoL was reduced but the life satisfaction was high.
In the present study, OI patients reported lower scores than the general Danish population in all of the four physical health domains of SF-36 and in the PCS. This reflects a debilitating disease where every day physical exercises such as running, walking, or climbing stairs are significantly impaired and obvious limitations due to physical disease are present. Even in OI patients who are less affected by physical disabilities, a disease like OI may affect physical behavior. It is possible that OI patients, as time goes by, adapt by being more careful and thereby less physically active compared to individuals without bone fragility.
Three of the four mental domains were also significantly affected, though to a smaller extent and with a greater variation than the four physical domains. Vitality (VT) and social function (SF) were significantly reduced, as were limitations due to mental health (RE). The combined score describing the general mental health (MCS), however, was not affected compared with the general population. Patients with OI type III even had significantly higher values. In general, there is a weak positive correlation between physical and mental SF-36 scales. In the calculation of PCS and MCS the correlation between the two components is 0 [22]. This compensation is introduced by adding a small negative weight to physical scales in the calculation of MCS. This means that very low physical SF-36 scores (as in OI type III) will generate a higher MCS than expected from the mental SF-36 scale result. This may explain at least part of the high MCS in patients with OI type III. However, none of the mental scale results in OI type III are numerically below the respective results in OI type I or IV, indicating a preserved mental health-related quality of life in these most severely affected patients. This corresponds well with previous descriptions of OI patients [24, 25]. Studies debate whether patients sustaining years of medical challenges develop a certain behavioral phenotype. In interviews including 55 adult patients with OI, the adults are described as endurable and very resilient with a possible environmental component due to the excessive physical challenges early in life [24]. However, observations of children with OI also describe a surprisingly unaffected emotionality [25]. In the context of describing quality of life in an adult population with OI it is important to note, that SF-36 is a general questionnaire that does not take a specific disease-related issues into account.
A higher level of education was significantly associated with better MCS. A higher educational level is in general an important trait that affects mental HRQoL in a positive direction as described in several other conditions [26–29]. We speculate that OI patients as well as others with the capabilities to educate and work are generally more satisfied in life and less affected by physical challenges. If a patient due to a disease is unable to begin and complete an education and get a job, that patient will constantly be reminded of the underlying disease and how it affects life in general.
The general impression of good quality of life implies with being in good health. Does this imply that patients with physical disabilities like OI can be considered in bad health and unable to possess a high level of subjective well-being and life satisfaction? This study clearly opposes this notion. A pattern similar to what we describe here is found in HRQoL studies in other conditions with inborn impaired physical health, such as cerebral palsy. Here physical health parameters are also decreased, with no effects on the mental parameters [30]. Moreover, it has been described that in congenital heart disease, children at a young age are challenged to develop a sense of coherency caused by extreme experiences derived by the disease [31]. We speculate whether this could reflect an adaptation to the limitations of a congenital disease and lifelong symptoms. Such experiences may affect individuals, also in adulthood [24]. Previous studies debate the paradox of good quality of life despite physical disabilities, and conclude that quality of life is just as much a matter of balance of body and mind, and abilities to cope with confronting problems [24, 32]. Both social and cognitive means may have an important impact on general health-related life quality [33]. Concepts and factors influencing quality of life may well differ among individuals, depending on the presence of physical disability [32]. Clinical departments taking care of patients with OI should be able to engage in discussions with the patients about education and worklife and encourage education among OI patients in order to improve HRQoL. The fact that OI predominantly affects HRQoL through the physical domains may indicate that improved medical treatment for the prevention of fractures and attention to skeletal effects of OI may lead to improved HRQoL among adult patients with OI.
The patients in this cohort were classified according to the original Sillence classification [2]. The results did not show differences between patients with mild and moderate OI. The results were not affected if the more recent classification from Dijk et al., 2014 [4] was used comparing patients with ‘common variable OI with normal sclerae’ and ‘non-deforming OI with blue sclerae’ (Data not shown).
Strengths of the present study include its size as it includes more patients than any previous study investigating HRQoL. In addition, the patients are well characterized and genetically confirmed cases of OI. HRQoL is a difficult measure to obtain; however, SF-36 is a well validated and widely used questionnaire. Limitations are that SF-36 is a generalized questionnaire, and therefore not developed to describe patients with skeletal challenges. It does not take recent events into account such as whether the responder has had a recent fracture. Other limitations are that the control group is historical and did not allow sex- and age-matched controls. Further, the control data only enables us to perform one-sided t-tests, increasing the chance of low p-values. However, the p-values in the present study were generally below 0.01 which decreases the risk of false-positive tests at the 0.05 level.
In conclusion, we have investigated the effect of OI and the different types of OI on HRQoL and demonstrated that OI affects physical and to some extent also mental HRQoL. The scores on physical health were correlated to the severity of OI. The mental component score in the OI patients was unaffected and comparable with the average of the general population.
References
Glorieux FH (2008) Osteogenesis imperfecta. Best Pract Res Clin Rheumatol 22:85–100
Sillence DO, Senn A, Danks DM (1979) Genetic heterogeneity in osteogenesis imperfecta. J Med Genet 16:101–116
Folkestad L, Hald JD, Ersboll AK, Gram J, Hermann AP, Langdahl B, Abrahamsen B (2016) Brixen K. A Nationwide Register-Based Cohort Study. J Bone Miner Res, Fracture Rates and Fracture Sites in Patients With Osteogenesis Imperfecta, p 10
van Dijk FS, Sillence DO (2014) Osteogenesis imperfecta: clinical diagnosis, nomenclature and severity assessment. Am J Med Genet A 164A:1470–1481
Chevrel G, Meunier PJ (2001) Osteogenesis imperfecta: lifelong management is imperative and feasible. Joint Bone Spine 68:125–129
Paterson CR, McAllion S, Stellman JL (1984) Osteogenesis imperfecta after the menopause. N Engl J Med 310:1694–1696
Rauch F, Glorieux FH (2004) Osteogenesis imperfecta. Lancet 363:1377–1385
Bishop NJ, Walsh JS (2014) Osteogenesis imperfecta in adults. J Clin Investig 124(2):476
Bishop N (2010) Characterising and treating osteogenesis imperfecta. Early Hum Dev 86:743–746
Balkefors V, Mattsson E, Pernow Y, Saaf M (2013) Functioning and quality of life in adults with mild-to-moderate osteogenesis imperfecta. Physiother Res Int 18:203–211
Wekre LL, Froslie KF, Haugen L, Falch JA (2010) A population-based study of demographical variables and ability to perform activities of daily living in adults with osteogenesis imperfecta. Disabil Rehabil 32:579–587
Staquet M, Hays R, Fayers P (1998) Quality of life assessment in clinical trials; methods and practice. Oxford University Press, Oxford
Widmann RF, Laplaza FJ, Bitan FD, Brooks CE, Root L (2002) Quality of life in osteogenesis imperfecta. Int Orthop 26:3–6
Forestier-Zhang L, Watts L, Turner A, Teare H, Kaye J, Barrett J, Cooper C, Eastell R, Wordsworth P, Javaid MK, Pinedo-Villanueva R (2016) Health-related quality of life and a cost-utility simulation of adults in the UK with osteogenesis imperfecta, X-linked hypophosphatemia and fibrous dysplasia. Orphanet J Rare Dis 11:160
han-Oliel N, Oliel S, Tsimicalis A, Montpetit K, Rauch F, Dogba MJ (2016) Quality of life in osteogenesis imperfecta: A mixed-methods systematic review. Am J Med Genet A 170:62–76
Widmann RF, Bitan FD, Laplaza FJ, Burke SW, DiMaio MF, Schneider R (1999) Spinal deformity, pulmonary compromise, and quality of life in osteogenesis imperfecta. Spine 24:1673–1678
Dogba MJ, Bedos C, Durigova M, Montpetit K, Wong T, Glorieux FH, Rauch F (2013) The impact of severe osteogenesis imperfecta on the lives of young patients and their parents—a qualitative analysis. BMC Pediatr 13:153. doi:10.1186/1471-2431-13-153.:153-13
Rauch F, Lalic L, Roughley P, Glorieux FH (2010) Relationship between genotype and skeletal phenotype in children and adolescents with osteogenesis imperfecta. J Bone Miner Res 25:1367–1374
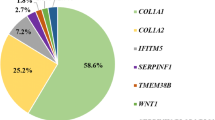
Hald JD, Folkestad L, Harslof T, Lund AM, Duno M, Jensen JB, Neghabat S, Brixen K, Langdahl B (2016) Skeletal phenotypes in adult patients with osteogenesis imperfecta-correlations with COL1A1/COL1A2 genotype and collagen structure. Osteoporos Int 27(11):3331–3341
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. conceptual framework and item selection. Med Care 30:473–483
Ware JE Jr, Kosinski M, Bayliss MS, McHorney CA, Rogers WH, Raczek A (1995) Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the Medical Outcomes Study. Med Care 33:AS264–AS279
Bjorner JB, Thunedborg K, Kristensen TS, Modvig J, Bech P (1998) The Danish SF-36 Health Survey: translation and preliminary validity studies. J Clin Epidemiol 51:991–999
Bjorner JB, Damsgaard MT, Watt T, Groenvold M (1998) Tests of data quality, scaling assumptions, and reliability of the Danish SF-36. J Clin Epidemiol 51:1001–1011
Ablon J (2003) Personality and stereotype in osteogenesis imperfecta: behavioral phenotype or response to life’s hard challenges? Am J Med Genet A 122A:201–214
Reite M, Davis K, Solomons C, Ott J (1972) Osteogenesis imperfecta: psychological function. Am J Psychiatry 128:1540–1546
Ose D, Rochon J, Campbell SM, Wensing M, Freund T, van LJ, Langst G, Szecsenyi J, Ludt S (2014) Health-related quality of life and risk factor control: the importance of educational level in prevention of cardiovascular diseases. Eur J Public Health 24:679–684
de Putter CE, Selles RW, Haagsma JA, Polinder S, Panneman MJ, Hovius SE, Burdorf A, van Beeck EF (2014) Health-related quality of life after upper extremity injuries and predictors for suboptimal outcome. Injury 45(11):1752–1758
Peric’ S, Rakocevic-Stojanovic V, Stevic Z, Basta I, Pavlovic S, Vujanac V, Marjanovic L, Lavrnic D (2010) Health-related quality of life in patients with myotonic dystrophy type 1 and amyotrophic lateral sclerosis. Acta Neurol Belg 110:71–77
Al-Shehri AH, Taha AZ, Bahnassy AA, Salah M (2008) Health-related quality of life in type 2 diabetic patients. Ann Saudi Med 28:352–360
van der Slot WM, Nieuwenhuijsen C, van den Berg-Emons RJ, Wensink-Boonstra AE, Stam HJ, Roebroeck ME (2010) Participation and health-related quality of life in adults with spastic bilateral cerebral palsy and the role of self-efficacy. J Rehabil Med 42:528–535
Bertoletti J, Marx GC, Hattge Junior SP, Pellanda LC (2014) Quality of life and congenital heart disease in childhood and adolescence. Arq Bras Cardiol 102:192–198
Albrecht GL, Devlieger PJ (1999) The disability paradox: high quality of life against all odds. Soc Sci Med 48:977–988
Bandura A (2004) Health promotion by social cognitive means. Health Educ Behav 31:143–164
Acknowledgements
We thank Dorte Haubek and Hans Gjørup for performing dental examinations, Christer Zøylner Swan and Jens Wanscher for performing audiologic evaluations, and Christian-Heinrich Leonhard for performing eye examinations. Grant supporters: Central Region of Denmark, Osteoporoseforeningen, Denmark
Author information
Authors and Affiliations
Contributions
Author Contributions
JDH, TH, and BL designed the study. JDH conducted the study and prepared the first draft of the paper. JDH is responsible for statistical analysis of the data. All authors contributed substantially, revised the paper critically, and approved the final version of the paper. JDH is the guarantor.
Corresponding author
Ethics declarations
Conflict of interest
LF reports having received speaker fees from Genzymes and AstraZeneca. TH reports having received speaker fees from Amgen. BL reports advisory board membership and having received speaking fees from Amgen, Eli Lilly, Merck, and UCB and research support from Eli Lilly, Novo Nordisk, and Orkla Health. KB reports having received grants from MSD, Novartis, Amgen, and NPS. JDH has no interests to declare.
Human and Animal Rights and Informed Consent
The study complied with ethical standards of research involving human participants and was approved by the Danish Ethical Committee (ref-number M-20100108). Informed consent was obtained from all patients.
Rights and permissions
About this article
Cite this article
Hald, J.D., Folkestad, L., Harsløf, T. et al. Health-Related Quality of Life in Adults with Osteogenesis Imperfecta. Calcif Tissue Int 101, 473–478 (2017). https://doi.org/10.1007/s00223-017-0301-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-017-0301-4